Abstract
Aim
This study aimed to evaluate the effect of trimetazidine (TMZ) in addition to standard treatment on exercise tolerance in patients with ischemic heart disease (IHD).
Methods
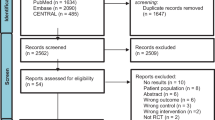
Studies were identified via a systematic search of PubMed, Embase, Cochrane Library, and the Chinese CNKI databases from January 1978 to January 2015. Data extraction, synthesis, and statistical analysis were performed by standard meta-analysis methods. Random or fixed effects models were used to estimate pooled mean differences in total exercise duration (TED), peak oxygen uptake (pVO2), metabolic equivalent system (METS), and 6-minute walking test (6-MWT).
Results
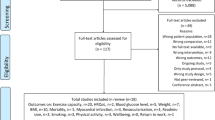
In all, 16 randomized controlled trials (RCTs) consisting of 2,004 participants were included. Pooled results showed that TMZ treatment significantly improved TED (WMD: 37.35, 95 % CI: 25.58–49.13, p < 0.00001), pVO2 (WMD: 2.41, 95 % CI: 1.76–3.06, p < 0.00001), METS (WMD: 1.33, 95 % CI: 0.38–2.28, p = 0.006), and 6-WMT (WMD: 62.46, 95 % CI: 35.86–89.05, p < 0.001) in all patients with IHD. Subgroup analysis showed that TMZ significantly increased TED in nondiabetic participants (WMD 34.77, 95 % CI: 22.28–47.25, p < 0.001), but not in diabetic participants (WMD: 40.36, 95 % CI: − 18.76–99.48, p = 0.18). And, subgroup analysis of TED by intervention duration suggested that there is no statistically difference between the 3-month and 6-month periods (WMD: 35.47, 95 %CI: 18.35–52.60, p < 0.0001 and WMD: 49.94, 95 %CI: 44.69–55.19, p < 0.00001). In addition, TMZ improved TED (WMD: 50.01, 95 % CI: 44.77–55.25 and WMD: 24.20, 95 % CI: 12.72–35.68) in IHD patients with or without heart failure (HF), respectively.
Conclusion
Addition of TMZ to standard treatment significantly improved exercise tolerance in patients with IHD, and IHD patients with HF may experience even more benefits. However, there is insufficient evidence to show that TMZ has beneficial effects in participants with diabetes.
Zusammenfassung
Ziel
Ziel der vorliegenden Studie war es, die Wirkung von Trimetazidin (TMZ) zusätzlich zu der Standardtherapie auf die Belastungstoleranz bei Patienten mit ischämischer Herzerkrankung („ischemic heart disease“, IHD) zu untersuchen.
Methoden
Studien wurden über eine systematische Suche in den Datenbanken PubMed, Embase, Cochrane Library und in der chinesischen CNKI (China National Knowledge Infrastructure) von Januar 1978 bis Januar 2015 gesucht. Die Datenerfassung, -synthese und statistische Analyse erfolgten mit Standardmethoden der Metaanalyse. Random- oder Fixed-Effects-Modelle wurden eingesetzt, um die gepoolten mittleren Differenzen bei der Gesamtbelastungsdauer („total exercise duration“, TED), der Spitzensauerstoffaufnahme („peak oxygen uptake“, pVO2), dem metabolischen Äquivalentsystem („metabolic equivalent system“, METS) und dem 6-min-Gehtest („6-minute walking test“, 6-MWT) abzuschätzen.
Ergebnisse
Es wurden 16 randomisierte kontrollierte Studien (RCT) mit 2004 Teilnehmern in die Auswertung eingeschlossen. Die gepoolten Ergebnisse zeigten, dass die TMU-Behandlung zu einer signifikanten Verbesserung der TED (gewichtete mittlere Differenz, WMD: 37,35; 95 %-Konfidenzintervall, 95%-KI: 25,58–49,13; p < 0,00001), der pVO2 (WMD: 2,41; 95 %-KI: 1,76–3,06; p < 0,00001), des METS (WMD: 1,33; 95 %-KI: 0,38–2,28; p = 0,006) und des 6-WMT (WMD: 62,46; 95 %-KI: 35,86–89,05; p < 0,001) bei allen Patienten mit IHD führte.
