Abstract
Background
Thrombin formation commences perioperatively in orthopaedic surgery and therefore some surgeons prefer preoperative initiation of pharmacologic thromboprophylaxis. However, because of the potential for increased surgical bleeding, the postoperative initiation of thromboprophylaxis has been advocated to reduce blood loss, need for transfusion, and bleeding complications. Trials on timing of thromboprophylaxis have been designed primarily to detect thrombotic events, and it has been difficult to interpret the magnitude of blood loss and bleeding events owing to lack of information for bleeding volume and underpowered bleeding end points.
Questions/purposes
We therefore asked whether there are differences in blood loss, transfusion requirements, and other postoperative clinical complications with preoperative versus postoperative start of thromboprophylaxis with dalteparin.
Methods
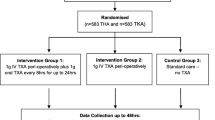
In a double-blind, randomized controlled trial, 80 patients undergoing primary cemented THA were allocated to dalteparin injections starting 12 hours before or 6 hours after surgery. Blood loss was measured by weighing sponges and drapes, volume in suction drains during surgery, and wound drains until removal 24 hours postoperatively. Hemoglobin and hematocrit were recorded at predefined times during and after surgery.
Results
We found no differences in blood loss (1081 mL ± 424 mL versus 1023 mL ± 238 mL), bleeding-related events (10% versus 17%), or number of patients who had transfusions (12 versus five) with preoperative and postoperative thromboprophylaxis, respectively. Other complications were few in both groups.
Conclusions
Our data suggest blood loss is similar with preoperative and postoperative initiation of dalteparin thromboprophylaxis, but indicate a trend toward fewer transfusion requirements which might favor postoperative start of thromboprophylaxis.
Level of Evidence
Level I, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
References
Barr PJ, Donnelly M, Cardwell C, Alam SS, Morris K, Parker M, Bailie KE. Drivers of transfusion decision making and quality of the evidence in orthopedic surgery: a systematic review of the literature. Transfus Med Rev. 2011;25:304–316.
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10.
Borgen PO, Dahl OE, Reikeras O. Preoperative versus postoperative initiation of dalteparin thromboprophylaxis in THA. Hip Int. 2010;20:301–307.
Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL. Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet. 1996;348:1055–1060.
Colwell CW Jr, Chelly JE, Murkin JM, Stevens D, O`Keefe TJ, Hall R, Parvizi J. Randomized study of aprotinin effect on transfusions and blood loss in primary THA. Clin Orthop Relat Res. 2007;465:189–195.
Dahl OE, Ogren M, Agnelli G, Eriksson BI, Cohen AT, Mouret P, Rosencher N, Bylock A, Panfilov S, Andersson M. Assessment of bleeding after concomitant administration of antiplatelet and anticoagulant agents in lower limb arthroplasty. Pathophysiol Haemost Thromb. 2006;35:428–434.
Dahl OE, Quinlan DJ, Bergqvist D, Eikelboom JW. A critical appraisal of bleeding events reported in venous thromboembolism prevention trials of patients undergoing hip and knee arthroplasty. J Thromb Haemost. 2010;8:1966–1975.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213.
Francis CW, Pellegrini VD Jr, Totterman S, Boyd AD Jr, Marder VJ, Liebert KM, Stulberg BN, Ayers DC, Rosenberg A, Kessler C, Johanson NA. Prevention of deep-vein thrombosis after total hip arthroplasty: comparison of warfarin and dalteparin. J Bone Joint Surg Am. 1997;79:1365–1372.
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW; American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th ed. Chest. 2008;133(6 suppl):381S–453S.
Graafsma YP, Prins MH, Lensing AW, de Haan RJ, Huisman MV, Buller HR. Bleeding classification in clinical trials: observer variability and clinical relevance. Thromb Haemost. 1997;78:1189–1192.
Hull RD, Liang J, Brant R. Pooled analysis of trials may, in the presence of heterogeneity inadvertently lead to fragile conclusions due to the importance of clinically relevant variables being either hidden or lost when the findings are pooled. Thromb Res. 2010;126:164–165.
