Abstract
Background
A federally funded demonstration project (Project SCOPE) was conducted to develop a model for delivering screening colonoscopy to underinsured patients in Suffolk County, NY. The recruitment model featured collaboration between Stony Brook University Medical Center and the Suffolk County Department of Health Services’ network of community health centers; bilingual patient navigators, and reimbursement of physicians and the hospital at Medicare rates.
Methods
We conducted a retrospective analysis of all (11,752) colonoscopies performed at Stony Brook Medicine, during the pre-SCOPE time period (2003–2004), during SCOPE period (2007–2008), and post-SCOPE (2010–2011), to measure the impact of SCOPE on reducing racial and ethnic disparities. Multiple logistic regression models were used to compare the likelihood of a patient being Hispanic or African American after adjusting for potential covariates.
Results
The numbers of Hispanics undergoing colonoscopies were 146 (4.3 %), 506 (12.3 %), and 262 (6 %) during the pre-SCOPE, SCOPE, and post-SCOPE time periods. The numbers of African Americans were 166 (5.1 %), 298 (7.2 %), and 255 (5.8 %). The odds ratio (OR = 1.4, 95 % CI = 1.06–1.83, p = 0.014) of a screening colonoscopy patient being Hispanic during the Project SCOPE period compared to the post-SCOPE period remained significant after taking into consideration the other covariates, such as diabetes, smoking, and insurance status.
Conclusions
Project SCOPE had a significant impact on increasing the proportion of Hispanics undergoing screening colonoscopies. Factors such as bilingual patient navigators, in addition to removing financial barriers, may have contributed to the increase.
Similar content being viewed by others
Introduction
Racial/ethnic disparities in colorectal cancer (CRC) screening have frequently been reported [1–4]. Although colonoscopy is increasingly used for colorectal cancer screening, minorities, who comprise one third of the United States population, lag behind non-Hispanic whites [5, 6]. According to the Centers for Disease Control and Prevention (CDC), 46.5 % of Hispanics, 55.0 % of African-Americans, and 46.9 % of Asians underwent screening colonoscopy in 2010 compared to 59.8 % of non-Hispanic whites [7, 8].
Previous studies have suggested that socioeconomic status may contribute to disparities in CRC screening for minorities. One of the more frequently noticeable covariates attributing to this discrepancy is the health insurance of these patients [3, 9]. According to the United States Department of Health and Health Services (HHS), 30.7 % of Hispanics, 20.8 % of black or African-Americans, and 18.1 % of Asian-Americans were not insured while only 11.7 % of white Americans were uninsured [10].
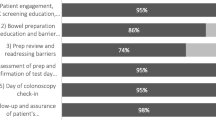
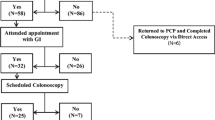
To combat this disparity, in 2005–2009, the CDC funded five demonstration projects in the USA to potentially increase the rate of CRC screening in the uninsured and underinsured [11]. One of these five projects was led by Stony Brook University Medical Center (SBUMC) in collaboration with Suffolk County Department of Health Services and was known as the Suffolk County Preventive Endoscopy Project (Project SCOPE). Project SCOPE provided the necessary funding to cover the cost for the procedures, which were performed by gastroenterologist at SBUMC. As described in greater detail elsewhere [12], in addition to removing financial barriers, Project SCOPE used other approaches to facilitate screening colonoscopy completion by underserved racial and ethnic minorities. This included bilingual patient navigators that provided language and culturally appropriate support services. Also, a pre-colonoscopy telephone “visit” with a project clinician made it feasible for patients to make a single visit to the gastroenterologist at the time of colonoscopy, which translated into one less day of work missed. A protocol for patient referral to SCOPE was developed with the County health centers, and this included expedited patient scheduling by the project clinician at the time of the pre-colonoscopy telephone “visit.”
This current retrospective study aim to assess the effects of Project SCOPE on the proportion of Hispanics and African-Americans undergoing total and screening colonoscopies at SBUMC, by comparing the proportions prior to, during and after Project SCOPE, taking into consideration the potential confounding covariates such as insurance. Finally, the risk factors associated with specific colonoscopic pathologic outcomes were investigated.
