Abstract
Rationale
Due to the episodic and chronic nature of bipolar disorder (BD), maintenance therapy represents a critical part of treatment; however, there is a paucity of studies comparing effectiveness of available long-term treatments.
Objective
The aim of this study is to determine and compare the efficacy of pharmacological treatments for maintenance treatment of BD by means of the number needed to treat (NNT).
Methods
The efficacy of drugs used for maintenance treatment of BD, as emerging from the results of randomized controlled trials, was assessed using the size effect measure of NNT. PubMed searches were conducted on English-language articles published until May 2010 using the search terms “bipolar disorder,” “mania,” “mixed episode,” or “bipolar depression,” cross-referenced with trial characteristic search phrases and generic names of medications. The search was supplemented by manually reviewing reference lists from identified publications.
Results
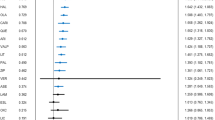
In 15 studies, aripiprazole, olanzapine, quetiapine, risperidone long-acting injection, lithium, lamotrigine, and divalproex proved effectiveness in terms of NNTs (≥10% advantage over placebo) for prevention of relapse into any mood episode. Quetiapine, lithium, risperidone long-acting injection, aripiprazole, and olanzapine are effective in manic recurrence prevention. Lamotrigine, quetiapine, and lithium present significant NNTs for prevention of depressive relapses.
Conclusions
All of the pharmacological agents assessed were effective in the prevention of any kind of mood episode; however, different efficacy profiles were found for prevention of manic and/or depressive relapses. The comparison of NNT values of the available agents may represent a useful tool in clinical settings, in order to facilitate implementation of long-term pharmacological interventions in patients with BD.


Similar content being viewed by others
References
Altman DG (1998) Confidence intervals for the number needed to treat. BMJ 317:1309–1312
Altman DG, Deeks JJ (2002) Meta-analysis, Simpson’s paradox, and the number needed to treat. BMC Med Res Methodol 2:3
Bowden CL, Calabrese JR, McElroy SL, Gyulai L, Wassef A, Petty F, Pope HG Jr, Chou JC, Keck PE Jr, Rhodes LJ, Swann AC, Hirschfeld RM, Wozniak PJ (2000) A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 57:481–489
Bowden CL, Calabrese JR, Sachs G, Yatham LN, Asghar SA, Hompland M, Montgomery P, Earl N, Smoot TM, DeVeaugh-Geiss J, Lamictal 606 Study Group (2003) A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry 60:392–400
Bowden CL, Vieta E, Ice KS, Schwartz JH, Wang PP, Versavel M (2010) Ziprasidone plus a mood stabilizer in subjects with bipolar I disorder: a 6-month, randomized, placebo-controlled, double-blind trial. J Clin Psychiatry 71:130–137
Calabrese JR, Suppes T, Bowden CL, Sachs GS, Swann AC, McElroy SL, Kusumakar V, Ascher JA, Earl NL, Greene PL, Monaghan ET, Lamictal 614 Study Group (2000) A double-blind, placebo-controlled, prophylaxis study of lamotrigine in rapid-cycling bipolar disorder. J Clin Psychiatry 61:841–850
Calabrese JR, Bowden CL, Sachs G, Yatham LN, Behnke K, Mehtonen OP, Montgomery P, Ascher J, Paska W, Earl N, DeVeaugh-Geiss J, Lamictal 605 Study Group (2003) A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 64:1013–1024
Calabrese JR, Vieta E, El-Mallakh R, Findling RL, Youngstrom EA, Elhaj O, Gajwani P, Pies R (2004) Mood state at study entry as predictor of the polarity of relapse in bipolar disorder. Biol Psychiatry 56:957–963
Calabrese JR, Goldberg JF, Ketter TA, Suppes T, Frye M, White R, DeVeaugh-Geiss A, Thompson TR (2006) Recurrence in bipolar I disorder: a post hoc analysis excluding relapses in two double-blind maintenance studies. Biol Psychiatry 59:1061–1064
Citrome L (2008) Compelling or irrelevant? Using number needed to treat can help decide. Acta Psychiatr Scand 117:412–419
Colom F, Vieta E, Daban C, Pacchiarotti I, Sánchez-Moreno J (2006) Clinical and therapeutic implications of predominant polarity in bipolar disorder. J Affect Disord 93:13–17
Cook RJ, Sackett DL (1995) The number needed to treat: a clinically useful measure of treatment effect. BMJ 310:452–454
Coryell W (2009) Maintenance treatment in bipolar disorder: a reassessment of lithium as the first choice. Bipolar Disord 11(Suppl 2):77–83
Goodwin GM, Bowden CL, Calabrese JR, Grunze H, Kasper S, White R, Greene P, Leadbetter R (2004) A pooled analysis of 2 placebo-controlled 18-month trials of lamotrigine and lithium maintenance in bipolar I disorder. J Clin Psychiatry 65:432–441
