Abstract
Background
Voluntary knuckle cracking is a common habit, with a reported prevalence of 25% to 45%. Habitual knuckle cracking also is a frequent source of questions for physicians, and the largest study to date reported an association with functional hand impairments.
Questions/purposes
(1) When compared with subjects who are not habitual knuckle crackers, do habitual knuckle crackers have greater QuickDASH scores, swelling, weakness, joint laxity, or ROM? (2) In subjects who crack their knuckles, does cracking immediately increase ROM? (3) What are the characteristic sonographic findings in joints that crack?
Methods
A prospective, institutional review board-approved study was performed on 400 metacarpophalangeal joints (MPJs) in 40 asymptomatic adult subjects. Of those, 30 subjects had a history of habitual knuckle cracking (defined as daily voluntary popping of MPJs). Clinical history provided by all subjects included a standardized QuickDASH questionnaire. Physical examination was performed by two orthopaedic surgeons (blinded to subjects’ knuckle-cracking history and sonographic outcomes). The physical examination included evaluation for swelling, grip strength, and ROM before and after attempted knuckle cracking. Sonographic examination was conducted by one sonographer, with static and real-time cine images recorded before, during, and after MPJ distraction was performed by the subjects. Two musculoskeletal radiologists (blinded to subjects’ knuckle-cracking history) interpreted the images for a definite hyperechoic focus during and after MPJ distraction; this was compared against the reference standard of an audible “crack” during joint distraction.
Results
Comparing subjects with knuckle cracking with those who did not crack their knuckles, there was no differences in QuickDASH scores (knuckle crackers, 3.7 ± 5.2; nonknuckle crackers, 3.2 ± 6.3; mean difference, 0.6; 95% CI, −3.5 to 4.6; p = 0.786), laxity (knuckle crackers, 2.0 ± 1.8; nonknuckle crackers, 0.3 ± 0.7; mean difference, 1.7; 95% CI, 0.5–2.9; p = 0.191), and grip strength (preultrasound, right hand, p = 0.499, left hand p = 0.575; postultrasound, right hand p = 0.777, left hand p = 0.424); ROM comparisons between subjects with a history of habitual knuckle cracking versus subjects without such a history only yielded increased ROM in joints that cracked during manipulation (knuckle cracking, 143.8° ± 26.5°; nonknuckle cracking, 134.9° ± 28.6°; mean difference, 9.0°; 95% CI, 2.9°–15.1°; p = 0.004). Swelling was not observed in any subjects, including when comparing MPJs before versus after distraction maneuvers that resulted in audible cracks. Immediately after a documented crack, there were greater ranges of motion with active flexion (preultrasound, 85.7° ± 12.4°; postultrasound, 88.6° ± 11.6°; mean difference, −2.9°; 95% CI, −5.1° to −0.8°; p = 0.009), passive flexion (preultrasound, 96.1° ± 12.4°; postultrasound, 100.3° ± 10.4°; mean difference, −4.3°; 95% CI, −6.2° to −2.3°; p < 0.001), passive extension (preultrasound, 41.8° ± 18.1°; postultrasound, 45.2° ± 17.6°; mean difference, −3.5°; 95% CI, −6.9° to −0.1°; p = 0.046), and passive total ROM (preultrasound, 137.8° ± 24.8°; postultrasound, 145.6° ± 23.1°; mean difference, −7.7°; 95% CI, −11.7° to −3.8°; p < 0.001). The characteristic sonographic finding observed during cracking events is an echogenic focus that appears de novo dynamically in the joint during distraction.
Conclusions
We found no evidence of immediate adverse physical examination findings after knuckle cracking. However, we did find a small increase in ROM among joints that cracked compared with those that did not. Future studies should examine if there are any long-term beneficial and adverse clinical outcomes associated with habitual knuckle cracking.
Level of Evidence
Level I, prognostic study.
