Abstract
Background
Clostridium difficile infection (CDI) recurs in nearly one-third of patients who develop an initial infection. Recurrent CDI (RCDI) is associated with considerable morbidity, mortality, and cost. Treatment for RCDI has not been not well examined.
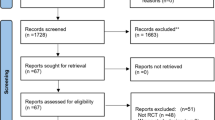
Methods
A systematic review.
Results
Sixty-four articles were identified evaluating eight different treatment approaches: metronidazole, vancomycin, fidaxomicin, nitazoxanide, rifampin, immunoglobulins, probiotics, and fecal bacteriotherapy. The meta-analysis found vancomycin to have a similar efficacy to metronidazole, although studies used varying doses and durations of therapy. Fidaxomicin was slightly more efficacious than vancomycin, though the number of studies was small. Good evidence for probiotics was limited. Fecal bacteriotherapy was found to be highly efficacious in a single randomized trial.
Conclusion
Metronidazole and vancomycin have good evidence for use in RCDI but heterogeneity in treatment duration and dose precludes robust conclusions. Fidaxomicin may have a role in treatment, but evidence is limited to subgroup analyses. Fecal bacteriotherapy was the most efficacious. Saccharomyces boulardii may have a role as adjunctive treatment.


Similar content being viewed by others
References
Lo Vecchio A, Zacur GM. Clostridium difficile infection: an update on epidemiology, risk factors, and therapeutic options. Curr Opin Gastroenterol. 2012;28:1–9.
Warny M, Pepin J, Fang A, Killgore G, Thompson A, Brazier J, et al. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet. 2005;366:1079–84. doi:10.1016/S0140-6736(05)67420-X.
McDonald LC, Killgore GE, Thompson A, Owens RC Jr, Kazakova SV, Sambol SP, et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353:2433–41. doi:10.1056/NEJMoa051590.
Pepin J, Alary M-E, Valiquette L, Raiche E, Ruel J, Fulop K, et al. Increasing risk of relapse after treatment of Clostridium difficile colitis in Quebec, Canada. Clin Infect Dis. 2005;40:1591–7.
Wenisch JM, Schmid D, Tucek G, Kuo HW, Allerberger F, Michl V, et al. A prospective cohort study on hospital mortality due to Clostridium difficile infection. Infection. 2012;40:479–84. doi:10.1007/s15010-012-0258-1.
Razavi B, Apisarnthanarak A, Mundy LM. Clostridium difficile: emergence of hypervirulence and fluoroquinolone resistance. Infection. 2007;35:300–7. doi:10.1007/s15010-007-6113-0.
Johnson S. Recurrent Clostridium difficile infection: a review of risk factors, treatments, and outcomes. J Infect. 2009;58:403–10.
Ghantoji SS, Sail K, Lairson DR, DuPont HL, Garey KW. Economic healthcare costs of Clostridium difficile infection: a systematic review. J Hosp Infect. 2010;74:309–18.
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010;31:431–55. doi:10.1086/651706.
Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22:128; author reply 128. doi:10.1097/EDE.0b013e3181fe7825.
Mezoff E, Mann EA, Hart KW, Lindsell CJ, Cohen MB. Clostridium difficile infection and treatment in the pediatric inflammatory bowel disease population. J Pediatr Gastroenterol Nutr. 2011;52:437–41.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84.
Tedesco FJ, Gordon D, Fortson WC. Approach to patients with multiple relapses of antibiotic-associated pseudomembranous colitis. Am J Gastroenterol. 1985;80:867–8.
Shetler K, Nieuwenhuis R, Wren SM, Triadafilopoulos G. Decompressive colonoscopy with intracolonic vancomycin administration for the treatment of severe pseudomembranous colitis. Surg Endosc. 2001;15:653–9. doi:10.1007/s004640080104.
McFarland LV, Elmer GW, Surawicz CM. Breaking the cycle: treatment strategies for 163 cases of recurrent Clostridium difficile disease. Am J Gastroenterol. 2002;97:1769–75.
Pépin J, Routhier S, Gagnon S, Brazeau I. Management and outcomes of a first recurrence of Clostridium difficile-associated disease in Quebec, Canada. Clin Infect Dis. 2006;42:758–64. doi:10.1086/501126.
