Abstract
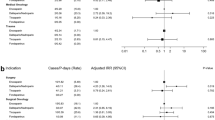
Background Although, guidelines for the appropriate use of enoxaparin are published, yet the extent of their implementation in clinical practice is still questionable. Furthermore, the optimal dosing of enoxaparin in special populations such as renal insufficiency and obesity remains controversial. In the Middle East, there are insufficient data on the appropriateness of enoxaparin use in different indications. Objective (1) To assess the appropriateness of enoxaparin dosing and duration per indication in compliance with the recommended guidelines and their impact on safety and efficacy outcomes in Lebanese health care centers. (2) To evaluate the influence of the hospital type (teaching vs. non-teaching) on the extent of compliance with established guidelines. Setting Seventeen health care centers in Lebanon, including teaching and non-teaching hospitals. Methods An observational, cross-sectional, multicenter study was conducted in 17 Lebanese hospitals. Data on demographics, indication, dosing regimen and clinical outcomes were collected. The appropriateness of dosing practices was determined as per the ACCP guidelines and the FDA dosing recommendations. Main outcome measure The appropriateness of enoxaparin dosing was compared across different hospital type and among special populations including severe renal insufficiency and very obese patients. Results Of the 463 patients who participated in the study, 40% received improper enoxaparin dosing, which was mostly observed in the VTE prophylaxis group (41.6%, P < 0.001). When comparing the overall dosing practices in Lebanese hospitals, there was no statistically significant difference in the correctness of enoxaparin dosing between teaching and non-teaching hospitals (61.6% vs. 58.2%, P = 0.449), respectively. Only 11.5% of renally impaired patients and 59.4% of obese patients received correct doses. Conclusion This study highlighted the improper practice and thus the need of implementation of clinical practice guidelines for the dosing of enoxaparin, in Lebanese hospitals.
Similar content being viewed by others
References
Cohen M, Demers C, Gurfinkel E, Turpie A, Fromell G, Goodman S, et al. A comparison of low molecular weight heparin with unfractionated heparin for unstable coronary artery disease. N Engl J Med. 1997;337(7):447–52.
Blazing M, de Lemos J, White H, Fox K, Verheugt F, Ardissino D, et al. Safety and efficacy of enoxaparin versus unfractionated heparin in patients with non-ST-segment elevation acute coronary syndromes who receive tirofiban and aspirin. A randomized controlled trial. JAMA. 2004;292(10):55–64.
Ferguson J, Califf R, Antman E, Cohen M, Grines C, Goodman S, et al. Enoxaparin versus unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes managed with an intended early invasive strategy. JAMA. 2004;292(1):45–54.
Quinlan DJ, McQuillan A, Eikelboom JW. Low-molecular-weight-heparin compared with intravenous heparin for treatment of pulmonary embolism. Ann Intern Med. 2004;140(3):175–83.
Merli G, Spiro T, Olsson C, Abildgaard U, Davidson B, Eldor A, et al. Subcutaneous enoxaparin once or twice daily compared with intravenous heparin for the treatment of venous thromboembolic disease. Ann Intern Med. 2001;134(3):191–202.
Boneu B. Low molecular weight heparins: are they superior to unfractionated heparins to prevent and to treat deep vein thrombosis? Thromb Res. 2000;100(2):V113–20.
Hirsh J, Warkentin T, Raschke R, Granger C, Ohman E, Dalen J. Heparin and low-molecular-weight heparin. Chest. 1999;115(6):489–510.
Weitz JI. Low-molecular-weight heparins. N Engl J Med. 1997;337(21):688–98.
Hirsh J, Bauer K, Donati M, Gould M, Samama M, Weitz J. Parenteral anticoagulants: American college of chest physicians evidence-based clinical practice guidelines (8th ed). Chest. 2008;133(6):141S–59S.
Geerts W, Bergqvist D, Pineo G, Heit J, Samama C, Lassen M, et al. Prevention of venous thromboembolism: American college of chest physicians evidence-based clinical practice guidelines (8th ed). Chest. 2008;133(6):381S–453S.
Kearon C, Kahn S, Agnelli G, Goldhaber S, Raskob G, Comerota A. Antithrombotic therapy for venous thromboembolic disease: American college of chest physicians evidence-based clinical practice guidelines (8th ed). Chest. 2008;133(6):454S–545S.
Harrington R, Becker R, Cannon C, Gutterman D, Lincoff A, Popma J, et al. Antithrombotic therapy for non ST segment elevation acute coronary syndromes: American college of chest physicians evidence-based clinical practice guidelines (8th ed). Chest. 2008;133(6):670S–707S.