Similar content being viewed by others
Introduction
Voluntary knuckle cracking is a common habit, with a reported prevalence of 25% [4] to 45% [22] in the United States. Habitual knuckle cracking also is a frequent source of questions for physicians, and controversies persist regarding any pathophysiology associated with knuckle cracking. For example, some investigators [6] suggest that only joints with sufficient laxity will crack, whereas another investigator [3] argued that joints that are too lax or too tight will not be able to perform an articular pop. With voluntary knuckle cracking in asymptomatic individuals, numerous theories have been advanced to explain the physiologic process, including sudden springing apart of the bones causing tissue vibrations [18], sudden tightening of the joint capsule [12], snapping back of the joint capsule [3], lysis of intraarticular adhesions [16], collapse of intraarticular gas bubbles [23], and formation of intraarticular gas bubbles [10].
In the largest study to date [4], clinical evaluation found habitual knuckle cracking is associated strongly with hand swelling and lower grip strength, and concluded habitual knuckle cracking “results in functional hand impairment”. Another author, without presenting data, offered the opinion that knuckle cracking is not deleterious, but concluded that “it is time we really found out” [20]. Imaging may be used as a noninvasive means of documenting the anatomic source of a sudden sound at the metacarpophalangeal joints (MPJ) (eg, knuckle cracking), but little is known about the real-time sonographic findings of this dynamic phenomenon. Thus, we were motivated to investigate if knuckle cracking is associated with observable differences in clinical history, physical examination, and dynamic sonographic findings.
Therefore, we asked: (1) When compared with subjects without a history of habitual knuckle cracking, do subjects with habitual knuckle cracking have greater QuickDASH scores, swelling, grip weakness, joint laxity, or ROM? (2) In subjects with a history of knuckle cracking, does cracking immediately increase ROM? (3) What are the characteristic sonographic findings in joints that crack?
Materials and Methods
Volunteers were recruited for this prospective study without any remuneration, compliant with the Health Insurance Portability and Accountability Act, by posting announcements at a university medical center between September 13, 2014 and February 6, 2015. Written informed consent was obtained for each volunteer based on the guidelines and approved documentation from our university institutional review board before study initiation. Inclusion criteria for this study included subjects with no history of joint problems in their hands, and 18 years or older. Forty subjects were enrolled on a first-come, first-served basis and identified themselves as either performing daily, voluntary (“habitual”) knuckle cracking or as never voluntarily performing knuckle cracking.
Thirty subjects with a history of habitual knuckle cracking and 10 without a history of habitual knuckle cracking were included, each with 10 digits, resulting in evaluation of 400 MPJs. There were no differences in age, gender distribution, and hand dominance between the two groups (Table 1). Interestingly, compared with subjects in the group without a history of habitual knuckle cracking, more subjects in the habitual knuckle cracking group reported that they also engaged in habitual cracking of other joints in their body (in addition to those in the hand) (23/30 [77%] versus 3/10 [30%]).
Clinical History
In addition to demographic traits (including gender, age, hand dominance), each subject completed the standardized QuickDASH outcome measure questionnaire [7].
Physical Examination
Subjects were randomly assigned to and underwent a detailed physical examination of both hands by one of two hand-specialty trained orthopaedic surgeons (RMS, APN). The surgeons were completely blinded to any history of knuckle cracking among the subjects. Before starting the study both orthopaedists created, by consensus, a document detailing the method of performing the individual ROM measurements.
Clinical assessment for swelling, grip strength, and ROM was performed promptly (< 5 minutes) before and after performing distraction maneuvers on the MPJs (as detailed in the Statistical Analysis below). Swelling was assessed as present or absent by the orthopaedic examiners. Grip strength was measured using a calibrated digital handheld dynamometer (Jamar; Lafayette Instrument Company, Lafayette, IN, USA), with the average of three maximal isometric efforts recorded (in pounds) [1, 21]. Active and passive ROM measurements were recorded (in degrees) during flexion and extension of the MPJs using a manual goniometer.
Additionally, after performing distraction maneuvers on the MPJs, assessment for hypermobility or “laxity” was performed using the 0- to 9-point Beighton scale, with scores of 4 or greater considered indicative of laxity [17]. The Beighton score is calculated by adding 1 point for each of the following: placing flat hands on the floor with straight legs; each elbow that bends backward; each knee that bends backward; each thumb that touches the forearm when bent; and each small finger that bends backward beyond 90°.