Die Subgruppenanalyse ergab, dass TMZ die TED bei Teilnehmern ohne Diabetes mellitus signifikant erhöhte (WMD 34,77; 95 %-KI: 22,28–47,25; p < 0,001), nicht aber bei Teilnehmern mit Diabetes (WMD: 40,36; 95 %-KI: − 18,76–99,48; p = 0,18). Und aus der Subgruppenanalyse der TED nach Interventionsdauer ergaben sich Hinweise darauf, dass statistisch kein Unterschied zwischen der 3-monatigen und der 6-monatigen Dauer bestehe (WMD: 35,47; 95 %-KI: 18,35–52,60; p < 0,0001 bzw. WMD: 49,94; 95 %-KI: 44,69–55,19; p < 0,00001). Außerdem zeigte sich eine Verbesserung der TED unter TMZ (WMD: 50,01; 95 %-KI: 44,77–55,25 bzw. WMD: 24,20; 95 %-KI: 12,72–35,68) bei IHD-Patienten mit bzw. ohne Herzinsuffizienz.
Schlussfolgerung
Die zusätzliche Gabe von TMZ zur Standardbehandlung verbesserte die Belastungstoleranz signifikant bei Patienten mit ischämischer Herzerkrankung. IHD-Patienten mit Herzinsuffizienz haben möglicherweise noch einen größeren Nutzen. Es gibt jedoch keine ausreichende Evidenz dafür, dass TMZ einen Nutzeffekt bei Teilnehmern mit Diabetes mellitus habe.




Similar content being viewed by others
References
Kantor PF, Lucien A, Kozak R, Lopaschuk GD (2000) The antianginal drug trimetazidine shifts cardiac energy metabolism from fatty acid oxidation to glucose oxidation by inhibiting mitochondrial long-chain 3-ketoacyl coenzyme A thiolase. Circ Res 86(5):580–588
Ruixing Y, Wenwu L, Al-Ghazali R (2007) Trimetazidine inhibits cardiomyocyte apoptosis in a rabbit model of ischemia-reperfusion. Transl Res 149(3):152–160
Williams FM, Tanda K, Kus M, Williams TJ (1993) Trimetazidine inhibits neutrophil accumulation after myocardial ischaemia and reperfusion in rabbits. J Cardiovasc Pharmacol 22(6):828–833
Di Napoli P, Chierchia S, Taccardi AA et al (2007) Trimetazidine improves post-ischemic recovery by preserving endothelial nitric oxide synthase expression in isolated working rat hearts. Nitric Oxide 16(2):228–236
Rodrigues B, Cam MC, McNeill JH (1995) Myocardial substrate metabolism: implications for diabetic cardiomyopathy. J Mol Cell Cardiol 27(1):169–179
Brottier L, Barat JL, Combe C et al (1990) Therapeutic value of a cardioprotective agent in patients with severe ischaemic cardiomyopathy. Eur Heart J 11(3):207–212
Lu C, Dabrowski P, Fragasso G, Chierchia SL (1998) Effects of trimetazidine on ischemic left ventricular dysfunction in patients with coronary artery disease. Am J Cardiol 82(7):898–901
Chang JA, Froelicher VF (1994) Clinical and exercise test markers of prognosis in patients with stable coronary artery disease. Curr Probl Cardiol 19(9):533–587
Pate RR, Pratt M, Blair SN et al (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 273(5):402–407
Zhang L, Lu Y, Jiang H et al (2012) Additional use of trimetazidine in patients with chronic heart failure: a meta-analysis. J Am Coll Cardiol 59(10):913–922
Zhou X, Chen J (2014) Is treatment with trimetazidine beneficial in patients with chronic heart failure? PLoS One 9(5):e94660
Gao D, Ning N, Niu X, Hao G, Meng Z (2011) Trimetazidine: a meta-analysis of randomised controlled trials in heart failure. Heart 97(4):278–286
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
El-Kady T, El-Sabban K, Gabaly M, Sabry A, Abdel-Hady S (2005) Effects of trimetazidine on myocardial perfusion and the contractile response of chronically dysfunctional myocardium in ischemic cardiomyopathy: a 24-month study. Am J Cardiovasc Drugs 5(4):271–278
Sisakian AS, Torgomian AL, Barkhudarian AL (2006) The effects of trimetazidine on left ventricular function and physical exercise tolerance in patients with ischemic cardiomyopathy. Klin Med (Mosk) 84(10):55–58
