Abstract
Purpose
To develop an instrument designed specifically to assess the experience of relatives of patients who die in the intensive care unit (ICU).
Methods
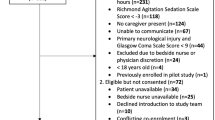
The instrument was developed using a mixed methodology and validated in a prospective multicentre study. Relatives of patients who died in 41 ICUs completed the questionnaire by telephone 21 days after the death, then completed the Hospital Anxiety and Depression Scale, Impact of Event Scale-Revised and Inventory of Complicated Grief after 3, 6, and 12 months.
Results
A total of 600 relatives were included, 475 in the main cohort and 125 in the reliability cohort. The 15-item questionnaire, named CAESAR, covered the patient’s preferences and values, interactions with/around the patient and family satisfaction. We defined three groups based on CAESAR score tertiles: lowest (≤59, n = 107, 25.9 %), middle (n = 185, 44.8 %) and highest (≥69, n = 121, 29.3 %). Factorial analysis showed a single dimension. Cronbach’s alpha in the main and reliability cohorts was 0.88 (0.85–0.90) and 0.85 (0.79–0.89), respectively. Compared to a high CAESAR score, a low CAESAR score was associated with greater risks of anxiety and depression at 3 months [1.29 (1.13–1.46), p = 0.001], post-traumatic stress-related symptoms at 3 [1.34 (1.17–1.53), p < 0.001], 6 [OR = 1.24 (1.06–1.44), p = 0.008] and 12 [OR = 1.26 (1.06–1.50), p = 0.01] months and complicated grief at 6 [OR = 1.40 (1.20–1.63), p < 0.001] and 12 months [OR = 1.27 (1.06–1.52), p = 0.01].
Conclusions
The CAESAR score 21 days after death in the ICU is strongly associated with post-ICU burden in the bereaved relatives. The CAESAR score should prove a useful primary endpoint in trials of interventions to improve relatives’ well-being.


Similar content being viewed by others
References
Angus DC, Barnato AE, Linde-Zwirble WT et al (2004) Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med 32:638–643
Azoulay E, Pochard F, Kentish-Barnes N et al (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994. doi:10.1164/rccm.200409-1295OC
Cuthbertson BH, Hull A, Strachan M, Scott J (2003) Post-traumatic stress disorder after critical illness requiring general intensive care. Intensive Care Med 30:450–455. doi:10.1007/s00134-003-2004-8
Lautrette A, Darmon M, Megarbane B et al (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356:469–478. doi:10.1056/NEJMoa063446
Siegel MD, Hayes E, Vanderwerker LC et al (2008) Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med 36:1722–1728. doi:10.1097/CCM.0b013e318174da72
Nelson JE, Azoulay E, Curtis JR et al (2012) Palliative care in the ICU. J Palliat Med 15:168–174. doi:10.1089/jpm.2011.9599
Clarke EB, Luce JM, Curtis JR et al (2004) A content analysis of forms, guidelines, and other materials documenting end-of-life care in intensive care units. J Crit Care 19:108–117
Patrick DL, Engelberg RA, Curtis JR (2001) Evaluating the quality of dying and death. J Pain Symptom Manage 22(3):717–726
Mularski RA, Heine CE, Osborne ML et al (2005) Quality of dying in the ICU: ratings by family members. Chest 128:280–287. doi:10.1378/chest.128.1.280
Curtis JR, Patrick DL, Engelberg RA et al (2002) A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage 24:17–31
Terwee CB, Bot SDM, de Boer MR et al (2006) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60:34–42. doi:10.1016/j.jclinepi.2006.03.012
Falissard B (2008) Mesurer la subjectivité en santé. Elsevier Masson, Issy-les-Moulineaux
Kentish-Barnes N, Chaize M, Seegers V et al (2015) Complicated grief after death of a relative in the intensive care unit. Eur Respir J 45:1341–1352. doi:10.1183/09031936.00160014
Lance CE (2006) The sources of four commonly reported cutoff criteria: what did they really say? Organ Res Methods. doi:10.1177/1094428105284919
Cattell RB (1966) The scree test for the number of factors. Multivar Behav Res 1:245–276