Sonographic Evaluation
Sonography was performed by a musculoskeletal sonographer (MC) (with 25 years of experience) using a dedicated ultrasound unit (LOGIQTM E9; GE Healthcare, Milwaukee, WI, USA) with the linear array L8-18i “hockey stick” probe operated at 18 MHz, with a temporal resolution of 87 and 232 frames per second.
Subjects were instructed to abstain from knuckle cracking for at least 4 hours preceding the examination. Subjects with and without a history of habitual knuckle cracking were examined while in the seated position with hands on a height-adjustable stand. The MPJs were examined sonographically in the longitudinal plane before, during, and after each MPJ was distracted manually with longitudinal traction, hyperflexion, or hyperextension by the subject. In addition to static images immediately (< 20 seconds) before and after distraction of the MPJ, real-time cine images were obtained dynamically during the distraction maneuver.
For each MPJ, an independent observer (RDB) (musculoskeletal radiologist with 19 years of experience) in the room recorded if a definite audible crack did or did not occur during the distraction maneuver. This served as the reference standard for evaluating the accuracy of sonographic observations by two readers.
The findings observed during sonographic imaging were analyzed independently by two musculoskeletal radiologists (DN, CB) (with one in fellowship training and one with 3 years in clinical practice). Both readers were blinded to whether the subjects had any history of habitual knuckle cracking and whether the subjects cracked their knuckles during the sonographic examination.
In joints that cracked, sonography showed hyperechoic foci, suggesting the formation of intraarticular gas. In contrast, this finding was not observed in association with the distraction maneuvers that did not result in a joint crack. These findings corroborate existing studies [9, 11]. Thus, sonographic examinations were interpreted as positive for showing knuckle cracking if new echogenic foci appeared either during real-time cine images during distraction or on static images immediately after distraction (Fig. 1). Conversely, sonographic examinations were interpreted as showing no crack if no echogenic foci appeared in the joint during real-time cine imaging during distraction and on static imaging immediately after distraction (Fig. 2).
Longitudinal sonographic examinations were interpreted as “positive” for showing knuckle cracking if a new echogenic focus (arrow) appeared in the metacarpophalangeal joint (between the metacarpal [MC] and the proximal phalanx [PP]) during real-time cine images during distraction or on static images immediately after distraction.
Longitudinal sonographic examinations were interpreted as “no crack” if no echogenic focus (arrow) appeared in the metacarpophalangeal joint (between the metacarpal [MC] head and the proximal phalanx [PP]) with real-time cine imaging during distraction or on static images immediately after distraction.
Statistical Analysis
Comparisons were made between subjects with a history of habitual knuckle cracking versus subjects without a history of habitual knuckle cracking across numerous variables to determine differences between groups. In addition, comparisons were made between joints that had a documented crack event during the distraction maneuver and joints that did not crack during the distraction maneuver our study. A chi-square test was used for categorical variables whereas an independent two-sided Student’s t-test was used for continuous variables. A p value less than 0.05 was considered statistically significant. A power analysis was performed on one of the primary endpoints, QuickDASH scores. A sample size of 3436 (α = 0.05, β = 0.80) would be required to detect a difference with an effect size of 0.10.