Surawicz CM, McFarland LV, Greenberg RN, Rubin M, Fekety R, Mulligan ME, et al. The search for a better treatment for recurrent Clostridium difficile disease: use of high-dose vancomycin combined with Saccharomyces boulardii. Clin Infect Dis. 2000;31:1012–7. doi:10.1086/318130.
Basu PP, Shah NJ, Krishnaswamy N, Korapati R, Tang C, Pacana T. Sequential use of nitazoxanide (NTZ) as a salvage therapy in patient with recurrent mild to moderate Clostridium difficile infection (CDI): a prospective, open-label, randomized clinical trial. Am J Gastroenterol. 2010;105:S142
Louie TJ, Miller MA, Mullane KM, Weiss K, Lentnek A, Golan Y, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med. 2011;364:422–31. doi:10.1056/NEJMoa0910812.
Cornely OA, Miller MA, Louie TJ, Crook DW, Gorbach SL. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis. 2012;55:S154–61. doi:10.1093/cid/cis462.
Musher DM, Logan N, Bressler AM, Johnson DP, Rossignol J-F. Nitazoxanide versus vancomycin in Clostridium difficile infection: a randomized, double-blind study. Clin Infect Dis. 2009;48:e41–6.
van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–15. doi:10.1056/NEJMoa1205037.
Drekonja DM, Butler M, MacDonald R, Bliss D, Filice GA, Rector TS, et al. Comparative effectiveness of Clostridium difficile treatments: a systematic review. Ann Intern Med. 2011;155:839–47.
Cohen MD. Quality assurance: potential use for the newly described exposure index in clinical practice. J Am Coll Radiol. 2010;7:748–9. doi:10.1016/j.jacr.2010.04.008.
Mattila E, Anttila VJ, Broas M, Marttila H, Poukka P, Kuusisto K, et al. A randomized, double-blind study comparing Clostridium difficile immune whey and metronidazole for recurrent Clostridium difficile-associated diarrhoea: efficacy and safety data of a prematurely interrupted trial. Scand J Infect Dis. 2008;40:702–8. doi:10.1080/00365540801964960.
Wullt M, Hagslätt MLJ, Odenholt I. Lactobacillus plantarum 299v for the treatment of recurrent Clostridium difficile-associated diarrhoea: a double-blind, placebo-controlled trial. Scand J Infect Dis. 2003;35:365–7. doi:10.1080/00365540310010985.
Baines SD, O’Connor R, Freeman J, Fawley WN, Harmanus C, Mastrantonio P, et al. Emergence of reduced susceptibility to metronidazole in Clostridium difficile. J Antimicrob Chemother. 2008;62:1046–52.
Musher DM, Logan N, Mehendiratta V, Melgarejo NA, Garud S, Hamill RJ. Clostridium difficile colitis that fails conventional metronidazole therapy: response to nitazoxanide. J Antimicrob Chemother. 2007;59:705–10. doi:10.1093/jac/dkl553.
Buggy BP, Fekety R, Silva J Jr. Therapy of relapsing Clostridium difficile-associated diarrhea and colitis with the combination of vancomycin and rifampin. J Clin Gastroenterol. 1987;9:155–9.
Berman AL. Efficacy of rifaximin and vancomycin combination therapy in a patient with refractory Clostridium difficile-associated diarrhea. J Clin Gastroenterol. 2007;41:932–3. doi:10.1097/01.mcg.0000225685.37465.e7.
Johnson S, Schriever C, Galang M, Kelly CP, Gerding DN. Interruption of recurrent Clostridium difficile-associated diarrhea episodes by serial therapy with vancomycin and rifaximin. Clin Infect Dis. 2007;44:846–8. doi:10.1086/511870.
Garey KW, Jiang ZD, Bellard A, Dupont HL. Rifaximin in treatment of recurrent Clostridium difficile-associated diarrhea: an uncontrolled pilot study. J Clin Gastroenterol. 2009;43:91–3. doi:10.1097/MCG.0b013e31814a4e97.