Methods
Patient Data Acquisition and Cohorts
This study was approved by the Institutional Review Boards of Stony Brook University. We used colonoscopy records from January 1, 2003 to December 31, 2011 via SBUMC Endoscopy Database. Personal health information (PHI) was stripped from the data and assigned a patient code for de-identifying purposes. Then, the 2003–2011 data sets were divided into three cohorts: pre-SCOPE time period (January 1, 2003–December 31, 2004), Project SCOPE time period (January 1, 2007–December 31, 2008), and post-SCOPE time period (January 1, 2010–December 31, 2011). Project SCOPE was from 2005–2009; however, we chose to only look at 2007–2008 when the program was well underway to avoid periods of transition. Other time frames during Project SCOPE were considered but would have included transitional periods of start-up and close-down. The socioeconomic (e.g., insurance), clinical, and pathological metadata were curated from electronic medical records, and Project SCOPE research records were stripped of identifying information after linking this data to the procedures. These variables could be extracted during the Project SCOPE and post-Project SCOPE time periods, but not during the pre-Project SCOPE time period.
Inclusion and Exclusion Criteria
Procedures were excluded from the study if the procedures were incomplete (e.g., poor bowel prep). Because the United States Preventive Services Task Force (USPSTF) recommends screening for individuals over the age of 50 years [13], only data on patients who were ≥50 and ≤80 were included in the analysis. Procedures performed on patients with inflammatory bowel diseases or on patients with possible ischemic colitis were excluded from this study.
Ethnicity Designation
Based on the United States Census Bureau [6], patients were classified into five major self-reported racial/ethnic categories: non-Hispanic whites, black or African-American, Asian-American, Hispanics/Latinos, and non-Hispanic other. In this study, we focused on Hispanic and African-American minorities, since the proportion of the other minorities was too low to analyze. Also, there were Hispanic Asians and Hispanic African-Americans. These individuals were reclassified as Asian or African-American rather than Hispanics.
Screening versus Diagnostic Colonoscopies
The designation of diagnostic versus screening was assigned according to the American Gastroenterological Association’s (AGA) criteria [14], after reviewing the colonoscopy records and the medical records. The AGA’s criteria on screening colonoscopy are asymptomatic patients that only have a previous personal history of polyps or adenocarcinoma and/or family history of polyps or adenocarcinoma. Please note, however, that Project SCOPE’s policy for the CDC CRC screening demonstration project excluded patients with a personal history of polyps or adenocarcinoma [11].
Socioeconomic Status/Other Covariates
Socioeconomic status was determined by the patient’s medical insurance. Medical insurance was classified into four categories: (1) Private; (2) Medicare (or Medicare equivalent); (3) Medicaid (or Medicaid equivalent); and (4) Self-pay (no insurance). Project SCOPE patients were included in the Self-pay category but their colonoscopies were ultimately paid for by the CDC grant. If there were patients that had multiple insurance coverage plans, we chose their highest level of insurance (Private (highest) > Medicare > Medicaid > Self-pay (lowest).
In addition to insurance, other covariates such as age, gender, smoking, diabetes mellitus, obesity, aspirin and non-steroidal anti-inflammatory drugs (NSAIDs), and personal and family history of colonic neoplasia have been identified as a risk factor for colonic neoplasia [15–23]; therefore, these covariates were also abstracted from the medicals records. Smoking history and family history of colonic neoplasia were self-defined in the medical records.
Pathologic Outcomes
To measure colonoscopic pathologic outcomes, results were classified into the following eight categories: (1) no histopathologic abnormalities; (2) inflammatory polyps only; (3) hyperplastic polyps only; (4) adenomatous polyp only; (5) serrated polyps only; (6) other tumors only (leiomyoma or carcinoids); (7) adenomas and serrated polyps (also termed serrated adenomas); (8) adenocarcinoma (with or without polyps). Also, high grade dysplasia was not noted as a specific pathologic diagnosis because in every case, it was accompanied by another surgical pathology such as tubular adenoma or hyperplastic polyp. Due to limited cases in some categories, only three colonoscopic pathologic outcomes were further investigated in the risk factor analysis: adenoma with or without serrated polyps (categories 4 and 7), serrated polyps with or without adenomas (categories 5 and 7), and adenocarcinoma (category 8).
