Abstract
Purpose
To determine the maximal tolerated doses (MTD) and dose-limiting toxicities (DLT) of combination of 24-h infusions of gemcitabine and irinotecan in patients with advanced solid tumors.
Patients and methods
Twenty-four patients with advanced solid tumors received gemcitabine as a 24-h IV infusion followed by a 24-h infusion of irinotecan every 2 weeks. Pharmacokinetic parameters of both drugs and their metabolites were estimated by using non-compartmental methods.
Results
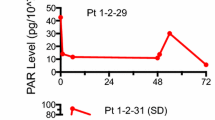
Twenty-four patients were fully evaluable for toxicity. DLT was observed in two of six patients at irinotecan/gemcitabine 110/150 mg/m2 (grade 3 diarrhea and grade 3 GI bleeding). No patient developed acute cholinergic symptoms at any dose. Other toxicities were ≤grade 2 nausea, vomiting, and fatigue. Tumor responses were observed in three patients (one CR: cholangiocarcinoma; two PR: SCLC, gastric neuroendocrine tumor). Stable disease >3 months was found in six patients including five patients who had failed short infusions of either drug. Pharmacokinetic analysis showed that C max of each drug and active metabolites were dose-dependent. High dose of gemcitabine increased C max, AUC, and T1/2 of irinotecan. However, gemcitabine had minimal effects on SN-38.
Conclusions
The recommended dose for Phase II studies is gemcitabine 125 mg/m2 given as a 24-h IV infusion on D1 and D15, followed by a 24-h IV infusion of irinotecan 110 mg/m2 on D2 and D16. Both pretreated patients and chemo-naive patients seem to tolerate higher doses of this combination without significant toxicities. Objective responses among patients with solid tumors, in particular cholangiocarcinoma and small cell lung cancer merits further investigation.



Similar content being viewed by others
References
Hertel LW, Boder GB, Kroin JS et al (1990) Evaluation of the antitumor activity of gemcitabine (2′,2′-difluoro-2′-deoxycytidine). Cancer Res 50:4417–4422
Takimoto CH, Arbuck SA (1996) Camptothecin analogs. In: Chabner BA, Longo DL (eds) Cancer chemotherapy & biotherapy. Principles & practice. Lippincott-Raven Publishers, Philadelphia
Bahadori HR, Rocha Lima CM, Green MR, Safa AR (1999) Synergistic effect of gemcitabine and irinotecan (CPT-11) on breast and small cell lung cancer cell lines. Anticancer Res 19(6B):5423–5428
Rocha Lima CM, Eckardt JR, Leong SS, Sherman CA, Perkel JA, Putman T, Safa AR, Bahadori HR, Green MR (1999) Single-agent gemcitabine and gemcitabine/irinotecan combination (irimogem) in non-small cell lung cancer. Semin Oncol 26(5 Suppl 16):43–50
Rocha Lima CM, Savarese D, Bruckner H, Dudek A et al (2002) Irinotecan plus gemcitabine induce both radiographic and CA 19-9 tumor marker responses in patients with previously untreated advanced pancreatic cancer. J Clin Oncol 20(5):1182–1191
Alberts SR, Erlichman C, Sloan J, Okuno SH, Burch PA, Rubin J, Pitot HC, Goldberg RM, Adjei AA, Atherton PJ, Kaufmann SH (2001) Phase I trial of gemcitabine and CPT-11 given weekly for four weeks every six weeks. Ann Oncol 12(5):627–631
Braakhuis BJM, Ruiz van Haperen VWT et al (1995) Schedule-departmet antitumor effect of gemcitabine in in vivo model systems. Semin Oncol 22(Suppl):42–46
Ruiz van Halperen VWT, Veerman G, Vermorken JB, Peters GJ (1994) Improved antitumor effect of 2′,2′-difluorodeoxycytidine (gemcitabine) in murine colon carcinomas, when administered as continuous infusions. Proc Am Assoc Cancer Res 35:447
Abbruzzese JL, Grunewald R, Weeks EA et al (1991) A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol 9:491–498
Gandhi V, Plunkett W, Du M, Ayres M, Estey E (2000) Prolonged infusion of gemcitabine: clinical and pharmacodynamic studies during a phase I trial in relapsed acute myelogenous leukemia. J Clin Oncol 20(3):665–673
Boven E, Schipper H, Erkelens CAM et al (1993) The influence of the schedule and the dose of gemcitabine on the anti-tumour efficacy in experimental human cancer. Br J Cancer 68:52–56
Grunewald R, Kantajian H, Du M et al (1992) Gemcitabine (2′, 2′ difluorodeoxycytidine) in leukemia: a phase I clinical, plasma and celluler pharmacology study. J Clin Oncol 10:406–413
Tempero M, Plunkett W, Ruiz van Haperen V, Hainsworth J, Hochster H, Lenzi R, Abbruzzese J (2003) Randomized phase II comparison of dose-intense gemcitabine: thirty-minute infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J Clin Oncol 21(18):3402–3408
von Delius S, Lersch C, Schulte-Frohlinde E, Mayr M, Schmid RM, Eckel F (2005) Phase II trial of weekly 24-hour infusion of gemcitabine in patients with advanced gallbladder and biliary tract carcinoma. BMC Cancer 5(1):61
Takimoto CH, Morrison G, Harold N et al (2000) A phase I & pharmacologic study of irinotecan administered as a 96-hour infusion weekly to adult cancer patients. J Clin Oncol 18:659–667
Herben VMM, Schellens JHM, Swart M et al (1999) Phase I & pharmacokinetic study of irinotecan administered as a low-dose, continuous infusion over 14 days in patients with solid tumors. J Clin Oncol 17:1897–1905
