Abstract
Summary
We estimated the number of hip fracture patients in 2007 in Japan and investigated the trends in incidence during a 20-year period from 1987 to 2007. Despite the increasing number of new patients, the incidence of hip fracture in some age groups showed the possibility of decline.
Purpose
The aims of this study were to estimate the number of hip fracture patients in 2007, to investigate the trends in incidence during a 20-year period from 1987 to 2007, and to show the regional differences in Japan.
Methods
Data were collected through a nationwide survey based on hospitals by the mailing method. Hip fracture incidences by sex and age and standardized incidence ratios by region were calculated.
Results
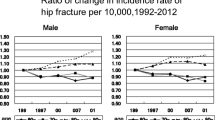
The estimated numbers of new hip fracture patients in 2007 were 148,100 in total (95% CI, 144,000–152,200), 31,300 (30,500–32,100) for men, and 116,800 (113,900–119,700) for women. The incidence rate in men aged 60–69 years and that in women aged 60–79 years were the lowest in the 15-year period from 1992 to 2007. The incidence was higher in western areas of Japan than in eastern areas in both men and women.
Conclusions
Despite the increasing number of new patients, the incidence of hip fracture in some age groups for both men and women showed the possibility of decline. The exact reasons for this are unknown, but drug therapy for osteoporosis and fall prevention programs might have influenced the results. Some nutrient intakes might explain the regional differences not only in Japan but also in some other countries.
Similar content being viewed by others
Introduction
Hip fracture is the most serious outcome of osteoporosis and is becoming more frequent as the age of the world’s population increases [1]. It is estimated that the number of hip fractures worldwide, which was about 1.7 million in 1990, will increase to 6.3 million in 2050 even if age-adjusted incidence rates for hip fracture remain stable [2].
From a different perspective, osteoporotic fractures worldwide accounted for 0.83% of the global burden of non-communicable diseases. In Europe, osteoporotic fractures accounted more for the Disability Adjusted Life Years lost than did common cancers with the exception of lung cancer [3].
In Japan, hip fracture, along with cerebrovascular disease, is a major cause of becoming bedridden, markedly decreasing quality of life in the elderly [4]. Hence, countermeasures against hip fracture are urgent medical and social issues in the rapidly aging Japanese population.
A nationwide survey in Japan has been implemented every 5 years since 1987, and the trend in hip fracture incidence has been reported. The first nationwide survey was carried out in 1987 to clarify the sex-specific and age-specific incidences of hip fractures, and the estimated number of new patients in 1987 was about 53,200 [5]. The second nationwide survey, using a different method to improve accuracy, was performed in 1992, and the number of new patients was estimated to be 76, 600 [6]. In the third nationwide survey, carried out in 1997, the estimated number of new patients was 92,400 [7]. In the fourth survey, in 2002, the estimated number was 117,900 [8]. The number of new patients with hip fracture increased 2.2-fold in the 15-period from 1987 to 2002.
The aims of this study were to estimate the number of hip fracture patients in 2007, to investigate the trends in incidence during the 20-year period from 1987 to 2007, and to show the regional distribution of hip fracture incidence in Japan.
Subjects and methods
Sampling method
For a nationwide estimate
To estimate the number of new hip fracture patients nationwide, in the fifth survey in 2007, hospitals and clinics including or specializing in orthopedics throughout Japan were divided into 13 strata according to the number of beds, maintaining comparability with previous surveys. In Japan, small hospitals with 19 or fewer beds are defined as clinics. All hospitals with 200 beds or more were included, and hospitals with 199 or fewer beds were randomly selected by Neyman’s allocation method [9] to minimize standard error. In this survey, among 8,234 orthopedic institutions in Japan, 4,500 institutions were selected as sites to investigate a nationwide estimate, using the same sample size as the previous surveys (Table 1). The number of new patients with hip fracture was estimated by the following formula:
where N i is the number of surveyed institutions in each stratum, n i is the number of responding institutions in each stratum, and P i is the summation of the number of new patients in each stratum [7].