Guttman L (1954) Some necessary conditions for common-factor analysis. Psychometrika 19:149–161
Cronbach LJ, Warrington WG (1951) Time-limit tests: estimating their reliability and degree of speeding. Psychometrika 16:167–188
Nunnally JC, Bernstein IH, Berge J (1967) Psychometric theory. McGraw-Hill, New York
Falissard B (2012) Psy: various procedures used in psychometry. R package version 1.1. http://CRAN.R-project.org/package=psy. Accessed 1 Jan 2015
Curtis JR (2015) Palliative care in critical illness: challenges for research and practice. Palliat Med 29:291–292. doi:10.1177/0269216315573901
Long AC, Curtis JR (2014) Quality of dying in the ICU: understanding ways to make it better. Intensive Care Med 40:1793. doi:10.1007/s00134-014-3512-4
Aslakson RA, Curtis JR, Nelson JE (2014) The changing role of palliative care in the ICU. Crit Care Med 42:2418–2428. doi:10.1097/CCM.0000000000000573
Curtis JR, Downey L, Engelberg RA (2013) The quality of dying and death: is it ready for use as an outcome measure? Chest 143:289–291. doi:10.1378/chest.12-1941
Glavan BJ, Engelberg RA, Downey L, Curtis JR (2008) Using the medical record to evaluate the quality of end-of-life care in the intensive care unit. Crit Care Med 36:1138–1146. doi:10.1097/CCM.0b013e318168f301
Nelson JE, Mulkerin CM, Adams LL, Pronovost PJ (2006) Improving comfort and communication in the ICU: a practical new tool for palliative care performance measurement and feedback. Qual Saf Health Care 15:264–271. doi:10.1136/qshc.2005.017707
Levy CR, Ely EW, Payne K et al (2005) Quality of dying and death in two medical ICUs: perceptions of family and clinicians. Chest 127:1775–1783. doi:10.1378/chest.127.5.1775
Kentish-Barnes N, McAdam JL, Kouki S et al (2015) Research participation for bereaved family members: experience and insights from a qualitative study. Crit Care Med. doi:10.1097/CCM.0000000000001092
Acknowledgments
These contributors participated to the study: Michel Badet, Chambéry Hospital, Chambéry, France; Julie Carr, Saint Eloi University Hospital, Montpellier, France; Sophie Cayot-Constantin, Estaing University Hospital, Clermont Ferrand, France; Vincent Das, André Grégoire Hospital, Montreuil, France; Fabienne Fieux, Saint Louis University Hospital, Paris, France; Emmanuelle Hammad, Hôpital Nord University Hospital, Marseille, France; Mercé Jourdain, Roger Salengro University Hospital, Lille, France; Véronique Leray, La Croix Rousse Hospital, Lyon, France; Djamel Mokart, Institut Paoli Calmettes, Marseille, France; Sami Hreich Hôpital Nord University Hospital, Marseille, France; Michel Ramakers, Saint Lô Hospital, Saint Lô, France; Jean-Michel Robert, Edouard Herriot University Hospital, Lyon, France; Antoine Roquilly, Hôtel Dieu University Hospital, Nantes, France.
Supported by a Grant from the French Ministry of Health (PHRC 10 104). Medical Intensive Care Unit, Hôpital Saint-Louis, ECSTRA team, Biostatistics and clinical epidemiology, UMR 1153 (Center of Epidemiology and Biostatistics Sorbonne Paris Cité, CRESS), INSERM, Paris Diderot Sorbonne University, Paris, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors declare any conflict of interest in relation to this manuscript.
Additional information
Take-home message: A 15-item questionnaire (CAESAR) proved reliable for assessing the experience of relatives with the dying and death of a loved one in the intensive care unit. This instrument should prove useful as the primary endpoint in trials of interventions designed to improve family care.
The complete list of contributors to this study is detailed in the Electronic Supplementary Material 2.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kentish-Barnes, N., Seegers, V., Legriel, S. et al. CAESAR: a new tool to assess relatives’ experience of dying and death in the ICU. Intensive Care Med 42, 995–1002 (2016). https://doi.org/10.1007/s00134-016-4260-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-016-4260-4