Abstract
Purpose
The extent to which days’ supply data are missing in pharmacoepidemiologic databases and effective methods for estimation is unknown. We determined the percentage of missing days’ supply on prescription and patient levels for oral anti-diabetic drugs (OADs) and evaluated three methods for estimating days’ supply within the Clinical Practice Research Datalink (CPRD) and The Health Improvement Network (THIN).
Methods
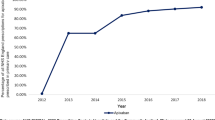
We estimated the percentage of OAD prescriptions and patients with missing days’ supply in each database from 2009 to 2013. Within a random sample of prescriptions with known days’ supply, we measured the accuracy of three methods to estimate missing days’ supply by imputing the following: (1) 28 days’ supply, (2) mode number of tablets/day by drug strength and number of tablets/prescription, and (3) number of tablets/day via a machine learning algorithm. We determined incidence rates (IRs) of acute myocardial infarction (AMI) using each method to evaluate the impact on ascertainment of exposure time and outcomes.
Results
Days’ supply was missing for 24 % of OAD prescriptions in CPRD and 33 % in THIN (affecting 48 and 57 % of patients, respectively). Methods 2 and 3 were very accurate in estimating days’ supply for OADs prescribed at a consistent number of tablets/day. Method 3 was more accurate for OADs prescribed at varying number of tablets/day. IRs of AMI were similar across methods for most OADs.
Conclusions
Missing days’ supply is a substantial problem in both databases. Method 2 is easy and very accurate for most OADs and results in IRs comparable to those from method 3.

Similar content being viewed by others
References
Gore M, Brix Finnerup N, Sadosky A et al (2013) Pain-related pharmacotherapy, healthcare resource use and costs in spinal cord injury patients prescribed pregabalin. Spinal Cord 51:126–133. doi:10.1038/sc.2012.97
Petersen I, McCrea RL, Sammon CJ et al (2016) Risks and benefits of psychotropic medication in pregnancy: cohort studies based on UK electronic primary care health records. Health Technol Assess 20:1–176. doi:10.3310/hta20230
Mamtani R, Haynes K, Bilker WB et al (2012) Association between longer therapy with thiazolidinediones and risk of bladder cancer: a cohort study. JNCI J Natl Cancer Inst 104:1411–1421. doi:10.1093/jnci/djs328
Cea Soriano L, Bateman BT, García Rodríguez LA, Hernández-Díaz S (2014) Prescription of antihypertensive medications during pregnancy in the UK. Pharmacoepidemiol Drug Saf 23:1051–1058. doi:10.1002/pds.3641
Margulis AV, Abou-Ali A, Strazzeri MM et al (2013) Use of selective serotonin reuptake inhibitors in pregnancy and cardiac malformations: a propensity-score matched cohort in CPRD. Pharmacoepidemiol Drug Saf 22:942–951. doi:10.1002/pds.3462
Price D, Thomas M, Haughney J et al (2013) Real-life comparison of beclometasone dipropionate as an extrafine- or larger-particle formulation for asthma. Respir Med 107:987–1000. doi:10.1016/j.rmed.2013.03.009
Farris KB, Kaplan B, Kirking DM (1994) Examination of days supply in computerized prescription claims. J Pharmacoepidemiol 3:63–76
Shah AD, Martinez C (2006) An algorithm to derive a numerical daily dose from unstructured text dosage instructions. Pharmacoepidemiol Drug Saf 15:161–166. doi:10.1002/pds.1151
World Health Organisation Collaborating Centre for Drug Statistics Methodology. (2016) ATC classification index with DDDs. http://www.whocc.no/atc_ddd_publications/atc_ddd_index/.
Sinnott S-J, Polinski JM, Byrne S, Gagne JJ (2016) Measuring drug exposure: concordance between defined daily dose and days’ supply depended on drug class. J Clin Epidemiol 69:107–113. doi:10.1016/j.jclinepi.2015.05.026
Carbonari DM, Saine ME, Newcomb CW et al (2015) Use of demographic and pharmacy data to identify patients included within both the Clinical Practice Research Datalink (CPRD) and The Health Improvement Network (THIN). Pharmacoepidemiol Drug Saf 24:999–1003. doi:10.1002/pds.3844
Gibson J (2012) Enhanced dosage determinations. CSD Med. Res, UK
Hastie T, Tibshirani R, Friedman JH (2009) The elements of statistical learning: data mining, inference, and prediction, 2nd edn. Springer, New York, NY
A practical guide to SVM classification. (2016) In: LIBSVM-- Libr. Support Vector Mach. https://www.csie.ntu.edu.tw/~cjlin/libsvm/.
Japkowicz N, Shah M (2014) Evaluating learning algorithms: a classification perspective. Cambridge University Press, New York
Hammad TA, McAdams MA, Feight A et al (2008) Determining the predictive value of Read/OXMIS codes to identify incident acute myocardial infarction in the General Practice Research Database. Pharmacoepidemiol Drug Saf 17:1197–1201. doi:10.1002/pds.1672
Gross R, Bilker WB, Strom BL, Hennessy S (2008) Validity and comparison of two measures of days supply in Medicaid claims data. Pharmacoepidemiol Drug Saf 17:1029–1032. doi:10.1002/pds.1606
Acknowledgments
This study was sponsored by AstraZeneca.
Authors’ contributions
All authors contributed to the research and development of new methods. AMG and HB provided expertise on Clinical Practice Research Datalink and The Health Improvement Network, respectively. KJL and CWN were responsible for data analysis. All authors interpreted the results of analyses. KJL drafted the manuscript and all authors contributed with critical revision of the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the UK Independent Scientific Advisory Committees for CPRD (Protocol 10_149RMn) and THIN (Protocol 11-039V) and the Institutional Review Board of the University of Pennsylvania. Informed consent of participants was not required.
Conflict of interest
This study was funded by AstraZeneca and KJL, CWN, JAR, DMC, MES, SC, and VLR received funding from AstraZeneca through their employers. AMG and HB are representatives from Clinical Practice Research Datalink and The Health Improvement Network, respectively. Authors report no other relevant potential conflicts of interest related to this manuscript.
Electronic supplementary material
ESM 1
(DOCX 62 kb)
Rights and permissions
About this article
Cite this article
Lum, K.J., Newcomb, C.W., Roy, J.A. et al. Evaluation of methods to estimate missing days’ supply within pharmacy data of the Clinical Practice Research Datalink (CPRD) and The Health Improvement Network (THIN). Eur J Clin Pharmacol 73, 115–123 (2017). https://doi.org/10.1007/s00228-016-2148-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2148-4