For regional estimates
Data from 5,613 institutions, all hospitals with 20 beds or more and 479 clinics, were used for regional estimates to improve estimation accuracy. Data from clinics that had been randomly selected for the nationwide estimate were used (Table 1).
To evaluate the regional differences in incidence of hip fracture, Japan was divided into 12 regions based on the National Health and Nutrition Survey in Japan.
The standardized incidence ratio was calculated as follows:
where B is the estimated number of patients in each region, I is the nationwide incidence of hip fracture by sex and age groups, and P is the regional population by sex and age groups.
Incidences by sex and age groups were calculated on the basis of the estimated number of new patients. This incidence was multiplied by the population by the sex and age groups in each region to obtain the expected number of patients. The ratio of estimated number of patients to expected number was calculated as the standardized incidence ratio.
Population figures from the 2005 national census were used to calculate the incidence of hip fracture and the standardized incidence ratio by region.
Questionnaire
A questionnaire was sent by mail to all participating or selected hospitals and clinics based on administrative hospital data from the Ministry of Health, Labour, and Welfare. We asked for information on the number of new patients with hip fracture between January 1 and December 31 in 2007 and information on each patient’s sex and age. Patients that underwent surgery for hip fracture at other institutions or patients for rehabilitation were excluded to avoid double counting of new hip fracture patients.
Results
Response rates
For a nationwide estimate, replies were obtained from 2,997 institutions, a response rate of 66.6%. The response rate was highest (76.2%) in hospitals with 900 beds and more and was lowest (58.7%) in hospitals with 500–599 beds. For regional estimates, replies were obtained from 3,778 institutions, a response rate of 67.3% (Table 2). The response rates by region were 78.4% in Hokuriku, 74.9% in Tohoku, 73.1% in Minamikyushu, 72.6% in Chugoku, 72.6% in Kitakyushu, 70.7% in Hokkaido, 67.0% in Kinki II, 66.1% in Shikoku, 65.4% in Kanto II, 65.3% in Tokai, 63.2% in Kinki I, and 59.4% in Kanto I.
Nationwide estimate
The estimated numbers of new hip fracture patients in 2007 were 148,100 in total (95% CI, 144,000–152,200), 31,300 (30,500–32,100) for men, and 116,800 (113,900–119,700) for women. As shown in Table 3, the number of new patients in the 2007 survey was 1.26 times higher than that in the 2002 survey [8, 10], and the number of new patients in the 2007 survey was 2.78 times higher than that in the 1987 survey [5]. The number of new female patients increased from 39,700 in 1987 to 116,800 in 2007.
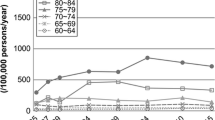
The crude annual incidence rate (per 10,000) of hip fracture in 2007 was calculated by sex and age (Table 4). The incidence rates of hip fracture in men and women by age were 0.32 and 0.15 under 40 years, 0.92 and 0.70 in 40s, 2.03 and 2.95 in 50s, 4.81 and 8.11 in 60s, 18.12 and 39.71 in 70s, 61.03 and 157.14 in 80s, and 146.62 and 313.58 over 90 years, respectively. The incidence rates of hip fracture were lowest for men aged 60–69 years and for women aged 60–79 years in the 15-year period from 1992 to 2007. As for the incidence of hip fracture overall, it kept increasing in each 5-year period in both men and women. The overall incidences in the 1992 survey were 3.08 in men and 9.20 in women, and those in 2007 were 5.11 in men and 18.14 in women. The overall incidences in the 2007 survey were 1.66 times higher in men and 1.97-times higher in women than those in 1992.