Statistical Analysis
To compare patient characteristics and other clinical factors among three time periods, chi-square test or Fisher’s exact test was performed for categorical variables (e.g., gender and ethnicity/race), and one-way ANOVA or two sample t test was used for continuous variables (e.g., patient’s age at procedure and BMI). Univariate logistic regression models were used to assess the odds of a patient being Hispanic or African-American in the three time periods first. Any variable that had a p value < 0.1 in univariate logistic regression models, and their two-way interactions were further assessed using a multiple logistic regression model. Odds ratios (OR) and their 95 % confidence intervals (CI) reported were from the final model after backward selection with a significance level of 0.05. Firth’s bias correction was used to estimate OR if there was zero count in some subgroup. Significance level after Bonferroni adjustment was set at 0.025 to take into account the fact that two different outcome variables were analyzed for the primary objective. As an exploratory analysis, similar modeling strategies were used to assess the risk factors for early diagnosis of colorectal cancer: adenoma with or without serrated polyps (categories 4 and 7), serrated polyps with or without adenomas (categories 5 and 7), and adenocarcinoma (category 8). Bonferroni adjustment was not applied here because of the exploratory nature. SAS 9.3 (SAS Institute, Inc., Cary, NC) was used for all of the statistical analysis in this study and p values were based on two-sided tests.
Results
Patient Characteristics for All Colonoscopies
The patient characteristics of the entire study population for the pre-SCOPE (n = 3,267), Project SCOPE (n = 4,127), and the post-SCOPE time periods (n = 4,358) are shown in Tables 1 and 2. Based on univariate analysis, higher proportions of Hispanics and African-American patients were observed in the Project SCOPE era compared with either the pre- or post-SCOPE time periods for the overall study population. Significantly, different covariates among all three time periods are listed in Table 1. Comparison of factors other than medical insurance status, gender, and age could only be conducted on the Project SCOPE and post-SCOPE time periods. The factors that were statistically significantly different between during Project SCOPE and post-SCOPE time periods are listed in Table 2.
Information on whether a colonoscopy was designated as screening was only available for the Project SCOPE (n = 2,395) and post-SCOPE time periods (n = 1,995, Tables 3 and 4). Univariate analysis of this more restricted population yielded similar conclusions to those reached for the total study population in which higher proportions of Hispanics and African-American patients were observed in the Project SCOPE versus the post-SCOPE time period. Covariates that were significantly different between Project SCOPE and post-SCOPE time periods for screening colonoscopy patients are listed in Tables 3 and 4.
Hispanics
The difference in the odds of patients being Hispanic remained significant after controlling for gender, age, and medical insurance and their first-order interaction terms during the three time periods. As shown in Table 5, patients were more likely to be Hispanic during the Project SCOPE time period compared to the post-SCOPE time period (OR = 1.367; 95 % CI = 1.149–1.627, p = 0.0004), or compared to the pre-SCOPE time period (OR = 2.196; 95 % CI = 1.779–2.710, p < 0.0001). Patients were also more likely to be Hispanic during the post-SCOPE (OR = 1.605; 95 % CI = 1.290–1.996, p < 0.0001) than the pre-SCOPE time period.
When only the Project SCOPE and post-Project SCOPE time periods were considered, additional factors (e.g., tobacco use, see Table 6) could be included to assess the contributions of these factors, as well as all their first-order interaction terms. Hispanic patients once again were more likely to undergo colonoscopy during Project SCOPE even after including additional covariates and their two-way interaction terms (OR = 1.283; 95 % = 1.062–1.550, p = 0.0099). This remained true after repeating the analysis for just screening colonoscopies (OR = 1.397; 95 % = 1.065–1.833, p = 0.016). Table 7 also listed other factors or two-way interactions that were associated with patients being Hispanic based on data from these two time periods.
African-Americans
Gender, medical insurance status, and age and their two-way interactions were further considered when comparing African-American patients undergoing colonoscopy during the three time periods. As shown in Table 5, there was a strong evidence to show that the odds of patients being African-American were significantly different among three time periods after adjusting for medical insurance, gender, and their two-way interaction (p = 0.0023). African-Americans were more likely to undergo colonoscopy during Project SCOPE (OR = 1.437; 95 % CI = 1.162–1.778, p = 0.0008) than pre-SCOPE time period and more likely during post-SCOPE (OR = 1.359; 95 % CI = 1.101–1.678, p = 0.0043) than pre-SCOPE time period. There were no significant differences between Project SCOPE (OR = 1.058; 95 % CI = 0.879–1.272, p = 0.5516) and post-SCOPE time periods.