Johnson S, Schriever C, Patel U, Patel T, Hecht DW, Gerding DN. Rifaximin Redux: treatment of recurrent Clostridium difficile infections with rifaximin immediately post-vancomycin treatment. Anaerobe. 2009;15:290–1.
Neff G, Zacharias V, Kaiser TE, Gaddis A, Kemmer N. Rifaximin for the treatment of recurrent Clostridium difficile infection after liver transplantation: a case series. Liver Transpl. 2010;16:960–3. doi:10.1002/lt.22092.
Basu PP, Dinani A, Rayapudi K, Pacana T, Shah NJ, Hampole H, et al. Rifaximin therapy for metronidazole-unresponsive Clostridium difficile infection: a prospective pilot trial. Ther Adv Gastroenterol. 2010;3:221–5. doi:10.1177/1756283X10372985.
Musher DM, Logan N, Hamill RJ, Dupont HL, Lentnek A, Gupta A, et al. Nitazoxanide for the treatment of Clostridium difficile colitis. Clin Infect Dis. 2006;43:421–7. doi:10.1086/506351.
Louie TJ, Cannon K, Byrne B, Emery J, Ward L, Eyben M, et al. Fidaxomicin preserves the intestinal microbiome during and after treatment of Clostridium difficile infection (CDI) and reduces both toxin reexpression and recurrence of CDI. Clin Infect Dis. 2012;55:S132–42. doi:10.1093/cid/cis338.
Venugopal AA, Johnson S. Fidaxomicin: a novel macrocyclic antibiotic approved for treatment of Clostridium difficile infection. Clin Infect Dis. 2012;54:568–74.
Lowy I, Molrine DC, Leav BA, Blair BM, Baxter R, Gerding DN, et al. Treatment with monoclonal antibodies against Clostridium difficile toxins. N Engl J Med. 2010;362:197–205. doi:10.1056/NEJMoa0907635.
Leung DY, Kelly CP, Boguniewicz M, Pothoulakis C, LaMont JT, Flores A. Treatment with intravenously administered gamma globulin of chronic relapsing colitis induced by Clostridium difficile toxin. J Pediatr. 1991;118:633–7.
Salcedo J, Keates S, Pothoulakis C, Warny M, Castagliuolo I, LaMont JT, et al. Intravenous immunoglobulin therapy for severe Clostridium difficile colitis. Gut. 1997;41:366–70.
Beales IL. Intravenous immunoglobulin for recurrent Clostridium difficile diarrhoea. Gut. 2002;51:456.
Wilcox MH. Descriptive study of intravenous immunoglobulin for the treatment of recurrent Clostridium difficile diarrhoea. J Antimicrob Chemother. 2004;53:882–4. doi:10.1093/jac/dkh176.
McPherson S, Rees CJ, Ellis R, Soo S, Panter SJ. Intravenous immunoglobulin for the treatment of severe, refractory, and recurrent Clostridium difficile diarrhea. Dis Colon Rectum. 2006;49:640–5. doi:10.1007/s10350-006-0511-8.
Jiang ZD, Garey KW, Price M, Graham G, Okhuysen P, Dao-Tran T, et al. Association of interleukin-8 polymorphism and immunoglobulin G anti-toxin A in patients with Clostridium difficile-associated diarrhea. Clin Gastroenterol Hepatol. 2007;5:964–8. doi:10.1016/j.cgh.2007.04.018.
Aslam S, Hamill RJ, Musher DM. Treatment of Clostridium difficile-associated disease: old therapies and new strategies. Lancet Infect Dis. 2005;5:549–57. doi:10.1016/S1473-3099(05)70215-2.
O’Horo J, Safdar N. The role of immunoglobulin for the treatment of Clostridium difficile infection: a systematic review. Int J Infect Dis. 2009;13:663–7. doi:10.1016/j.ijid.2008.11.012.
Yazdankhah S, Midtvedt T, Narvhus J, Berstad A, Lassen J, Halvorsen R. The use of probiotics for critically ill patients in hospitals. Microb Ecol Health Dis. 2009;21:114–21. doi:10.3109/08910600903495046.
O’Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006;7:688–93. doi:10.1038/sj.embor.7400731.
Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, et al. Enterotypes of the human gut microbiome. Nature. 2011;473:174–80. doi:10.1038/nature09944.