Results
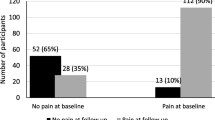
Comparing subjects with a history of habitual knuckle cracking with subjects without such a history, with the numbers available, there were no differences in QuickDASH scores (knuckle crackers, 3.7 ± 5.2; nonknuckle crackers, 3.2 ± 6.3; mean difference, 0.6; 95% CI, −3.5 to 4.6; p = 0.786), laxity (knuckle crackers, 2.0 ± 1.8; nonknuckle crackers, 0.3 ± 0.7; mean difference, 1.7; 95% CI, 0.5–2.9; p = 0.191), and grip strength (preultrasound, right hand, p = 0.499, left hand p = 0.575; postultrasound, right hand p = 0.777, left hand; p = 0.424) (Table 2). Although we found a small difference in QuickDASH scores between subjects with knuckle cracking and those without for sports activities, all results were within the normal range. Furthermore, when limiting the Beighton score to the hand components (that is, small finger hyperextension greater than 90° and thumb hyperextension to volar forearm), no differences were observed (knuckle crackers, 1.1 ± 1.2; nonknuckle crackers, 0.2 ± 0.4; mean difference, 0.9; 95% CI, 0.1–1.7; p = 0.202). ROM comparisons between subjects with a history of habitual knuckle cracking versus without such a history only yielded increased ROM in knuckle crackers after ultrasound recorded manipulation (knuckle cracking 143.8° ± 26.5°; nonknuckle cracking 134.9° ± 28.6°; mean difference, 9.0°; 95% CI, 2.9°–15.1°, p = 0.004) (Table 2). Swelling was not observed in any subjects, including habitual knuckle crackers before or after MPJ distraction maneuvers that resulted in audible cracks. More subjects in the habitual knuckle cracking group (23/30 [77%]) reported habitual cracking of other joints, compared with those in the nonknuckle cracking group (3/10 [30%]; p = 0.007). Increased ROM was found immediately after distraction events in 62 of the 400 MPJs successfully discharging an audible crack; in particular, there were greater ranges of motion with active flexion (preultrasound, 85.7° ± 12.4°; postultrasound, 88.6° ± 11.6°; mean difference, −2.9o; 95% CI, −5.1o to −0.8o; p = 0.009), passive flexion (preultrasound, 96.1° ± 12.4°; postultrasound, 100.3° ± 10.4°; mean difference, −4.3°; 95% CI, −6.2° to −2.3°; p < 0.001), passive extension (preultrasound, 41.8° ± 18.1°; postultrasound, 45.2° ± 17.6°; mean difference, −3.5°; 95% CI, −6.9° to −0.1°; p = 0.046), and passive total ROM (preultrasound, 137.8° ± 24.8°; postultrasound, 145.6° ± 23.1°; mean difference, −7.7°; 95% CI, −11.7° to −3.8°; p < 0.001) after documented joint cracking occurred during MPJ distraction (Table 3).
Of the knuckles that cracked during distraction maneuvers, (50/62 [81%]) showed positive findings on sonography. Conversely, of the knuckles that did not crack when the joint was distracted, (321/338 [95%]) showed no positive findings on sonography.
Discussion
Principal findings of this study relate to the clinical history, physical examination, and sonographic evaluation of subjects with and without knuckle cracking. Habitual voluntary knuckle cracking is a frequent source of questions for physicians, and controversies persist regarding any pathophysiology associated with knuckle cracking. We investigated the understudied question regarding whether subjects who perform habitual knuckle cracking have greater QuickDASH scores, swelling, grip strength, joint laxity, or ROM of the MPJs compared with those without a history of habitual knuckle cracking, and characterized the dynamic sonographic findings in joints that crack. We were unable to identify differences between the QuickDASH scores, swelling, grip strength, and laxity in subjects who were habitual knuckle crackers versus those who were nonknuckle crackers. However, we did find increased ROM in joints immediately after they cracked, although this change was small. With dynamic sonography, the characteristic finding during knuckle cracking was a sudden hyperechoic flash appearing de novo in the joint.
Our study has several limitations. First, we studied a small cross-sectional cohort of relatively young asymptomatic adults; it was not our intent to study the long-term longitudinal outcomes of subjects with habitual knuckle cracking versus those without knuckle cracking. Therefore, our study is not designed to assess the potential role of knuckle cracking in the development of conditions such as arthritis. It is conceivable that the cumulative long-term effects of knuckle cracking “microtrauma” could result in adverse articular sequelae. Second, because of our method of volunteer recruitment, there was likely an enrollment bias favoring subjects with a history of habitual knuckle cracking. Third, our reference standard of an audible crack, although adequate, did not allow for histologic analysis of intraarticular findings. Furthermore, we recognize that the lack of perfect concordance between an audible crack and sonographic findings may have occurred owing to decentering of the ultrasound probe during the distraction maneuver. However, we believe that the hyperechoic cloudlike area that appeared sonographically in cracking joints does represent intraarticular gas formation owing to tribonucleation [8, 10, 25].