Regional estimates
Crude incidences of hip fracture per 10,000 by region were high in men in the western areas of Japan (Shikoku, 7.46 per 10,000; Minamikyushu, 7.28 per 10,000; and Chugoku, 7.03 per 10,000) compared with those in the eastern areas (Kanto I, 3.77 per 10,000; Tohoku, 4.28 per 10,000; and Tokai, 4.97 per 10,000). The pattern in women was similar, with the highest rates in the western areas of Minamikyushu (27.37 per 10,000), Chugoku (24.98 per 10,000), and Shikoku (24.64 per 10,000) and lower rates in the eastern areas of Kanto I (13.59 per 10,000), Tohoku (13.66 per 10,000), and Kanto II (17.1 per 10,000).
Figure 1 shows the east–west regional differences expressed by standardized incidence ratios. Similarity in the patterns for both men and women is noteworthy.
Discussion
The results of our study showed the incidence of hip fracture in 2007 and the trend in hip fracture over a 20-year period. According to data obtained every 5 years, the number of new hip fracture patients has continued to increase. The total number of hip fracture patients was 53,200 in 1987, and the number increased markedly to 148,100 in 2007. The number of female hip fracture patients was about 3.7 times larger than the number of male hip fracture patients in 2007, indicating a disparity in sex. It is clear that the number of new patients increases yearly because of changes in the national demographic structure. Between 1985 and 2005, the proportion of people 65 years of age or over in Japan increased from 10.3% (12.5 million) to 20.1% (25.7 million; 8.6% to 17.4% in men and 12.0% to 22.6% in women). The numbers of men and women 60 years of age or over in 2000 were 13 million and 16.8 million, respectively, and those in 2005 were 15 million and 19.2 million, respectively. Increases in number of people 60 years of age or over in 2005 were approximately two million (rate of increase of 15.9%) for men and 2.4 million (rate of increase of 14.4%) for women compared to the numbers in the year 2000. Japan is now facing an unprecedented situation, an aging society.
The aging population has become a major issue not only in Japan but also in many other countries. The World Population Prospects based on the 2006 Revision Population Database show the proportions of people aged 60 years of age or over in each country. The most remarkable difference among countries is the speed of population aging [11].
A study in Korea, based on data from the Health Insurance Review Agency, showed that the incidence rate of hip fractures in women, but not that in men, increased from 2001 to 2004 in Korea [12]. The reasons for the increase were suggested to be due to an increase in the number of frail elderly women and a substantial increase in chronic disease related to frailty. The proportions of people aged 60 years of age or over in Korea were 11.4% in 2000 and 13.7% in 2005. A study in Taiwan, based on an inpatient database of the National Health Insurance Program, showed a modest increase in hip fracture incidence and a steady increase in the actual number of hip fractures for both men and women from 1996 to 2000 in Taiwan [13]. The reasons for this trend were suggested to be inadequate nutrition for the elderly in Taiwan in past decades, high probability of falls, and insufficient geriatric care. Another study in Taiwan, a nationwide 7-year trend of hip fractures in the elderly population aged 65 years or over, showed that overall incidence increased by 30% from 1996 to 2002 and that there were dramatic increases in incidences for people aged older than 85 years in both males and females [14]. Although the percentage of people aged 60 years or over in both of these Asian countries was not so high during the study period, the percentage is predicted to be much higher in the near future.
According to a study on trend of hip fracture in Germany during the period from 1995 to 2004, using data obtained from the national discharge register, age and sex-adjusted annual incidence ratios increased statistically significantly, but only slightly [15]. The proportions of people aged 60 years or over in Germany were 20.9% in 1995 and 25.1% in 2005 [16]. These percentages are similar in those in Japan. However, the prospect of the speed of population aging after 2005 is quite different. In Germany, it is estimated that a further increase will not greatly exceed that expected from the demographic aging of the population. A study in southeastern Norway during the period from 1998 to 2003 showed a high incidence of hip fracture, but did not indicate any increase [17]. The proportions of people aged 60 years or over in Norway were 20.5% in 1995 and 19.6% in 2005 [16].