D’Souza AL, Rajkumar C, Cooke J, Bulpitt CJ. Probiotics in prevention of antibiotic associated diarrhoea: meta-analysis. BMJ. 2002;324:1361.
McFarland LV, Surawicz CM, Greenberg RN, Fekety R, Elmer GW, Moyer KA, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA. 1994;271:1913–8.
Elmer GW, McFarland LV, Surawicz CM, Danko L, Greenberg RN. Behaviour of Saccharomyces boulardii in recurrent Clostridium difficile disease patients. Aliment Pharmacol Ther. 1999;13:1663–8.
Surawicz CM, McFarland LV, Elmer G, Chinn J. Treatment of recurrent Clostridium difficile colitis with vancomycin and Saccharomyces boulardii. Am J Gastroenterol. 1989;84:1285–7.
Gorbach SL, Chang TW, Goldin B. Successful treatment of relapsing Clostridium difficile colitis with Lactobacillus GG. Lancet. 1987;2:1519.
Biller JA, Katz AJ, Flores AF, Buie TM, Gorbach SL. Treatment of recurrent Clostridium difficile colitis with Lactobacillus GG. J Pediatr Gastroenterol Nutr. 1995;21:224–6.
Seal D, Borriello SP, Barclay F, Welch A, Piper M, Bonnycastle M. Treatment of relapsing Clostridium difficile diarrhoea by administration of a non-toxigenic strain. Eur J Clin Microbiol. 1987;6:51–3.
Miller M. The fascination with probiotics for Clostridium difficile infection: lack of evidence for prophylactic or therapeutic efficacy. Anaerobe. 2009;15:281–4.
Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958;44:854–9.
Bakken JS, Borody T, Brandt LJ, Brill JV, Demarco DC, Franzos MA, et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastroenterol Hepatol. 2011;9:1044–9.
Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis. 2011;53:994–1002.
Postigo R, Kim JH. Colonoscopic versus nasogastric fecal transplantation for the treatment of Clostridium difficile infection: a review and pooled analysis. Infection. 2012;40:643–8. doi:10.1007/s15010-012-0307-9.
Maire F. La transplantation fécale: Un traitement d’avenir de la colite à Clostridium difficile? [Fecal transplantation: new therapy for recurrent Clostridium difficile infection?]. Hépato-Gastro. 2012;19:285–8. doi:10.1684/hpg.2012.0710.
Polák P, Freibergerová M, Juránková J, Kocourková H, Mikešová L, Svačina R, et al. První zkušenosti s fekální bakterioterapií v léčbě relabující pseudomembranózní kolitidy způsobené Clostridium difficile [First experiences with faecal bacteriotherapy in the treatment of relapsing pseudomembranous colitis due to Clostridium difficile]. Klin Mikrobiol Infekc Lek. 2011;17:214–7.
Schwan A, Sjölin S, Trottestam U, Aronsson B. Relapsing Clostridium difficile enterocolitis cured by rectal infusion of normal faeces. Scand J Infect Dis. 1984;16:211–5.
Persky SE, Brandt LJ. Treatment of recurrent Clostridium difficile-associated diarrhea by administration of donated stool directly through a colonoscope. Am J Gastroenterol. 2000;95:3283–5. doi:10.1111/j.1572-0241.2000.03302.x.
Hellemans R, Naegels S, Holvoet J. Fecal transplantation for recurrent Clostridium difficile colitis, an underused treatment modality. Acta Gastroenterol Belg. 2009;72:269–70.
Khoruts A, Dicksved J, Jansson JK, Sadowsky MJ. Changes in the composition of the human fecal microbiome after bacteriotherapy for recurrent Clostridium difficile-associated diarrhea. J Clin Gastroenterol. 2010;44:354–60. doi:10.1097/MCG.0b013e3181c87e02.
Russell G, Kaplan J, Ferraro M, Michelow IC. Fecal bacteriotherapy for relapsing Clostridium difficile infection in a child: a proposed treatment protocol. Pediatrics 2010;126:e239–42. doi:10.1542/peds.2009-3363.