Haaz MC, Rivory LP, Riche C et al (1997) The transformation of irinotecan (CPT-11) to its active metabolite SN-38 by human liver microsomes: differential hydrolysis for the lactone and carboxylate forms. Naunyn Schmiedebergs Arch Pharmacol 356:257–262
Slatter JG, Su P, Sams JP et al (1998) Bioactivation of the anticancer agent CPT-11 to SN-38 by human hepatic microsomal carboxylesterases and the in vitro assessement of potential drug interactions. Drug Metab Dispos 25:1157–1164
Gupta E, Lestingi TM, Mick R et al (1994) Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res 54:3723-3725
Yamazaki H, Funakoshi S, Hirano A et al. (1999) Phase I & pharmacokinetic study of irinotecan (CPT-11) given by 24 hours infusion plus oral uracil/tegafur (UFT) in patients with lung cancer. Proc Am Soc Clin Oncol 18: abstr 2036
Salman HS, Tanaka K, Sparano JA (2000) Phase I/II trial of gemcitabine plus cyclophosphamide in patients with metastatic breast carcinoma previously treated with taxanes. Clin Breast Cancer 2(4):299–303
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Keith B, Xu Y, Grem JL (2003) Measurement of the anti-cancer agent gemcitabine in human plasma by high-performance liquid chromatography. J Chromatogr B Analyt Technol Biomed Life Sci 785(1):65–72
Yilmaz B, Kadioglu Y (2004) Comparison of zero- and second-order derivative spectrophotometric and HPLC methods for the determination of gemcitabine in human plasma. Farmaco 59(5):425–429
Rivory LP, Chatelut E, Canal P, Mathieu-Boue A, Robert J (1994) Kinetics of the in vivo interconversion of the carboxylate and lactone forms of irinotecan (CPT-11) and of its metabolite SN-38 in patients. Cancer Res 54:6330–6333
Rivory LP, Bowles MR, Robert J, Pond SM (1996) Conversion of irinotecan (CPT-11) to its active metabolite, 7-ethyl-10-hydroxycamptothecin (SN-38) by human liver carboxylesterase. Biochem Pharmcol 52:1103–1111
Wang H, Wang S, Nan L, Yu D, Agrawal S, Zhang R (2002) Antisense anti-MDM2 mixed-backbone oligonucleotides enhance therapeutic efficacy of topoisomerase I inhibitor irinotecan in nude mice bearing human cancer xenografts: In vivo activity and mechanisms. Int J Oncol 20:745–752
Wright MA, Morrison G, Lin P et al. (2005) A phase I pharmacologic and pharmacogenetic trial of sequential 24-hour infusion of irinotecan followed by leucovorin and a 48-hour infusion of fluorouracil in adult patients with solid tumors. Clin Cancer Res 11(11):4144–4150
Piantadosi S (1997) Clinical trials: a methodologic perspective. Wiley, New York, pp 151–155
Saif MW, Sellers S, Russo S (2006) Gemcitabine-related radiation recall in a patient with pancreatic cancer. Anticancer Drugs 17(1):107–111
Ulrich-Pur H, Kornek GV, Fiebiger W, Schull B, Raderer M, Scheithauer W (2001) Treatment of advanced hepatocellular carcinoma with biweekly high-dose gemcitabine. Oncology 60(4):313–315
Penz M, Kornek GV, Raderer M, Ulrich-Pur H, Fiebiger W, Lenauer A, Depisch D, Krauss G, Schneeweiss B, Scheithauer W (2001) Phase II trial of two-weekly gemcitabine in patients with advanced biliary tract cancer. Ann Oncol 12(2):183–186
Fuchs CS, Moore MR, Harker G, Villa L, Rinaldi D, Hecht JR (2003) Phase III comparison of two irinotecan dosing regimens in second-line therapy of metastatic colorectal cancer. J Clin Oncol 21(5):807–814
Saltz LB, Cox JV, Blanke C et al (2000) Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. N Engl J Med 343:905–914
Burris HA III, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P, Nelson R, Dorr FA, Stephens CD, Von Hoff DD (1997) Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 15(6):2403–2413
Stewart DF, Ma M, Furman WL et al (1998) Pharmocokinetics of inrinotecan and its active metabolite SN-38 in children with recurrent solid tumors after protracted low dose IV irinotecan. Proc Am Soc Clin Oncol 17:186a
Slatter JG, Schaaf LJ, Sams JP, Feenstra KL, Johnson MG, Bombardt PA, Cathcart KS, Verburg MT, Pearson LK, Compton LD, Miller LL, Baker DS, Pesheck CV, Lord RS (2000) Pharmacokinetics, metabolism and excretion of irinotecan (CPT-11) following I.V. infusion of [14C] CPT-11 in cancer patients. Drug Metab Dispos 28:423–433
Mathijssen RHJ, Loos WJ, Verweij J, Sparreboom A (2002) Pharmacology of topoisomerase I inhibitors irinotecan (CPT-11) and topotecan. Curr Cancer Drug Target 2:103–123
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was approved and funded by the National Comprehensive Cancer Network (NCCN) from general research support provided by Pfizer, Inc.
Rights and permissions
About this article
Cite this article
Saif, M.W., Sellers, S., Li, M. et al. A phase I study of bi-weekly administration of 24-h gemcitabine followed by 24-h irinotecan in patients with solid tumors. Cancer Chemother Pharmacol 60, 871–882 (2007). https://doi.org/10.1007/s00280-007-0434-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0434-7