When only the Project SCOPE and post-SCOPE time periods were considered, additional factors (e.g., tobacco use, see Table 6) could be included to assess the contributions of these factors, as well as all their first-order interaction terms. In contrast to Hispanics, not enough evidence existed for the significant difference in the odds of patients being African-Americans (OR = 1.120; 95 % CI = 0.920–1.364, p = 0.2593) after taking into account these additional factors (see Table 6). The same situation remained after repeating the analysis for just screening colonoscopies (See Table 7). When insurance was removed from the multiple logistic regression model, among all the screening colonoscopy patients, the odds of a patient being African-American during Project SCOPE are higher than in the post-SCOPE time period (OR = 1.44, 95% CI = 1.13–1.82, p = 0031).
Risk Factors for Adenomas, Serrated Polyps, and CRC
As a secondary endpoint, we examined colonoscopy outcomes with respect to the detection of adenomas, serrated polyps, and CRC during the Project SCOPE and post-SCOPE time periods (Supplementary Tables S5–S8, Tables 8 and 9). No effect of African-American race or Hispanic ethnicity was detected with respect to these secondary outcomes. Logistic regression analysis revealed that detection of adenomas, when considering all colonoscopies (see Table 8), was significantly associated with increased age (OR = 1.149/5 years, 95 % CI = 1.111–1.187, p < 0.0001), male gender (OR = 1.577, 95 % CI = 1.420–1.754, p < 0.0001), smoking (current smoker vs. never smoked; OR = 1.693, 95 % CI = 1.447–1.982 and former smoker vs. never smoked; OR = 1.2, 95 % CI = 1.069–1.348, p < 0.0001), and a positive family history of CRC (OR = 1.231, 95 % CI = 1.024–1.482, p = 0.0264). Significant first-order interaction terms are listed in Table 8. Detection of sessile serrated polyps were significantly associated with current smokers but not former smokers (overall smoking p = 0.0005; current smoker vs. never smoked OR = 3.184, 95 % CI = 1.75–5.794 p = 0.0001; former smoker vs. never smoked OR = 1.353, 95 % CI = 0.776–2.389, p = 0.2980; more recent time period OR = 2.01, 95 % CI = 1.179–3.425, p = 0.01; and positive family history of CRC OR = 2.29, 95 % CI = 1.22–4.3, p = 0.01). Detection of adenocarcinoma was associated with increased age (OR = 1.37/5 years, 95 % CI = 1.22–1.54, p < 0.0001), male gender (OR = 2.09, 95 % CI = 1.37–3.19, p = 0.0006), a positive personal history of CRC (OR = 8.23, 95 % CI = 4.4–15.4, p < 0.0001), and not having a previous colonoscopy (OR = 4.88, 95 % CI = 2.79–8.55, p < 0.0001) (Table 8).
When only screening colonoscopies were analyzed, the total number of adenocarcinomas detected was decreased to only 13 (with 87 detected on diagnostic colonoscopies); whereas the number of adenomas and serrated polyps detected in screening and diagnostic colonoscopies were similar. Logistic regression analysis revealed that detection of adenomas in screening colonoscopies was also significantly associated with increased age (OR = 1.186/5 years, 95 % CI = 1.126–1.250, p < 0.0001), smoking (current smokers vs. patients who never smoked OR = 2.086, 95 % CI = 1.665–2.613, p < 0.0001; ex-smoker vs. patients who never smoked OR = 1.363, 95 % CI = 1.001–1.727, p = 0.0003), and lack of insurance (p = 0.0032). Significant first-order interaction terms are listed in Table 8. Detection of sessile serrated polyps was significantly associated with male gender (OR = 2.392, 95 % CI = 1.135–5.025, p = 0.0219), tobacco (current smokers vs. patients who never smoked OR = 4.198, 95 % CI = 1.729–10.195, p = 0.0015), and NSAIDs use (OR = 3.179, 95 % CI = 1.086–9.307, p = 0.0349). For screening colonoscopies, only male gender was significantly associated with detection of adenocarcinoma in univariate analysis (p = 0.0089) (Table 9).