Fløtterød O, Hopen G. Refractory Clostridium difficile infection. Untraditional treatment of antibiotic-induced colitis. Tidsskr Nor Laegeforen. 1991;111:1364–5.
Härkönen N. Uusiutuneen pseudomembranoottisen koliitin hoito ulosteensiirrolla [Recurrent pseudomembranous colitis treated with the donor feces]. Duodecim. 1996;112:1803–4.
Tvede M, Rask-Madsen J. Bacteriotherapy for chronic relapsing Clostridium difficile diarrhoea in six patients. Lancet. 1989;1:1156–60.
Paterson DL, Iredell J, Whitby M. Putting back the bugs: bacterial treatment relieves chronic diarrhoea. Med J Aust. 1994;160:232–3.
Faust G, Langelier D, Haddad H, Menard DB. Treatment of recurrent pseudomembranous colitis with stool transplantation: report of six cases. Can J Gastroenterol. 2002;16:A43.
Aas J, Gessert CE, Bakken JS. Recurrent Clostridium difficile colitis: case series involving 18 patients treated with donor stool administered via a nasogastric tube. Clin Infect Dis. 2003;36:580–5.
Jorup-Rönström C, Håkanson A, Persson AK, Midtvedt T, Norin E. Feceskultur framgångsrik terapi vid Clostridium difficile-diarré. Lakartidningen. 2006;103:3603–5.
Wettstein A, Borody T, Leis S, Chongnan J, Torres M, Hindler JF. Fecal bacteriotherapy—an effective treatment for relapsing symptomatic Clostridium difficile infection. In: 15th United European Gastroenterology Week 2007; France 2007.
Louie T, Louie MR, Krulicki W, Byrne B, Ward L. Home-based fecal flora infusion to arrest multiply-recurrent Clostridium difficile infection. In: 48th Interscience Conference on Antimicrobial Agents and Chemotherapy; Arlington, VA: Infectious Disease Society of America; 2008.
MacConnachie AA, Fox R, Kennedy DR, Seaton RA. Faecal transplant for recurrent Clostridium difficile-associated diarrhoea: a UK case series. QJM. 2009;102:781–4. doi:10.1093/qjmed/hcp118.
Garborg K, Waagsbø B, Stallemo A, Matre J, Sundøy A. Results of faecal donor instillation therapy for recurrent Clostridium difficile-associated diarrhoea. Scand J Infect Dis. 2010;42:857–61. doi:10.3109/00365548.2010.499541.
Kelly C, de Leon L. Successful treatment of recurrent Clostridium difficile infection with donor stool administered at colonoscopy: a case series. Am J Gastroenterol. 2010;105:S135; abstract 366
Mellow MH, Kanatzar A. Colonoscopic fecal bacteriotherapy in the treatment of recurrent Clostridium difficile infection—results and follow-up. Am J Gastroenterol. 2010;105:S135
Miller CB, Dellon E, Isaacs K, Gangarosa L. Fecal bacteriotherapy via colonoscopy as rescue therapy for refractory and recurrent Clostridium difficile-associated diarrhea. Am J Gastroenterol. 2010;105:S323
Rohlke F, Surawicz CM, Stollman N. Fecal flora reconstitution for recurrent Clostridium difficile infection: results and methodology. J Clin Gastroenterol. 2010;44:567–70.
Silverman MS, Davis I, Pillai DR. Success of self-administered home fecal transplantation for chronic Clostridium difficile infection. Clin Gastroenterol Hepatol. 2010;8:471–3. doi:10.1016/j.cgh.2010.01.007.
Yoon SS, Brandt LJ. Treatment of refractory/recurrent C. difficile-associated disease by donated stool transplanted via colonoscopy: a case series of 12 patients. J Clin Gastroenterol. 2010;44:562–6.
Brandt LJ, Aroniadis OC, Mellow M, Kanatzar A, Kelly C, Park T, et al. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107:1079–87. doi:10.1038/ajg.2012.60.
Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012;107:761–7. doi:10.1038/ajg.2011.482.
Jorup-Rönström C, Håkanson A, Sandell S, Edvinsson O, Midtvedt T, Persson AK, et al. Fecal transplant against relapsing Clostridium difficile-associated diarrhea in 32 patients. Scand J Gastroenterol. 2012;47:548–52. doi:10.3109/00365521.2012.672587.
