Abstract
Summary
This study of elderly Swedish women investigated the association between chronic vitamin D insufficiency and osteoporotic fractures occurring between ages 80–90. The incidence and risk of hip and major osteoporotic fractures was significantly higher in elderly women with low vitamin D levels maintained over 5 years.
Introduction
Vitamin D insufficiency among the elderly is common; however, relatively little is known about the effects of long-term hypovitaminosis D on fracture. We investigated sequential assessment of serum 25(OH)D at age 75 and 80 to determine if continuously low 25(OH)D levels are associated with increased 10-year fracture incidence.
Methods
One thousand forty-four Swedish women from the population-based OPRA cohort, all 75 years old, attended at baseline (BL); 715 attended at 5 years. S-25(OH)D was available in 987 and 640, respectively and categorized as: <50 (Low), 50–75 (Intermediate), and >75 nmol/L (High). Incident fracture data was collected with maximum follow-up to 90 years of age.
Results
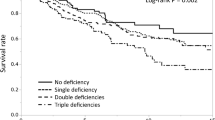
Hip fracture incidence between age 80–85 was higher in women who had low 25(OH)D at both baseline and 5 years (22.2 % (Low) vs. 6.6 % (High); p = 0.003). Between age 80–90, hip fracture incidence was more than double that of women in the high category (27.9 vs. 12.3 %; p = 0.006). Within 5-years, 50 % of women in the continuously low group compared to 34 % in the continuously high 25(OH)D group had an osteoporotic fracture (p = 0.004) while 10-year incidence was higher compared to the intermediate (p = 0.020) but not the high category (p = 0.053). The 10-year relative risk of hip fracture was almost three times higher and osteoporotic fracture risk almost doubled for women in the lowest 25(OH)D category compared to the high category (HR 2.7 and 1.7; p = 0.003 and 0.023, respectively).
Conclusion
In these elderly women, 25(OH)D insufficiency over 5-years was associated with increased 10-year risk of hip and major osteoporotic fractures.



Similar content being viewed by others
References
Cranney A, Horsley T, O'Donnell S, Weiler H, Puil L, et al (2007) Effectiveness and safety of vitamin D in relation to bone health. Evid Rep Technol Assess (Full Rep): 1–235
Nuti R, Martini G, Valenti R, Gambera D, Gennari L, Salvadori S, Avanzati A (2004) Vitamin D status and bone turnover in women with acute hip fracture. Clin Orthop Relat Res: 208–213
Sakuma M, Endo N, Oinuma T (2007) Serum 25-OHD insufficiency as a risk factor for hip fracture. J Bone Miner Metab 25:147–150
Reid IR, Bolland MJ, Grey A (2013) Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet 383:146–155
Bryson DJ, Nichols JS, Ford AJ, Williams SC (2013) The incidence of vitamin D deficiency amongst patients with a femoral neck fracture: are current bone protection guidelines sufficient? Acta Orthop Belg 79:470–473
Seitz S, Koehne T, Ries C, De Novo OA, Barvencik F et al (2013) Impaired bone mineralization accompanied by low vitamin D and secondary hyperparathyroidism in patients with femoral neck fracture. Osteoporos Int 24:641–649
Maier S, Sidelnikov E, Dawson-Hughes B, Egli A, Theiler R et al (2013) Before and after hip fracture, vitamin D deficiency may not be treated sufficiently. Osteoporos Int 24:2765–2773
Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ et al (2012) A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 367:40–49
Izaks GJ (2007) Fracture prevention with vitamin D supplementation: considering the inconsistent results. BMC Musculoskelet Disord 8:26
Abrahamsen B, Masud T, Avenell A, Anderson F, Meyer HE, Cooper C, Smith H, LaCroix AZ, Torgerson D, Jackson R, Rejnmark L, Wactawski-Wende J, Brixen K, Mosekilde L, Robbins JA, Francis RM (2010) Patient level pooled analysis of 68 500 patients from seven major vitamin D fracture trials in US and Europe. BMJ 340:b5463
Bergman GJ, Fan T, McFetridge JT, Sen SS (2010) Efficacy of vitamin D3 supplementation in preventing fractures in elderly women: a meta-analysis. Curr Med Res Opin 26:1193–1201
Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS et al (2005) Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet 365:1621–1628
Larsen ER, Mosekilde L, Foldspang A (2004) Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res 19:370–378
Rizzoli R, Boonen S, Brandi ML, Bruyere O, Cooper C et al (2013) Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin 29:305–313
Lai JK, Lucas RM, Clements MS, Roddam AW, Banks E (2010) Hip fracture risk in relation to vitamin D supplementation and serum 25-hydroxyvitamin D levels: a systematic review and meta-analysis of randomised controlled trials and observational studies. BMC Public Health 10:331
Snellman G, Melhus H, Gedeborg R, Byberg L, Berglund L, Wernroth L, Michaelsson K (2010) Determining vitamin D status: a comparison between commercially available assays. PLoS ONE 5:e11555
Dawson-Hughes B, Harris SS (2010) High-dose vitamin D supplementation: too much of a good thing? JAMA 303:1861–1862
Snellman G, Byberg L, Lemming EW, Melhus H, Gedeborg R et al (2013) Long-term dietary vitamin D intake and risk of fracture and osteoporosis: a longitudinal cohort study of Swedish middle-aged and elderly women. J Clin Endocrinol Metab 99:781–790
Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, Dawson-Hughes B (2004) Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr 80:752–758
