Abstract
Background
Roux-en-Y gastric bypass (RYGB) surgery can lead to long-term remission of type 2 diabetes mellitus, depending on changes in weight and circulating levels of gut hormones. The general objectives of this study were to evaluate changes in plasma levels of the ghrelin gene products following RYGB surgery and to determine the role of ghrelin in inhibiting apoptosis of INS-1 cells induced by hyperglycemia.
Methods
Sixteen obese Chinese patients with type 2 diabetes mellitus who underwent gastric bypass surgery were assessed in this investigation. Blood plasma levels of acylated ghrelin (AG), unacylated ghrelin (UAG), and obestatin (OB) were measured both before and 12 months after RYGB surgery. To determine the effect of ghrelin on inhibition of apoptosis, INS-1 cells were cultured in a high glucose concentration and treated with AG, UAG, or OB. Cell viability was assessed using the MTT assay, and apoptosis was evaluated by flow cytometry with Annexin-V FITC/PI double staining and transmission electron microscopy. Intracellular calcium trafficking was assessed using flow cytometry and confocal microscopy. All the data was processed using the SPSS statistical package and expressed as means ± SD, with p < 0.05 considered statistically significant.
Results
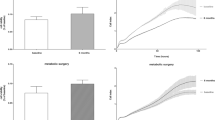
Fasting and postprandial plasma levels of AG, UAG, and OB were significantly elevated 1 year after RYGB surgery. Mean fasting plasma AG, UAG, and OB increased from preoperative levels of 37.0, 462, and 69.4 pg/mL, respectively, to 61.4, 804, and 112 pg/mL (with p < 0.05) 1 year after surgery. Mean 120-min postprandial plasma AG, UAG, and OB increased from preoperative levels of 23.8, 287, and 53.8 pg/mL, respectively, to 39.7, 516, and 69.0 pg/mL (with p < 0.05) postoperatively. After a 1-week culture of INS-1 beta cell in high glucose, peptide treatment showed increased cell survival by 69 % (AG), 60 % (UAG), and 73 % (OB) and decreased apoptosis by 49 % (AG), 37 % (UAG), and 38 % (OB) compared to cells cultured in high glucose without peptides, respectively (with p < 0.05). Treatment with AG, UAG, and OB inhibited intracellular calcium mobilization and intramitochondrial calcium accumulation in INS-1 cells to protect the cells from hyperglycemia-induced apoptosis.
Conclusions
The remission of diabetes following RYGB surgery seems to be associated with increased plasma levels of AG, UAG, and OB. Moreover, the ghrelin gene products probably protect β cells by maintaining calcium homeostasis. Additional mechanisms, currently unclear, are likely to be involved as well.






Similar content being viewed by others
References
IDF diabetes atlas. 5th ed. Brussels: International Diabetes Federation, 2011 (http://www.idf.org/diabetesatlas).
Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248.e5–56.e5.
Buchwald H, Avidor Y, Braunwald E, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Rubino F. Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. J Diabetes Care. 2008;31(2):$290–96.
Yu H, Zheng X, Zhang Z. Mechanism of Roux-en-Y gastric bypass treatment for type 2 diabetes in rats. J Gastrointest Surg. 2013;17(6):1073–83.
Shak JR, Roper J, Perez-Perez GI, et al. The effect of laparoscopic gastric banding surgery on plasma levels of appetite-control, insulinotropic, and digestive hormones. Obes Surg. 2008;18:1089–96.
Martins C, Kjelstrup L, Ingrid L, et al. Impact of sustained weight loss achieved through Roux-en-Y gastric bypass or a lifestyle intervention on ghrelin, obestatin, and ghrelin/obestatin ratio in morbidly obese patients. Obes Surg. 2011;21(6):751–8.
Holdstock C, Engstrӧm BE, Ohrvall M, et al. Ghrelin and adipose tissue regulatory peptides: effect of gastric bypass surgery in obese humans. J Clin Endocrinol Metab. 2003;88:3177–83.
Faraj M, Havel PJ, Phélis S, et al. Plasma acylation-stimulating protein, adiponectin, leptin, and ghrelin before and after weight loss induced by gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2003;88:1594–602.
Fruhbeck G, Rotellar F, Hernández-Lizoain JL, et al. Fasting plasma ghrelin concentrations 6 months after gastric bypass are not determined by weight loss or changes in insulinemia. Obes Surg. 2004;14:1208–15.
Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346(21):1623–30.
Morinigo R, Casamitjana R, Moize V, et al. Short-term effects of gastric bypass surgery on circulating ghrelin levels. Obes Res. 2004;12:1108–16.
Kojima M, Hosoda H, Date Y, et al. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–60.
Abizaid A, Horvath TL. Ghrelin and the central regulation of feeding and energy balance. Indian J Endocrinol Metab. 2012;16 Suppl 3:S617–26.
González-Jiménez E, Schmidt Río-Valle J. Regulation of dietary intake and energy balance: factors and mechanisms involved. Nutr Hosp. 2012;27(6):1850–9.