Kassam Z, Hundal R, Marshall JK, Lee CH. Fecal transplant via retention enema for refractory or recurrent Clostridium difficile infection. Arch Intern Med. 2012;172:191–3. doi:10.1001/archinte.172.2.191.
Kelly CR, de Leon L, Jasutkar N. Fecal microbiota transplantation for relapsing Clostridium difficile infection in 26 patients: methodology and results. J Clin Gastroenterol. 2012;46:145–9.
Mattila E, Uusitalo-Seppälä R, Wuorela M, Lehtola L, Nurmi H, Ristikankare M, et al. Fecal transplantation, through colonoscopy, is effective therapy for recurrent Clostridium difficile infection. Gastroenterology. 2012;142:490–6.
Mellow MH, Kanatzar A. Colonoscopic fecal bacteriotherapy in the treatment of recurrent Clostridium difficile infection—results and follow-up. J Okla State Med Assoc. 2011;104:89–91.
Lund-Tønnesen S, Berstad A, Schreiner A, Midtvedt T. Clostridium difficile-assosiert diare behandlet med homolog feces [Clostridium difficile-associated diarrhoea treated with homologous faeces]. Tidsskr Nor Laegeforen. 1998;118:1027–30.
Liacouras CA, Piccoli DA. Whole-bowel irrigation as an adjunct to the treatment of chronic, relapsing Clostridium difficile colitis. J Clin Gastroenterol. 1996;22:186–9.
Herpers BL, Vlaminckx B, Burkhardt O, Blom H, Biemond-Moeniralam HS, Hornef M, et al. Intravenous tigecycline as adjunctive or alternative therapy for severe refractory Clostridium difficile infection. Clin Infect Dis. 2009;48:1732–5. doi:10.1086/599224.
Louie TJ, Peppe J, Watt CK, Johnson D, Mohammed R, Dow G, et al. Tolevamer, a novel nonantibiotic polymer, compared with vancomycin in the treatment of mild to moderately severe Clostridium difficile-associated diarrhea. Clin Infect Dis. 2006;43:411–20. doi:10.1086/506349.
Barker RH Jr, Dagher R, Davidson DM, Marquis JK. Review article: tolevamer, a novel toxin-binding polymer: overview of preclinical pharmacology and physicochemical properties. Aliment Pharmacol Ther. 2006;24:1525–34.
Dubberke E. Strategies for prevention of Clostridium difficile infection. J Hosp Med. 2012;7:S14–7. doi:10.1002/jhm.1908.
Centers for Disease Control and Prevention (CDC). Vital signs: preventing Clostridium difficile infections. MMWR Morb Mortal Wkly Rep. 2012;61:157–62.
Tedesco FJ, Barton RW, Alpers DH. Clindamycin-associated colitis. A prospective study. Ann Intern Med. 1974;81:429–33.
Gerding DN, Johnson S, Peterson LR, Mulligan ME, Silva J Jr. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995;16:459–77
Hassett J, Meyers S, McFarland L, Mulligan ME. Recurrent Clostridium difficile infection in a patient with selective IgG1 deficiency treated with intravenous immune globulin and Saccharomyces boulardii. Clin Infect Dis. 1995;20:S266–68. doi:10.1093/clinids/20.Supplement_2.S266
Murphy C, Vernon M, Cullen M. Intravenous immunoglobulin for resistant Clostridium difficile infection. Age Ageing. 2006;35:85–86. doi:10.1093/ageing/afi212
Hassoun A, Ibrahim F. Use of intravenous immunoglobulin for the treatment of severe Clostridium difficile colitis. Am J Geriatr Pharmacother. 2007;5:48–51. doi:10.1016/j.amjopharm.2007.03.001
Acknowledgments
The authors would like to thank librarian Mona K. Stevermer for her assistance with the literature search.
Conflict of interest
None of the authors have any relevant conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
O’Horo, J.C., Jindai, K., Kunzer, B. et al. Treatment of recurrent Clostridium difficile infection: a systematic review. Infection 42, 43–59 (2014). https://doi.org/10.1007/s15010-013-0496-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-013-0496-x