Abstract
Purpose
The purpose of this study was to evaluate pre-operative education versus no education and mini-invasive surgery versus standard surgery to reach complete independence.
Methods
We conducted a four-arm randomized controlled trial of 209 patients. The primary outcome criterion was the time to reach complete functional independence. Secondary outcomes included the operative time, the estimated total blood loss, the pain level, the dose of morphine, and the time to discharge.
Results
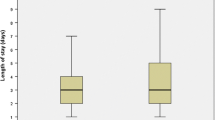
There was no significant effect of either education (HR: 1.1; P = 0.77) or mini-invasive surgery (HR: 1.0; 95 %; P = 0.96) on the time to reach complete independence. The mini-invasive surgery group significantly reduced the total estimated blood loss (P = 0.0035) and decreased the dose of morphine necessary for titration in the recovery (P = 0.035).
Conclusions
Neither pre-operative education nor mini-invasive surgery reduces the time to reach complete functional independence. Mini-invasive surgery significantly reduces blood loss and the need for morphine consumption.


Similar content being viewed by others
References
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370(9597):1508–1519
Haute Autorité de Santé (2007) Evaluation des prothèses de hanche. Saint-Denis La Plaine. www.has-sante.fr/portail/upload/docs/application/pdf/rapport_evaluation_des_protheses_de_hanche.pdf. Accessed 30 March 2015
Berry DJ, Harmsen WS, Cabanela ME, Morrey BF (2002) Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am 84-A(2):171–177
Ibrahim MS, Twaij H, Giebaly DE, Nizam I, Haddad FS (2013) Enhanced recovery in total hip replacement: a clinical review. Bone Joint J 95-B(12):1587–1594
Xu CP, Li X, Song JQ, Cui Z, Yu B (2013) Mini-incision versus standard incision total hip arthroplasty regarding surgical outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE 8(11):e80021
McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A (2014) Preoperative education for hip or knee replacement. Cochrane Database Syst Rev 5:CD003526
Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ (2012) Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res 470(2):490–496
Maradit Kremers H, Visscher SL, Kremers WK, Naessens JM, Lewallen DG (2014) Obesity increases length of stay and direct medical costs in total hip arthroplasty. Clin Orthop Relat Res 472(4):1232–1239
Vasarhelyi EM, MacDonald SJ (2012) The influence of obesity on total joint arthroplasty. J Bone Joint Surg (Br) 94(11 Suppl A):100–102
Nezry N, Jeanrot C, Vinh TS, Ganz R, Tomeno B, Anract P (2000) Partial anterior trochanteric osteotomy in total hip arthroplasty: surgical technique and preliminary results of 127 cases. J Arthroplasty 18(3):333–337
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58(3):277–280
Schoenfeld DA (1983) Sample-size formula for the proportional-hazards regression model. Biometrics 39(2):499–503
Gail M, Simon R (1985) Testing for qualitative interactions between treatment effects and patient subsets. Biometrics 41(2):361–372
Crowe J, Henderson J (2003) Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther 70(2):88–96
Gocen Z, Sen A, Unver B, Karatosun V, Gunal I (2004) The effect of preoperative physiotherapy and education on the outcome of total hip replacement: a prospective randomized controlled trial. Clin Rehabil 18(4):353–358
Vukomanovi A, Popovi Z, Durovi A, Krsti L (2008) The effects of short-termp reoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl 65(4):291–297
Giraudet-Le Quintrec JS, Coste J, Vastel L, Pacault V, Jeanne L, Lamas JP, Kerboull L, Fougeray M, Conseiller C, Kahan A, Courpied JP (2003) Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat Res 414:112–120
Sherry E, Egan M, Henderson A, Warnke PH (2002) Minimally invasive techniques for total hip arthroplasty. J Bone Joint Surg Am 84-A(8):1481, author reply 1481–2
Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP (2005) Minimally invasive total hip arthroplasty. A prospective randomized study. J Arthroplasty 20(2):139–144
Musil D, Stehlík J, Verner M (2008) A comparison of operative invasiveness in minimally invasive anterolateral hip replacement (MIS-AL) and standard hip procedure, using biochemical markers. Acta Chir Orthop Traumatol Cech 75(1):16–20
Acknowledgments
This research was funded by the Programme Hospitalier de Recherche Clinique 2005 (DRCD P051040).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Biau, D.J., Porcher, R., Roren, A. et al. Neither pre-operative education or a minimally invasive procedure have any influence on the recovery time after total hip replacement. International Orthopaedics (SICOT) 39, 1475–1481 (2015). https://doi.org/10.1007/s00264-015-2802-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2802-y