Subjects with a history of habitual knuckle cracking did not have more disability or swelling than subjects without a history of knuckle cracking. Furthermore, in blinded analysis comparing joints that cracked versus those that did not, we found no adverse outcomes of swelling or decreased grip strength. This is potentially important because of the concern for adverse sequelae among many people who crack their knuckles. No prior studies, to our knowledge, have looked for (and not found) upper extremity disability using a validated standardized scoring instrument. Our findings differ sharply from those of the largest study to date [4], which evaluated 300 subjects (74 subjects with knuckle cracking versus 226 without knuckle cracking). Although those investigators did not find any association of habitual knuckle cracking with osteoarthritis, they reported that habitual knuckle cracking was strongly associated with hand swelling and weaker grip strength, and concluded that habitual knuckle cracking “results in functional hand impairment” and “should be discouraged”. That report, however, did not specify which joints were cracked, did not indicate if the evaluation was blinded, did not record the examiners level of experience, did not describe the methodology used to assess grip strength, and did not use any diagnostic imaging. Although we did not identify any deleterious clinical history or physical examination findings, occasional adverse sequelae of knuckle cracking have been reported by others [5, 15, 24]. In addition to acute MPJ damage attributable to vigorous knuckle cracking [5], chronic derangements have been reported with habitual knuckle cracking (eg, formation of knuckle pads [15], development of ligament ossification and calcification [24]).
We did find that active and passive ROM measurements increased after a distraction maneuver and resulted in an audible crack. The current study is the largest to show this association, and corroborates the findings of two other studies. In one study examining long finger MPJs, minimally increased ROM was found with passive flexion (62 MPJs; mean, 3°; SD, 6°) [13]. In another study of MPJs [19], there was reportedly a 5% to 10% gain in passive ROM, with a smaller increase in active ROM. While increases in ROM after joints crack is quite small, it is conceivable that even small increases in ROM may be associated with the sensation of “decreased tension” that habitual knuckle crackers often describe as a motivation for this voluntary activity.
Although the bubble formation mechanism is debated and bubble growth in vivo has not been studied extensively (in part owing to imaging difficulties) [14], the dynamic temporal changes and morphologic features of echogenic areas observed consistently in our study support the role of tribonucleation in the process of knuckle cracking. Tribonucleation is defined as the creation of small gas bubbles by the action of making and breaking contact between solid surfaces immersed in a liquid containing dissolved gas [8]. Tribonucleation causes bubble formation because large negative pressures are generated by viscous adhesion between two closely opposed joint surfaces separated by a thin film of viscous synovial fluid [2]. Bubble formation is found to be in proportion to the product of the viscosity of the fluid and to the velocity of the separation from the solid surfaces [8], although gentle contact of surfaces also can play a role [25]. One MRI study [10] evaluated a single individual (without information regarding clinical history or physical examination), and showed a transient bright signal in the joint space speculated to represent intraarticular gas. Kawchuk et al. [10] emphasized their belief that an audible crack results from the inception of a bubble in the MPJ, however, knuckle cracking always occurred faster than could be seen by a single-frame duration of 310 ms (3.2 frames per second), and no crack was audible during the MRI. In contrast to MRI, sonography allowed us to hear any audible crack during distraction and afforded a much faster temporal resolution (232 vs 3.2 frames per second) and superior spatial resolution (approximately 1.0 vs 0.1 mm).
Although there have been conflicting opinions and common concerns regarding the widespread habit of knuckle cracking, we found no detectable immediate adverse physical examination findings. While subjects with habitual knuckle cracking had no greater short-term impairment scores than subjects without knuckle cracking, future research should explore other related matters, such as other joints that crack, patients who are symptomatic, and long-term clinical outcomes. Our analysis shows that subjects with a history of habitual MPJ cracking are much more likely to crack other joints in their body. After a documented knuckle-cracking event, physical examination did show a small increased ROM, although the clinical relevance of this finding is uncertain. Finally, we observed that the dynamic sonographic findings of knuckle cracking are highly characteristic and visually impressive.
References
Abizanda P, Navarro JL, Garcia-Tomas MI, Lopez-Jimenez E, Martinez-Sanchez E, Paterna G. Validity and usefulness of hand-held dynamometry for measuring muscle strength in community-dwelling older persons. Arch Gerontol Geriatr. 2012;54:21–27.
Blatteau JE, Souraud JB, Gempp E, Boussuges A. Gas nuclei, their origin, and their role in bubble formation. Aviat Space Environ Med. 2006;77:1068–1076.