Discussion
In this study, we report the impact of a federally funded program to expand screening colonoscopy access to indigent patients on the percentage of Hispanic and African-American minorities undergoing colonoscopies at a single academic medical center before, during, and after the program. During the post-SCOPE period, financial assistance reverted to pre-SCOPE levels. For many of the indigent patients, the cost of the screening procedure with maximal financial assistance was beyond their means. Bilingual patient navigator services also came to an end. The major observation of this study is that the odds ratio of a screening colonoscopy being completed by a Hispanic patient during Project SCOPE remained significant, even after inclusion of multiple covariates in the logistic regression. Because medical insurance status was included in the analysis, that factor besides removing financial barriers may have contributed. Ninety percent of Hispanic patients preferred Spanish language [11]. The patient interactions with the clinician and patient navigator included education about colorectal cancer and screening during the course of the conversation, e.g., response to patient’s questions and addressing fears, which may have previously deterred accepting colonoscopy or understanding the necessity of screening for colorectal cancer. Since language is so critical to general health literacy, the addition of patient navigation likely had a greater impact among Hispanics. Previous publications have also reported the benefits of using patient navigators for underrepresented minorities as well as removal of financial barriers [24–32].
In contrast, the likelihood that a patient undergoing screening colonoscopies was African-American did not reach significance when multiple covariates were included in the analysis (Table 5), although they did differ significantly if insurance was not included in the model, and there were more African-Americans completing screening colonoscopy during Project SCOPE than post-SCOPE time period. Since African-Americans have a higher risk of colorectal cancer than whites or Hispanics, it is important not to lose sight of the critical role of insurance coverage for early colorectal cancer detection in African-Americans. Access to diagnostic colonoscopy may be less of a barrier than access to screening colonoscopy, and the motivation to complete the screening colonoscopy less strong than in a symptomatic patient seeking a diagnostic colonoscopy. There were fewer African-Americans than Hispanics, possibly related to the demographics of Suffolk County, where Hispanics are the largest growing minority in the region. One potential explanation for the lack of significance is that the analysis including multiple covariates is underpowered. Alternatively, the language barrier and consequently the impact of losing bilingual patient navigator services may have been less of a factor in African-Americans compared to Hispanics.
Through Project SCOPE, a referral protocol and pattern were created for colonoscopy screening of health center patients and survey data collected a month after screening, documented high satisfaction among health center patients with the services received. The overall (modest) increase in the representation of Hispanics and African-Americans in total colonoscopies post-SCOPE compared to pre-SCOPE time period may reflect Project SCOPE’s outreach efforts to increase the awareness of the need for colorectal cancer screening in patients attending the surrounding community health centers.
Multiple logistic regression analysis on the detection of premalignant neoplasms (adenomas and serrated polyps) in screening colonoscopies revealed increased detection with lack of insurance, increased age, and smoking. Age [15] and smoking [23] have been previously identified as positively associated with an increased risk of adenomas. The total number of adenocarcinomas detected on screening colonoscopies was only 13. This is because the remaining 81 carcinomas were detected on diagnostic colonoscopies. This greatly limits our ability to analyze the factors associated with detecting adenocarcinomas on screening colonoscopies. On univariate analysis, only male gender was significantly associated with detection of adenocarcinoma. The factors associated with detecting adenomas on screening colonoscopies were similar to those identified with detection of adenomas on all colonoscopies.
Limitations of this study include the data presented is from only a single site. Additional limitations were that complete patient metadata could not be retrieved from the Project SCOPE time period and during the pre-SCOPE time period colonoscopy reports and patient metadata were not available.
While colonoscopy remains the gold standard for the diagnosis of colorectal cancer and the only procedure for the removal of premalignant adenomatous polyps, it remains unclear what the best approach is for initial colorectal cancer screening, particularly in patients with limited financial means [33, 34]. Different insurers vary greatly on which colonoscopic procedures are covered completely and which require copayments [35]. The state of Delaware has taken the lead on expanding coverage for colon cancer screening using colonoscopy as the initial screening tool [36]. The current mechanism for colorectal cancer screening for indigent patients in Suffolk County, New York relies on initial fecal immune chemical testing followed by colonoscopy only if the tests are positive for occult blood through the New York State Department of Health Cancer Services Program [33, 34]. It is critical that the impact of all of these interventions be carefully monitored in order to refine models of delivering colorectal cancer screening to vulnerable populations. Based on the results of this study, Stony Brook University Hospital has made a commitment to hire full time bilingual nurse patient navigator, in order to reduce the language barrier and to continue handling the pre-colonoscopy visit by telephone for eligible patients.