Hull RD, Pineo GF, Francis C, Bergqvist D, Fellenius C, Soderberg K, Holmqvist A, Mant M, Dear R, Baylis B, Mah A, Brant R. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs warfarin in hip arthroplasty patients: a double-blind, randomized comparison. The North American Fragmin Trial Investigators. Arch Intern Med. 2000;160:2199–2207.
Hull RD, Yusen RD, Bergqvist D. State-of-the-art review: assessing the safety profiles of new anticoagulants for major orthopedic surgery thromboprophylaxis. Clin Appl Thromb Hemost. 2009;15:377–388.
Johansson T, Pettersson LG, Lisander B. Tranexamic acid in total hip arthroplasty saves blood and money: a randomized, double-blind study in 100 patients. Acta Orthop. 2005;76:314–319.
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, Soglian AG, Pap AF, Misselwitz F, Haas S; RECORD2 Investigators. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet. 2008;372:31–39.
Kakkar VV, Howe CT, Flanc C, Clarke MB. Natural history of postoperative deep-vein thrombosis. Lancet. 1969;2:230–232.
Lachiewicz PF. Comparison of ACCP and AAOS guidelines for VTE prophylaxis after total hip and total knee arthroplasty. Orthopedics. 2009;32(12 suppl):74–78.
Lemaire R. Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br. 2008;90:1128–1136.
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B. Hidden blood loss after total hip arthroplasty. J Arthroplasty. 2011;26:1100–1105.
Novicoff WM, Brown TE, Cui Q, Mihalko WM, Slone HS, Saleh KJ. Mandated venous thromboembolism prophylaxis: possible adverse outcomes. J Arthroplasty. 2008;23(6 suppl 1):15–19.
Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89:33–38.
Planes A, Vochelle N, Mazas F, Mansat C, Zucman J, Landais A, Pascariello JC, Weill D, Butel J. Prevention of postoperative venous thrombosis: a randomized trial comparing unfractionated heparin with low molecular weight heparin in patients undergoing total hip replacement. Thromb Haemost. 1988;60:407–410.
Raskob GE, Hirsh J. Controversies in timing of the first dose of anticoagulant prophylaxis against venous thromboembolism after major orthopedic surgery. Chest. 2003;124(6 suppl):379S–385S.
Salido JA, Marin LA, Gomez LA, Zorrilla P, Martinez C. Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery: analysis of predictive factors. J Bone Joint Surg Am. 2002;84:216–220.
Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty: correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86:561–565.
Sharrock NE, Go G, Harpel PC, Ranawat CS, Sculco TP, Salvati EA. The John Charnley Award: thrombogenesis during total hip arthroplasty. Clin Orthop Relat Res. 1995;319:16–27.
Strebel N, Prins M, Agnelli G, Buller HR. Preoperative or postoperative start of prophylaxis for venous thromboembolism with low-molecular-weight heparin in elective hip surgery? Arch Intern Med. 2002;162:1451–1456.
Walsh M, Preston C, Bong M, Patel V, Di Cesare PE. Relative risk factors for requirement of blood transfusion after total hip arthroplasty. J Arthroplasty. 2007;22:1162–1167.
Warwick D, Bannister GC, Glew D, Mitchelmore A, Thornton M, Peters TJ, Brookes S. Perioperative low-molecular-weight heparin: is it effective and safe. J Bone Joint Surg Br. 1995;77:715–719.
Acknowledgments
We thank Nina Bøhler, study nurse, for valuable help in preparing the injections and conducting the block randomization in this controlled study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he, or a member of his immediate family, has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in the connection with this submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at Martina Hansens Hospital, Baerum Postterminal, Norway.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Borgen, P.O., Dahl, O.E. & Reikerås, O. Blood Loss in Cemented THA is not Reduced with Postoperative Versus Preoperative Start of Thromboprophylaxis. Clin Orthop Relat Res 470, 2591–2598 (2012). https://doi.org/10.1007/s11999-012-2320-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2320-9