Brodeur R. The audible release associated with joint manipulation. J Manipulative Physiol Ther. 1994;18:155–164.
Castellanos J, Axelrod D. Effect of habitual knuckle cracking on hand function. Ann Rheum Dis. 1990;49:308–309.
Chan PS, Steinberg DR, Bozentka DJ. Consequences of knuckle cracking: a report of two acute injuries. Am J Orthop (Belle Mead, NJ). 1999;28:113–114.
Fryer GA, Mudge JM, McLaughlin PA. The effect of talocrural joint manipulation on range of motion at the ankle. J Manipulative Physiol Ther. 2002;25:384–390.
Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:44.
Ikels KG. Production of gas bubbles in fluids by tribonucleation. J Appl Physiol. 1970;28:524–527.
Jones AR, Yelverton CJ, Bester C. Ultrasound imaging of the trapeziometacarpal articular cavity to investigate the presence of intraarticular gas bubbles after chiropractic manipulation. J Manipulative Physiol Ther. 2014;37:476–484.
Kawchuk GN, Fryer J, Jaremko JL, Zeng H, Rowe L, Thompson R. Real-time visualization of joint cavitation. PLoS ONE. 2015;10:e0119470.
Malghem J, Omoumi P, Lecouvet FE, Vande Berg BC. Presumed intraarticular gas microbubbles resulting from a vacuum phenomenon: visualization with ultrasonography as hyperechoic microfoci. Skeletal Radiol. 2011;40:1287–1293.
Mennell J. The value of manipulation in the treatment of rheumatic diseases. Postgrad Med J. 1939;15:301–308.
Mierau D, Cassidy J, Bowen V, Dupuis P, Noftall F. Manipulation and mobilization of the third metacarpophalangeal joint: a quantitative radiographic and range of motion study. Man Med. 1988;3:135–140.
Papadopoulou V, Evgenidis S, Eckersley RJ, Mesimeris T, Balestra C, Kostoglou M, Tang MX, Karapantsios TD. Decompression induced bubble dynamics on ex vivo fat and muscle tissue surfaces with a new experimental set up. Colloids Surf B Biointerfaces. 2015;129:121–129.
Peterson CM, Barnes CJ, Davis LS. Knuckle pads: does knuckle cracking play an etiologic role? Pediatr Dermatol. 2000;17:450–452.
Protopapas M, Cymet TC. Joint cracking and popping: understanding noises that accompany articular release. J Am Osteopathic Assoc. 2002;102:283–287.
Remvig L, Jensen DV, Ward RC. Are diagnostic criteria for general joint hypermobility and benign joint hypermobility syndrome based on reproducible and valid tests? A review of the literature. J Rheumatol. 2007;34:798–803.
Roston JB, Haines RW. Cracking in the metacarpo-phalangeal joint. J Anat. 1947;81:165–173.
Sandoz R. The significance of the manipulative crack and of other articular noises. Ann Swiss Chiropr Assoc. 1969;4:47–68.
Simkin PA. Habitual knuckle cracking and hand function. Ann Rheum Dis. 1990;49:957.
Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3:472–479.
Swezey RL, Swezey SE. The consequences of habitual knuckle cracking. West J Med. 1975;122:377–379.
Unsworth A, Dowson D, Wright V. ‘Cracking joints’: a bioengineering study of cavitation in the metacarpophalangeal joint. Ann Rheum Dis. 1971;30:348–358.
Watson P, Hamilton A, Mollan R. Habitual joint cracking and radiological damage. BMJ. 1989;299:1566.
Wildeman S, Lhuissier H, Sun C, Lohse D, Prosperetti A. Tribonucleation of bubbles. Proc Natl Acad Sci U S A. 2014;111:10089–10094.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at University of California, Davis; Sacramento, CA, USA.
About this article
Cite this article
Boutin, R.D., Netto, A.P., Nakamura, D. et al. “Knuckle Cracking”: Can Blinded Observers Detect Changes with Physical Examination and Sonography?. Clin Orthop Relat Res 475, 1265–1271 (2017). https://doi.org/10.1007/s11999-016-5215-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-5215-3