Belardinelli R, Purcaro A (2001) Effects of trimetazidine on the contractile response of chronically dysfunctional myocardium to low-dose dobutamine in ischaemic cardiomyopathy. Eur Heart J 22(23):2164–2170
Fragasso G, Piatti Md PM, Monti L et al (2003) Short- and long-term beneficial effects of trimetazidine in patients with diabetes and ischemic cardiomyopathy. Am Heart J 146(5):E18
Vitale C, Spoletini I, Malorni W et al (2013) Efficacy of trimetazidine on functional capacity in symptomatic patients with stable exertional angina—the VASCO-angina study. Int J Cardiol 168(2):1078–1081
Szwed H, Sadowski Z, Elikowski W et al (2001) Combination treatment in stable effort angina using trimetazidine and metoprolol: results of a randomized, double-blind, multicentre study (TRIMPOL II). TRIMetazidine in POLand. Eur Heart J 22(24):2267–2274
Ribeiro LW, Ribeiro JP, Stein R, Leitao C, Polanczyk CA (2007) Trimetazidine added to combined hemodynamic antianginal therapy in patients with type 2 diabetes: a randomized crossover trial. Am Heart J 154(1):78.e71–e77
Di Napoli P, Di Giovanni P, Gaeta MA, D’Apolito G, Barsotti A (2007) Beneficial effects of trimetazidine treatment on exercise tolerance and B-type natriuretic peptide and troponin T plasma levels in patients with stable ischemic cardiomyopathy. Am Heart J 154(3):602. e601–e605
Belardinelli R, Lacalaprice F, Faccenda E, Volpe L (2008) Trimetazidine potentiates the effects of exercise training in patients with ischemic cardiomyopathy referred for cardiac rehabilitation. Eur J Cardiovasc Prev Rehabil 15(5):533–540
Belardinelli R, Solenghi M, Volpe L, Purcaro A (2007) Trimetazidine improves endothelial dysfunction in chronic heart failure: an antioxidant effect. Eur Heart J 28(9):1102–1108
Belardinelli R, Cianci G, Gigli M, Mazzanti M, Lacalaprice F (2008) Effects of trimetazidine on myocardial perfusion and left ventricular systolic function in type 2 diabetic patients with ischemic cardiomyopathy. J Cardiovasc Pharmacol 51(6):611–615
Chazov EI Lepakchin VK, Zharova EA et al (2005) Trimetazidine in Angina Combination Therapy–the TACT study: trimetazidine versus conventional treatment in patients with stable angina pectoris in a randomized, placebo-controlled, multicenter study. Am J Ther 12(1):35–42
Manchanda SC, Krishnaswami S (1997) Combination treatment with trimetazidine and diltiazem in stable angina pectoris. Heart 78(4):353–357
Hui D (2006) Trimetazidine treatment of unstable angina pectoris clinical observation of 50 cases. Chin J Cardiovasc Rehabil Med 15(6):581–583. doi:10.3969/j.issn.1008-0074.2006.06.023
Teng Y (2011) Effect of trimetazidine in the treatment of stable angina pectoris. Chin J Mod Drug Appl 11,187–188
Zhang Z, Jun-ai MA (2006) Effect of trimetazidine in the treatment of chronic heart failure of left ventricle in Patients with coronary heart disease. Chin J Cardiovasc Med 04:301–303
Ferraro E, Giammarioli AM, Caldarola S et al (2013) The metabolic modulator trimetazidine triggers autophagy and counteracts stress-induced atrophy in skeletal muscle myotubes. Febs J 280(20):5094–5108
Monti LD, Setola E, Fragasso G et al (2006) Metabolic and endothelial effects of trimetazidine on forearm skeletal muscle in patients with type 2 diabetes and ischemic cardiomyopathy. Am J Physiol Endocrinol Metab 290(1):E54–E59
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Zhao, L. Peng, Y. Luo, S. Li, Z. Zheng, R. Dong, J. Zhu, and J. Liu state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Zhao, Y., Peng, L., Luo, Y. et al. Trimetazidine improves exercise tolerance in patients with ischemic heart disease. Herz 41, 514–522 (2016). https://doi.org/10.1007/s00059-015-4392-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4392-2