References
O’Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage gaps in colorectal cancer screening among Medicare beneficiaries. Arch Intern Med. 2005;165:2129–35.
Lees KA, Wortley PM, Coughlin SS. Comparison of racial/ethnic disparities in adult immunization and cancer screening. Am J Prev Med. 2005;29:404–11.
Gonzales M, Nelson H, Rhyne RL, Stone SN, Hoffman RM. Surveillance of colorectal cancer screening in new Mexico Hispanics and non-Hispanic whites. J Community Health. 2012;37:1279–88.
Jerant AF, Fenton JJ, Franks P. Determinants of racial/ethnic colorectal cancer screening disparities. Arch Intern Med. 2008;168:1317–24.
CDC Health Disparities and Inequalities Report Fact Sheet, United States. 2011. Available at: http://www.cdc.gov/minorityhealth/reports/CHDIR11/FactSheet.pdf.
Humes KR, Jones NA, Ramirez, RR. The Overview of Race and Hispanic Origin: 2010; 2010 Census Briefs. http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. Issued March 2011, accessed April 2013.
Centers for Disease Control and Prevention. Morbidity and mortality weekly report: Cancer screening-United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:41–5.
Centers for Disease Control and Prevention. Cancer screening in the United States. Available at: http://www.cdc.gov/cancer/colorectal/what_cdc_is_doing/screening_us.htm. Accessed May 2013.
Trivers KF, Shaw KM, Sabatino SA, Shapiro JA, Coates RJ. Trends in colorectal cancer screening disparities in people aged 50–64 years, 2000–2005. Am J Prev Med. 2008;35:185–93.
ASPE/Health Policy. Overview of the Uninsured in the United States: A Summary of the 2011 Current Population Survey; ASPE Issue Brief. http://aspe.hhs.gov/health/reports/2011/CPSHealthIns2011/ib.pdf. Issued September 2011, last accessed May 2013.
Seeff LC, Royalty J, Helsel WE, Kammerer WG, Boehm JE, et al. Clinical outcomes from the CDC's Colorectal Cancer Screening Demonstration Program. Cancer. 2013;119 Suppl 15:2820–33.
Lane DS, Cavanagh MF, Messina CR, Anderson JC. An academic medical center model for community colorectal cancer screening: The Centers for Disease Control and Prevention Demonstration Program Experience. Acad Med. 2010;85:1354–61.
Zauber AG, Landsdorp-Vogelaar II, Knudsen AB, Wilschut J, van Ballegooijen M, et al. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:659–69.
American Gastroenterological Association. Screening Versus Diagnostic Colonoscopy: What You, Your Patients and Referring Physicians Should Know. Available at: http://www.gastro.org/journals-publications/gi-quality-and-practice-management-news/2011/screening-versus-diagnostic-colonoscopy-what-you-your-patients-and-referring-physicians-should-know. Accessed June 2013.
Rex DK, Lehman GA, Ulbright TM, Smith JJ, Pound DC, et al. Colonic neoplasia in asymptomatic persons with negative fecal occult blood tests: Influence of age, gender, and family history. Am J Gastroenterol. 1993;88:825–31.
Botteri E, Iodice S, Raimondi S, Maisonneuve P, Lowenfels AB. Cigarette smoking and adenomatous polyps: Meta-analysis. Gastroenterology. 2008;134:388–95.
Sedjo RL, Byers T, Levin TR, Haffner SM, Saad MF, et al. Change in body size and the risk of colorectal adenomas. Cancer Epidemiol Biomarkers Prev. 2007;16:526–31.
Yuhara H, Steinmaus C, Cohen SE, Corley DA, Tei Y, et al. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. 2011;106:1911–21.
Murff HJ, Shrubsole MJ, Chen Z, Smalley WE, Chen H, et al. Nonsteroidal anti-inflammatory drug use and risk of adenomatous and hyperplastic polyps. Cancer Prev Res (Phila). 2011;4:1799–807.
Winawer SJ, Zauber AG, Ho MN, O'Brien MJ, Gottlieb LS, et al. Prevention of colorectal cancer by colonoscopic polypectomy. N Eng J Med. 1993;329:1977–81.
Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95.
Kerber RA, Slattery ML, Potter JD, Caan BJ, Edwards SL. Risk of colon cancer associated with a family history of cancer or colorectal polyps: the diet, activity, and reproduction in colon cancer study. Int J Cancer. 1998;78:157–60.
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Ascherio A, et al. A prospective study of cigarette smoking and risk of colorectal adenoma and colorectal cancer in U.S. men. J Natl Cancer Inst. 1994;86:183–91.
Jandorf L, Gutierrez Y, Lopez J, Christie J, Itzkowitz SH. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82:216–24.
Nash D, Azeez S, Vlahov D, Schori M. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006;83:231–43.
Ananthakrishnan AN, Schellhase KG, Sparapani RA, Laud PW, Neuner JM. Disparities in colon cancer screening in the Medicare population. Arch Intern Med. 2007;167:258–64.
Richards CA, Kerker BD, Thorpe L, Olson C, Krauskopf MS, et al. Increased screening colonoscopy rates and reduced racial disparities in the New York Citywide Campaign: an urban model. Am J Gastroenterol. 2011;106:1880–6.
Grubbs SS, Polite BN, Carney Jr J, Bowser W, Rogers J, et al. Eliminating racial disparities in colorectal cancer in the real world: it took a village. J Clin Oncol. 2013;31:1928–30.
Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med. 2012;27:1033–46.
Lane DS, Messina CR, Cavanagh MF, Chen JJ. A provider intervention to improve colorectal cancer screening in county health centers. Med Care. 2008;46:S109–16.
Meissner HI, Breen N, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the United States. Cancer Epidemiol Biomarkers Prev. 2006;15:389–94.
Stimpson JP, Pagán JA, Chen LW. Reducing racial and ethnic disparities in colorectal cancer screening is likely to require more than access to care. Health Aff (Millwood). 2012;31:2747–54.
Quintero E, Castella A, Bujanda L, et al. Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. N Engl J Med. 2012;366:697–706.
Lee JK, Liles EG, Bent S, et al. Accuracy of fecal immunochemical tests for colorectal cancer: Systematic review and meta-analysis. Ann Intern Med. 2014;160:171–81.
Avital I, Langan RC, Summers TA, Steele SR, Waldman SA, et al. Evidence-based Guidelines for Precision Risk Stratification-Based Screening (PRSBS) for Colorectal Cancer: Lessons learned from the US Armed Forces: Consensus and Future Directions. J Cancer. 2013;4:172–92.
Politz K, Lucia K, Keith K. Coverage of Colonoscopies under the Affordable Care Act’s Prevention Benefit. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8351.pdf. Issued September 2012, last accessed July 2013.
Acknowledgments
This work was supported partially by the Stony Brook Medicine Department of Medicine Seed Grant Award (J.B) and the Simons Foundation (E.L.). We thank Diana Kaplan and Matthew Katz for assistance with curating the clinical metadata for the Project SCOPE and post-Project SCOPE time periods. In addition, we thank Beth Hollister for assistance in retrieving many of the colonoscopy reports. We would also like to thank the Biostatistical Consulting Core in the School of Medicine for their statistical support.
Conflict of Interest
Phillip Son BA, Dorothy S. Lane, MD, MPH, Catherine R. Messina, PhD, Jie Yang, PhD, Jiawen Zhu, MS, Ellen Li MD, PhD, Satish Nagula, MD, Chris E. Lascarides, MD Juan Carlos Bucobo, MD declare no conflicts of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table S1
(PDF 29 kb)
Supplementary Table S2
(PDF 28 kb)
Supplementary Table S3
(PDF 28 kb)
Supplementary Table S4
(PDF 29 kb)
Supplementary Table S5
(PDF 26 kb)
Supplementary Table S6
(PDF 30 kb)
Supplementary Table S7
(PDF 30 kb)
Supplementary Table S8
(PDF 30 kb)
Rights and permissions
About this article
Cite this article
Son, P., Lane, D.S., Messina, C.R. et al. Impact of Project SCOPE on Racial/Ethnic Disparities in Screening Colonoscopies. J. Racial and Ethnic Health Disparities 1, 110–119 (2014). https://doi.org/10.1007/s40615-014-0016-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-014-0016-4