Campbell PM, Allain TJ (2006) Muscle strength and vitamin D in older people. Gerontology 52:335–338
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA et al (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Gerdhem P, Ringsberg KA, Obrant KJ, Akesson K (2005) Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA Study of Elderly Women. Osteoporos Int 16:1425–1431
Holvik K, Ahmed LA, Forsmo S, Gjesdal CG, Grimnes G et al (2013) Low serum levels of 25-hydroxyvitamin D predict hip fracture in the elderly. A NOREPOS study. J Clin Endocrinol Metab 98:3341–3350
Ivaska KK, Gerdhem P, Vaananen HK, Akesson K, Obrant KJ (2010) Bone turnover markers and prediction of fracture: a prospective follow-up study of 1040 elderly women for a mean of 9 years. J Bone Miner Res 25:393–403
Sakuma M, Endo N, Oinuma T, Hayami T, Endo E et al (2006) Vitamin D and intact PTH status in patients with hip fracture. Osteoporos Int 17:1608–1614
Bakhtiyarova S, Lesnyak O, Kyznesova N, Blankenstein MA, Lips P (2006) Vitamin D status among patients with hip fracture and elderly control subjects in Yekaterinburg, Russia. Osteoporos Int 17:441–446
Bischoff-Ferrari HA, Can U, Staehelin HB, Platz A, Henschkowski J et al (2008) Severe vitamin D deficiency in Swiss hip fracture patients. Bone 42:597–602
Khadgawat R, Brar KS, Gahlo M, Yadav CS, Malhotra R, Guptat N, Tandon N (2010) High prevalence of vitamin D deficiency in Asian-Indian patients with fragility hip fracture: a pilot study. J Assoc Physicians India 58:539–542
Gerdhem P, Brandstrom H, Stiger F, Obrant K, Melhus H et al (2004) Association of the collagen type 1 (COL1A 1) Sp1 binding site polymorphism to femoral neck bone mineral density and wrist fracture in 1044 elderly Swedish women. Calcif Tissue Int 74:264–269
Ahn J, Peters U, Albanes D, Purdue MP, Abnet CC et al (2008) Serum vitamin D concentration and prostate cancer risk: a nested case–control study. J Natl Cancer Inst 100:796–804
Jonsson B, Gardsell P, Johnell O, Redlund-Johnell I, Sernbo I (1994) Remembering fractures: fracture registration and proband recall in southern Sweden. J Epidemiol Community Health 48:489–490
Gerdhem P, Akesson K (2007) Rates of fracture in participants and non-participants in the Osteoporosis Prospective Risk Assessment study. J Bone Joint Surg (Br) 89:1627–1631
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Ross AC, Taylor CL, Yaktine AL, Del Valle HB (eds) (2011) Dietary Reference Intakes for Calcium and Vitamin D. National Academy of Sciences, Washington
Melhus H, Snellman G, Gedeborg R, Byberg L, Berglund L et al (2010) Plasma 25-hydroxyvitamin D levels and fracture risk in a community-based cohort of elderly men in Sweden. J Clin Endocrinol Metab 95:2637–2645
Looker AC (2013) Serum 25-hydroxyvitamin D and risk of major osteoporotic fractures in older U.S. adults. J Bone Miner Res 28:997–1006
Cauley JA, Danielson ME, Boudreau R, Barbour KE, Horwitz MJ et al (2011) Serum 25-hydroxyvitamin D and clinical fracture risk in a multiethnic cohort of women: The women's health initiative (WHI). J Bone Miner Res 26:2378–2388
Kanis JA, McCloskey EV, Johansson H, Oden A, Strom O, Borgstrom F (2010) Development and use of FRAX in osteoporosis. Osteoporos Int 21(Suppl 2):S407–S413
(1997) Dietary reference intakes. Nutr Rev 55: 319–326.
Sigurdsson G, Franzson L, Steingrimsdottir L, Sigvaldason H (2000) The association between parathyroid hormone, vitamin D and bone mineral density in 70-year-old Icelandic women. Osteoporos Int 11:1031–1035
Chapuy MC, Schott AM, Garnero P, Hans D, Delmas PD, Meunier PJ (1996) Healthy elderly French women living at home have secondary hyperparathyroidism and high bone turnover in winter. EPIDOS Study Group. J Clin Endocrinol Metab 81:1129–1133
Holick MF, Siris ES, Binkley N, Beard MK, Khan A et al (2005) Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab 90:3215–3224
Bischoff-Ferrari HA, Shao A, Dawson-Hughes B, Hathcock J, Giovannucci E, Willett WC (2010) Benefit-risk assessment of vitamin D supplementation. Osteoporos Int 21:1121–1132
Wihlborg A, Akesson K, Gerdhem P (2014) External validity of a population-based study on osteoporosis and fracture. Acta Orthop 85:1–5
Acknowledgments
Thanks are extended to the research nurses at the Clinical and Molecular Osteoporosis Research Unit, Malmö and to all the women who kindly participated in the study.
This work was supported by grants from the Swedish Research Council (K2012-52X-14691-10-3), FAS (2007–2125), Greta and Johan Kock Foundation, A. Påhlsson Foundation, A. Osterlund Foundation, the H Järnhardt foundation, King Gustav V and Queen Victoria Foundation, Åke Wiberg Foundation, Thelma Zoegas Foundation, The Swedish Rheumatism Association, Skåne University Hospital Research Fund, Research and Development Council of Region Skåne, Sweden.
PG was supported by funding from the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet and by the Karolinska Institutet research funds.
The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buchebner, D., McGuigan, F., Gerdhem, P. et al. Vitamin D insufficiency over 5 years is associated with increased fracture risk—an observational cohort study of elderly women. Osteoporos Int 25, 2767–2775 (2014). https://doi.org/10.1007/s00198-014-2823-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2823-1