Damjanovic SS, Lalic NM, Pesko PM, et al. Acute effects of ghrelin on insulin secretion and glucose disposal rate in gastrectomized patients. J Clin Endocrinol Metab. 2006;91(7):2574–81.
Kim SW, Kim KW, Shin CS, et al. Acylated ghrelin secretion is acutely suppressed by oral glucose load or insulin-induced hypoglycemia independently of basal growth hormone secretion in humans. Horm Res. 2007;67(5):211–9.
Kishimoto I, Tokudome T, Hosoda H, et al. Ghrelin and cardiovascular diseases. J Cardiol. 2012;59(1):8–13.
Korbonits M, Goldstone AP, Gueorguiev M, et al. Ghrelin—a hormone with multiple functions. Front Neuroendocrinol. 2004;25(1):27–68.
Soares JB, Leite-Moreira AF. Ghrelin, des-acyl ghrelin and obestatin: three pieces of the same puzzle. Peptides. 2008;29(7):1255–70.
Granata R, Baragli A, Settanni F, et al. Unraveling the role of the ghrelin gene peptides in the endocrine pancreas. J Mol Endocrinol. 2010;45(3):107–18.
Granata R, Isgaard J, Alloatti G, et al. Cardiovascular actions of the ghrelin gene-derived peptides and growth hormone-releasing hormone. Exp Biol Med (Maywood). 2011;236(5):505–14.
Holst B, Egerod KJ, et al. G protein-coupled receptor 39 deficiency is associated with pancreatic islet dysfunction. Endocrinology. 2009;150(6):2577–85.
Fujimiya M, Asakawa A, Ataka K, et al. Ghrelin, des-acyl ghrelin, and obestatin: regulatory roles on the gastrointestinal motility. Int J Pept. 2010;2010:305192.
Chanclón B, Luque RM, Córdoba-Chacón J, et al. Role of endogenous cortistatin in the regulation of ghrelin system expression at pancreatic level under normal and obese conditions. PLoS One. 2013;8(2):e57834.
Salehi A, Dornonville de la Cour C, Håkanson R, et al. Effects of ghrelin on insulin and glucagon secretion: a study of isolated pancreatic islets and intact mice. Regul Pept. 2004;118(3):143–50.
Peng Z, Xiaolei Z, Al-Sanaban H, et al. Ghrelin inhibits insulin release by regulating the expression of inwardly rectifying potassium channel 6.2 in islets. Am J Med Sci. 2012;343(3):215–9.
Cummings DE. Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes (Lond). 2009;33 Suppl 1:S33–40.
Merglen A, Theander S, Rubi B, et al. Glucose sensitivity and metabolism-secretion coupling studied during two-year continuous culture in INS-1E insulinoma cells. Endocrinology. 2004;145:667–78.
Asfari M, Janjic D, Meda P, et al. Establishment of 2-mercaptoethanol dependent differentiated insulin-secreting cell lines. Endocrinology. 1992;130:167–78.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32:2133–5.
Pournaras DJ, Glicksman C, Vincent RP, et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology. 2012;153(8):3613–9.
Hideharu S, Poochong T, Schauer PR, et al. Review of metabolic surgery for type 2 diabetes in patients with a BMI < 35 kg/m2. J Obes. 2012;2012:147256.
Schernthaner G, Brix JM, Kopp HP, et al. Cure of type 2 diabetes by metabolic surgery? A critical analysis of the evidence in 2010. Diabetes Care. 2011;34 Suppl 2:S355–60.
Oliván B, Teixeira J, Bose M, et al. Effect of weight loss by diet or gastric bypass surgery on peptide YY3-36 levels. Ann Surg. 2009;249(6):948–53.
Kelishadi R, Hashemipour M, Mohammadifard N, et al. Short- and long-term relationships of serum ghrelin with changes in body composition and the metabolic syndrome in prepubescent obese children following two different weight loss programmes. Clin Endocrinol. 2008;69(5):721–9.
Fruhbeck G, Diez-Caballero A, Gil M, et al. The decrease in plasma ghrelin concentrations following bariatric surgery depends on the functional integrity of the fundus. Obes Surg. 2004;14:606–12.
Ariyasu H, Takaya K, Tagami T, et al. Stomach is a major source of circulating ghrelin, and feeding determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001;86:4753–8.
Pournaras DJ, Carel W. Ghrelin and metabolic surgery. Int J Pept. 2010;2010:217267.
Akamizu T, Kangawa K. The physiological significance and potential clinical applications of ghrelin. Eur J Intern Med. 2012;23:197–202.
Moran TH, Dailey MJ. Intestinal feedback signaling and satiety. Physiol Behav. 2011;105(1):77–81.
Patriti A, Facchiano E, Gullà N, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2007;245(1):157–8.
Borg CM, le Roux CW, Ghatei MA, et al. Progressive rise in gut hormone levels after Roux-en-Y gastric bypass suggests gut adaptation and explains altered satiety. Br J Surg. 2006;93(2):210–5.
Zorrilla EP, Iwasaki S, Moss JA, et al. Vaccination against weight gain. Proc Natl Acad Sci U S A. 2006;103(35):13226–31.