While some studies have shown an increase in the incidence of hip fractures, one nationwide study in Finland suggested a declining trend in fracture rates. That study showed that the crude incidence of hip fracture decreased between 1997 and 2004, following a constant rise between 1970 and 1997 [18]. Although the reasons for the secular change in risk of hip fracture incidence were unknown, the authors provided possible explanations, such as a cohort effect toward healthier elderly populations, increase in average body weight and body mass index, specific actions to prevent and treat osteoporosis, and effects of programs and interventions to prevent falling by strength and balance training.
In addition to the nationwide study in Finland, two recent small studies in Canada and Denmark have also suggested the decline in the incidence of hip fracture. The study in Ontario, Canada, showed the possibility of decline in hip fracture rate because of increased patterns of diagnosis through the bone mineral density testing and treatment for osteoporosis, introduction of the bisphosphonate family [19]. According to the study conducted in Funen, Denmark, between 1996 and 2003, the incidence rate of first hip fracture decreased in both men and women. In most age groups, the actual number of fractures also decreased. A multitude of interventions for the elderly such as preventive home visits, fall prevention programs, optimized nutrition, and medication were suggested as possible reasons for the decrease [20]. Considering the percentages of people aged 60 years or over in these three countries, the changes during the study periods were not so great: 19.0% in 1995 and 21.4% in 2005 in Finland, 16.1% in 1995 and 16.7% in 2000 in Canada, and 19.8% in 1995 and 21.2% in 2005 in Denmark [16].
In the present study, hip fracture rates were very high in the older age groups. These results were in accordance with results for hip fracture incidence from 2004 to 2006 in Tottori, which is located in mid-western Japan [21]. However, we found that the incidences of hip fracture in 2007 were lowest in men aged 60–69 years and in women aged 60–79 years in the 15-year period from 1992 to 2007. As to the reason for that, we consider that persons 60–70 years old with osteoporosis might have come to medical attention and have been treated aggressively. In persons in their 80s and 90s and over, medical treatment for serious diseases such as stroke might be given priority over treatment of osteoporosis, resulting in hip fracture.
Focusing on the current situation of osteoporosis in Japan, it is difficult to obtain the incidence of osteoporosis nationwide at present. However, according to a cohort study based on the general population, Research on Osteoarthritis/Osteoporosis Against Disability by Yoshimura et al., the number of osteoporosis patients aged 40 years or over is estimated to be 6.4 million diagnosed by the lumbar spine or 10.7 million diagnosed by the femoral neck [22].
According to a questionnaire survey of diagnosis and treatment of osteoporosis for doctors specializing in orthopedics, internal medicine, and obstetrics and gynecology, 73% of the doctors in total and more than 95% of orthopedists diagnosed osteoporosis. The recognition rates of diagnostic criteria for osteoporosis in Japan were 61% in total and more than 90% by orthopedists [23].
Regarding first-line treatment for osteoporosis, for patients aged 65 years or over without existing fractures, 43% of doctors chose bisphosphonates and the next was activated vitamin D3 (29%). For patients aged 65 years or over with existing fractures, 55% of doctors chose bisphosphonates and the next was activated vitamin D (22%). It has been recognized among doctors that the ultimate goal of drug therapy for osteoporosis is to prevent fractures. Drug therapy might influence the incidence of hip fracture in the near future.
There has been a change in people’s perspective on falling, from fear of fractures to fall prevention. Experiencing falling may lead to fear of falling and thus a decline in quality of life for elderly people. Since falling is the primary risk factor for hip fractures, lessons for fall prevention started in 1997. Educational campaigns for fall prevention have been carried out in many parts of Japan since then [24]. Programs for fall prevention have been created for elderly persons with various risk levels and in different settings. Iwamoto et al. reported the beneficial effect of an exercise program aimed at improving flexibility, body balance, muscle power, and walking ability in preventing falls in the elderly [25]. A community exercise program for frail elderly people and an exercise intervention for community-dwelling elderly Japanese women showed that the combination of exercise classes and home-based exercise improved physical function and decreased the incidence of falls [26, 27]. Moreover, randomized controlled trials in the USA and Australia have shown the positive effects of Tai Chi programs, such as a decrease in the number of falls and the risk for falling and an improvement in functional balance [28, 29]. As a part of a health care project in a town, an exercise based on Tai Chi has been developed and practiced in Japan [30].