Goodwin GM, Anderson I, Arango C, Bowden CL, Henry C, Mitchell PB, Nolen WA, Vieta E, Wittchen HU (2008) ECNP consensus meeting. Bipolar depression. Nice, March (2007). Eur Neuropsychopharmacol 18:535–549
Gray G (2004) Concise guide to evidence-based psychiatry. American Psychiatric Publishing Inc, Washington, DC, pp 67–68
Keck PE Jr, Calabrese JR, McIntyre RS, McQuade RD, Carson WH, Eudicone JM, Carlson BX, Marcus RN, Sanchez R, Aripiprazole Study Group (2007) Aripiprazole monotherapy for maintenance therapy in bipolar I disorder: a 100-week, double-blind study versus placebo. J Clin Psychiatry 68:1480–1491
Kraemer HC, Kupfer DJ (2006) Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry 59:990–996
Macfadden W, Alphs L, Haskins JT, Turner N, Turkoz I, Bossie C, Kujawa M, Mahmoud R (2009) A randomized, double-blind, placebo-controlled study of maintenance treatment with adjunctive risperidone long-acting therapy in patients with bipolar I disorder who relapse frequently. Bipolar Disord 11:827–839
Martinez-Aran A, Vieta E, Chengappa KN, Gershon S, Mullen J, Paulsson B (2008) Reporting outcomes in clinical trials for bipolar disorder: a commentary and suggestions for change. Bipolar Disord 10:566–579
Perlis RH, Ostacher MJ, Patel JK, Marangell LB, Zhang H, Wisniewski SR, Ketter TA, Miklowitz DJ, Otto MW, Gyulai L, Reilly-Harrington NA, Nierenberg AA, Sachs GS, Thase ME (2006) Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry 163:217–224
Prien RF, Caffey EM Jr, Klett CJ (1973) Prophylactic efficacy of lithium carbonate in manic–depressive illness. Report of the Veterans Administration and National Institute of Mental Health Collaborative Study Group. Arch Gen Psychiatry 28:337–341
Quiroz JA, Yatham LN, Palumbo JM, Karcher K, Kushner S, Kusumakar V (2010) Risperidone long-acting injectable monotherapy in the maintenance treatment of bipolar I disorder. Biol Psychiatry 68:156–162
Richy F, Ethgen O, Bruyere O, Deceulaer F, et al. (2004) From sample size to effect-size: small study effect investigation (SSEi). The Internet Journal of Epidemiology 1
Suppes T, Vieta E, Liu S, Brecher M, Paulsson B (2009) Maintenance treatment for patients with bipolar I disorder: results from a North American study of quetiapine in combination with lithium or divalproex (trial 127). Am J Psychiatry 166:476–488
Thase ME (2008) Selecting appropriate treatments for maintenance therapy for bipolar disorder. J Clin Psychiatry 69(5):28–35
Tohen M, Chengappa KN, Suppes T, Baker RW, Zarate CA, Bowden CL, Sachs GS, Kupfer DJ, Ghaemi SN, Feldman PD, Risser RC, Evans AR, Calabrese JR (2004) Relapse prevention in bipolar I disorder: 18-month comparison of olanzapine plus mood stabiliser v. mood stabiliser alone. Br J Psychiatry 184:337–345
Tohen M, Calabrese JR, Sachs GS, Banov MD, Detke HC, Risser R, Baker RW, Chou JC, Bowden CL (2006) Randomized, placebo-controlled trial of olanzapine as maintenance therapy in patients with bipolar I disorder responding to acute treatment with olanzapine. Am J Psychiatry 163:247–256
Vieta E, Berk M, Wang W, Colom F, Tohen M, Baldessarini RJ (2009) Predominant previous polarity as an outcome predictor in a controlled treatment trial for depression in bipolar I disorder patients. J Affect Disord 119:22–27
Vieta E, Cruz N, García-Campayo J, de Arce R, Manuel Crespo J, Vallès V, Pérez-Blanco J, Roca E, Manuel Olivares J, Moríñigo A, Fernández-Villamor R, Comes M (2008a) A double-blind, randomized, placebo-controlled prophylaxis trial of oxcarbazepine as adjunctive treatment to lithium in the long-term treatment of bipolar I and II disorder. Int J Neuropsychopharmacol 11:445–452
Vieta E, Suppes T, Eggens I, Persson I, Paulsson B, Brecher M (2008b) Efficacy and safety of quetiapine in combination with lithium or divalproex for maintenance of patients with bipolar I disorder (international trial 126). J Affect Disord 109:251–263
Weisler RH, Nolen WA, Neijber A, Hellqvist A, Paulsson B (2008). Quetiapine or lithium versus placebo for maintenance treatment of bipolar I disorder after stabilization on quetiapine. Presented at the 60th Institute on Psychiatric Services Congress, Chicago, IL, 2–5 October 2008
Yatham LN, Kennedy SH, Schaffer A, Parikh SV, Beaulieu S, O’Donovan C, MacQueen G, McIntyre RS, Sharma V, Ravindran A, Young LT, Young AH, Alda M, Milev R, Vieta E, Calabrese JR, Berk M, Ha K, Kapczinski F (2009) Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disord 11:225–255
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Popovic, D., Reinares, M., Amann, B. et al. Number needed to treat analyses of drugs used for maintenance treatment of bipolar disorder. Psychopharmacology 213, 657–667 (2011). https://doi.org/10.1007/s00213-010-2056-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-010-2056-8