Wiedmer P, Nogueiras R, Broglio F, et al. Ghrelin, obesity and diabetes. Nat Clin Pract Endocrinol Metab. 2007;3(10):705–12. Review.
Favaro E, Granata R, Miceli I, et al. The ghrelin gene products and exendin-4 promote survival of human pancreatic islet endothelial cells in hyperglycaemic conditions, through phosphoinositide 3-kinase/Akt, extracellular signal-related kinase (ERK)1/2 and cAMP/protein kinase A (PKA) signalling pathways. Diabetologia. 2012;55(4):1058–70.
Wang W, Zhang D, Zhao H, et al. Ghrelin inhibits cell apoptosis induced by lipotoxicity in pancreatic beta-cell line. Regul Pept. 2010;161(1–3):43–50.
Cai L, Li W, Wang G, et al. Hyperglycemia-induced apoptosis in mouse myocardium: mitochondrial cytochrome c-mediated caspase-3 activation pathway. Diabetes. 2002;51:1938–48.
Wold LE, Ceylan-Isik AF, Fang CX, et al. Metallothionein alleviates cardiac dysfunction in streptozotocin-induced diabetes: role of Ca2+ cycling proteins, NADPH oxidase, poly(ADP-Ribose) polymerase and myosin heavy chain isozyme. Free Radic Biol Med. 2006;40:1419–29.
Li J, Wang P, Yu S, et al. Calcium entry mediates hyperglycemia-induced apoptosis through Ca2+/calmodulin-dependent kinase II in retinal capillary endothelial cells. Mol Vis. 2012;18:2371–9.
Müller I, Lipp P, Thiel G. Ca2+ signaling and gene transcription in glucose-stimulated insulinoma cells. Cell Calcium. 2012;52(2):137–51.
Younce CW, Burmeister MA, Ayala JE. Exendin-4 attenuates high glucose-induced cardiomyocyte apoptosis via inhibition of endoplasmic reticulum stress and activation of SERCA2a. Am J Physiol Cell Physiol. 2013;304(6):C508–18.
Herchuelz A, Nguidjoe E, Jiang L, et al. β-Cell preservation and regeneration in diabetes by modulation of β-cell Ca2+ homeostasis. Diabetes Obes Metab. 2012;14(3):136–42.
Giorgi G, Baldassari F, Bononi A, et al. Mitochondrial Ca2+ and apoptosis. Cell Calcium. 2012;52(1):36–43.
Xu G, Chen J, Jing G, Shalev A. Preventing β-cell loss and diabetes with calcium channel blockers. Diabetes. 2012;61(4):848–56.
Rudijanto A. Calcium channel blocker (diltiazem) inhibits apoptosis of vascular smooth muscle cell exposed to high glucose concentration through lectin-like oxidized low density lipoprotein receptor-1 (LOX-1) pathway. Acta Med Indones. 2010;42(2):59–65.
Wang Y, Gao L, Li Y, Sun Z, et al. Nifedipine protects INS-1 β-cell from high glucose-induced ER stress and apoptosis. Int J Mol Sci. 2011;12(11):7569–80.
Giorgi C, Baldassari F, Bononi A. Mitochondrial Ca(2+) and apoptosis. Cell Calcium. 2012;52(1):36–43.
Giorgi C, Agnoletto C, Bononi A, et al. Mitochondrial calcium homeostasis as potential target for mitochondrial medicine. Mitochondrion. 2012;12(1):77–85.
Wang Y, Nishi M, Doi A, et al. Ghrelin inhibits insulin secretion through the AMPK–UCP2 pathway in beta cells. FEBS Lett. 2010;584(8):1503–8.
Buschard K, Hy M, Bokvist K, et al. Sulfatide controls insulin secretion by modulation of ATP-sensitive K(+)-channel activity and Ca(2+)-dependent exocytosis in rat pancreatic beta-cells. Diabetes. 2002;51:2514–21.
Zhang CY, Baffy G, Perret P, et al. Uncoupling protein-2 negatively regulates insulin secretion and is a major link between obesity, beta cell dysfunction, and type 2 diabetes. Cell. 2001;105:745–55.
Lee SH, Lee HY, Kim SY, et al. Enhancing effect of taurine on glucose response in UCP2-overexpressing beta cells. Diabetes Res Clin Pract. 2004;66 Suppl 1:S69–74.
Ma X, Lin Y, Lin L, et al. Ablation of ghrelin receptor in leptin-deficient ob/ob mice has paradoxical effects on glucose homeostasis when compared with ablation of ghrelin in ob/ob mice. Am J Physiol Endocrinol Metab. 2012;303(3):E422–31.
Acknowledgments
This study was supported by funding from the National Natural Science Foundation of China (No. 81000158) and the Outstanding Scientific Fund of ShengJing Hospital. The paper has been revised by Mark Sewe from China Medical University and all authors showed respect for his kindly help.
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, J., Feng, X., Zhong, S. et al. Gastric Bypass Surgery May Improve Beta Cell Apoptosis with Ghrelin Overexpression in Patients with BMI ≥ 32.5 kg/m2 . OBES SURG 24, 561–571 (2014). https://doi.org/10.1007/s11695-013-1135-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-1135-4