The results of the present study showed that the incidence of hip fracture was higher in the western areas than in the eastern areas of Japan for both men and women. This trend has not changed since 1987, when the first nationwide survey was carried out. According to a study on associations between hip fracture incidence and intake of four nutrients, calcium, magnesium, vitamin D, and vitamin K, intake of vitamin K showed a possibility of contributing to the regional differences more than did intake of calcium or vitamin D; high intake of vitamin K was associated with lower incidence of hip fracture, and vice versa [31]. Kaneki et al. found a large geographic difference in serum vitamin K2 levels in postmenopausal women and showed the relation between regional difference in intake of fermented soybeans, which contain a large amount of MK-7, and hip fracture incidence [32].
Although each country has unique factors that might influence the incidence of hip fracture besides the common factors related to hip fractures, there is a possibility that intakes of nutrients, especially intake of vitamin K, might explain the regional differences in some countries.
In countries that will face rapid aging of the population in the near future, such as Korea and China, the number of hip fracture patients will continue to increase. However, appropriate diagnosis of osteoporosis, widespread use of antiresorptive agents and the development of new medication, thorough countermeasures for fall prevention, and proper nutrient intake might contribute to the decline of hip fracture incidence in the coming years.
Our study has several limitations. First, we used the mailing method because we do not have a nationwide computer-based register system of hip fractures. At present, this is the best way to obtain information on hip fractures as a nationwide survey. In order to receive as many responses as possible, we asked for it four times. Moreover, we dealt with any questions from institutions on the phone. Second, although we asked institutions not to include patients that underwent surgery for hip fracture at other institutions or patients for rehabilitation, it was not possible to check them. Third, since we collected data for all hip fracture patients together, it was not possible to distinguish between fractures caused by primary osteoporosis and secondary osteoporosis. It was also impossible to analyze data by types of hip fractures.
In conclusion, despite the increasing number of new patients, the incidence of hip fracture in some age groups for both men and women showed the possibility of decline. The exact reasons for this are unknown, but drug therapy for osteoporosis and fall prevention programs might have contributed to the results. Moreover, some nutrient intakes might explain the regional differences not only in Japan but also in some countries. Additional studies are necessary to identify factors that contribute to regional differences throughout the world.
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018
Johnell O, Kanis J (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Ministry of Health, Labour and Welfare, Japan (2006) Comprehensive survey of living conditions of the people on health and welfare (in Japanese). Health and Welfare Statistics Association, Tokyo
Orimo H, Hosoda Y, Fujiwara S et al (1991) Hip fracture incidence in Japan. J Bone Miner Metab 9:89–93
Orimo H, Hashimoto T, Yoshimura N et al (1997) Nationwide incidence survey of femoral neck fracture in Japan, 1992. J Bone Miner Metab 15:89–93
Orimo H, Hashimoto T, Sakata K, Yoshimura N, Suzuki T, Hosoi T (2000) Trends in the incidence of hip fracture in Japan, 1987–1997: the third nationwide survey. J Bone Miner Metab 18:126–131
Orimo H, Sakata K (2004) Hip fracture incidence in Japan in 2002: report of the 4th Nationwide Survey for Hip Fracture. Jpn Med J 4180:25–30 (in Japanese)
Groves R, Fowler F, Couper M et al (2009) Survey methodology, 2nd edn. Wiley, New Jersey
Yoshimura N, Suzuki T, Hosoi T, Orimo H (2005) Epidemiology of hip fracture in Japan: incidence and risk factors. J Bone Miner Metab 23(Suppl):78–80
Lutz W, Sanderson W, Scherbov S (2008) The coming acceleration of global population ageing. Nature 451:716–719
Lim S, Koo B, Lee E et al (2008) Incidence of hip fractures in Korea. J Bone Miner Metab 26:400–405
Chie W, Yang R, Liu J, Tsai K (2004) High incidence rate of hip fracture in Taiwan: estimated from a nationwide health insurance database. Osteoporos Int 15:998–1002
Shao C, Hsieh Y, Tsai C, Lai K (2009) A nationwide seven-year trend of hip fractures in the elderly population of Taiwan. Bone 44:125–129
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2007) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int. doi:10.1007/s0019800705346
World Population Prospects, Department of Economics and Social Affairs homepage. Website: http://un.org/esa/population/unpop/htm
Bjørgul K, Reikerås O (2007) Incidence of hip fracture in southeastern Norway A study of 1,730 cervical and trochanteric fractures. Int Orthop 31:665–669
Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Jarvinen M (2006) Nationwide decline in incidence of hip fracture. J Bone Miner Res 21(12):1836–1838
Jaglal S, Weller I, Mamdani M, Hawker G, Kreder H, Jaakkimainen L, Adachi J (2005) Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res 20:898–905
Nymark T, Lauritsen J, Ovesen O, Rock N, Jeune B (2006) Decreasing incidence of hip fracture in the Funen County, Denmark. Acta Orthop 77:109–113
Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K, Teshima R (2008) Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int. doi:10.1007/s0019800806850
Yoshimura N, Muraki S, Oka H et al (2009) Prevalence of knee osteoarthritis, lumber spondylosis in Japanese men and women: the Research on Osteoarthritis/osteoporosis Against Disability (ROAD). J Bone Miner Metab 27(5):620–628
Orimo H (2007) Osteoporosis in the elderly. Nippon Ronen Igakkai Zasshi 44:579–581 (in Japanese)
Mutoh Y (2008) Medical encyclopedia for fall prevention. 1st edn. 178–188. J Med J Tokyo (in Japanese)
Iwamoto J, Suzuki H, Tanaka K et al (2008) Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporos Int. doi:10.1007/s0019800807949
Suzuki T, Kim H, Yoshida H, Ishizaki T (2004) Randomized controlled trial of exercise intervention for the prevention of falls in community-dwelling elderly Japanese women. J Bone Miner Metab 22:602–611
Inokuchi S, Matsusaka N, Hayashi T, Shindo H (2007) Feasibility and effectiveness of a nurse-led community programme for prevention of falls among frail elderly people: a multi-centre controlled trial. J Rehabil Med 39:479–485
Li F, Harmer P, Fisher K, McAuley E et al (2005) Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci 60:187–194
Voukelatos A, Cumming R, Lord S, Rissel C (2007) A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi Trial. J Am Geriatr Soc 55:1185–1191
Yasumura S, Matsuzaki Y (2009) Special Report ‘Prevention of nursing care in Kitakata city through Tai Chi program’. Public Health 4:260–265 (in Japanese)
Yaegashi Y, Onoda T, Tanno K, Kuribayashi T, Sakata K, Orimo H (2008) Association of hip fracture incidence and intake of calcium, magnesium, vitamin D, and vitamin K. Eur J Epidemiol 23:219–225
Kaneki M, Hedges S, Hosoi T et al (2001) Japanese fermented soybean food as the major determinant levels of vitamin K2: possible implications for hip-fracture risk. Nutrition 17:315–321
Acknowledgements
This study was supported by a Grant-in-Aid for Comprehensive Research on Aging and Health from the Ministry of Health Labour and Welfare of Japan.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Orimo, H., Yaegashi, Y., Onoda, T. et al. Hip fracture incidence in Japan: estimates of new patients in 2007 and 20-year trends. Arch Osteoporos 4, 71–77 (2009). https://doi.org/10.1007/s11657-009-0031-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11657-009-0031-y