Sanofi-Aventis US LLC. Lovenox® (enoxaparin sodium injection) prescribing information. Bridgewater: Sanofi-Aventis US LLC; 2008.
Chopard P, Dörffler-Melly J, Hess U, Wuillemin W, Hayoz D, Gallino A, et al. Venous thromboembolism prophylaxis in acutely ill medical patients: definite need for improvement. J Intern Med. 2005;257(4):352–7.
Becker R, Spencer F, Gibson M, Rush J, Sanderink G, Murphy S, et al. Influence of patient characteristics and renal function on factor Xa inhibition pharmacokinetics and pharmacodynamics after enoxaparin administration in non-ST elevation acute coronary syndromes. Am Heart J. 2002;143(5):753–9.
Mahe I, Gouin-Thibalt I, Drouet L, Simoneau G, Di Castillo H, Siguret V, et al. Elderly medical patients created with prophylactic dosages of enoxaparin: influence of renal function on anti-Xa activity level. Drugs Aging. 2007;24:63–71.
Lim W, Dentali F, Eikelboom JW, Crowther MA. Meta-analysis: low-molecular-weight heparin and bleeding in patients with severe renal insufficiency. Ann Intern Med. 2006;144(9):673–84.
Montalescot G, Collet J, Tanguy M, Ankri A, Payot L, Dumaine R, et al. Anti-Xa activity relates to survival and efficacy in unselected acute coronary syndrome patients treated with enoxaparin. Circulation. 2004;110(4):392–8.
Turpie A. Thrombosis prophylaxis in the acutely ill medical patient: insights from the prophylaxis in medical patients with enoxaparin (medenox) Trial. Am J Cardiol. 2000;86:48–52.
Cheymol G. Effects of obesity on pharmacokinetics implications for drug therapy. Clin Pharmacokinet. 2000;39(3):215–31.
Sanderink G, Le Liboux A, Jariwala N, Harding N, Ozoux M, Shukla U, et al. The pharmacokinetics and pharmacodynamics of enoxaparin in obese volunteers. Clin Pharmacol Ther. 2002;72(3):308–18.
Bazinet A, Almanric K, Brunet C, Turcotte I, Martineau J, Caron S, et al. Dosage of enoxaparin among obese and renal impairment patients. Thromb Res. 2005;116(1):41–50.
Wilson S, Wilbur K, Burton E, Anderson D. Effect of patient weight on the anticoagulant response to adjusted therapeutic dosage of low-molecular-weight heparin for the treatment of venous thromboembolism. Haemostasis. 2001;31(1):42–8.
Duplaga BA, Rivers CW, Nutescu E. Dosing and monitoring of low-molecular weight heparins in special populations. Pharmacotherapy. 2001;21(2):218–34.
Kucher N, Leizorovicz A, Vaitkus P, Cohen A, Turpie A, Olsson C, et al. Efficacy and safety of fixed low-dose dalteparin in preventing venous thromboembolism among obese or elderly hospitalized patients: a subgroup analysis of the PREVENT trial. Arch Intern Med. 2005;165(3):341–5.
Rondina M, Wheeler M, Rodgers G, Draper L, Pendleton R. Weight-based dosing of enoxaparin for VTE prophylaxis in morbidly obese, medically-ill patients. Thromb Res. 2010;125(3):220–3.
Vats V, Nutescu E, Theobald J, Wojtynek J, Schumock G. Survey of hospitals for guidelines, policies, and protocols for anticoagulants. Am J Health Syst Pharm. 2007;64(11):1203–8.
World Health Organization. Report of a WHO consultation on obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 1998.
Cockcroft DW, Gault MN. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41.
Macie C, Forbes L, Foster G, Douketis J. Dosing practices and risk factors for bleeding in patients receiving enoxaparin for the treatment of an acute coronary syndrome. Chest. 2004;125(5):1616–21.
Al-Sallami H, Jordan S, Ferguson R, Medlicott N, Schollum J, Duffull S. Current enoxaparin dosing guidelines have dubious credibility. N Z Med J. 2010;123(1313):62–7.
Taher AT, Aoun J, Salameh P. The AVAIL ME study: a multinational survey of VTE risk and prophylaxis. J Thromb Thrombolysis. 2011;31(1):47–56.
Rothberg M, Lahti M, Pekow P, Lindenauer P. Venous thromboembolism prophylaxis among medical patients at US hospitals. J Gen Intern Med. 2010;25(6):489–94.
Masroujeh R, Shamseddeen W, Isma’eel H, Otrock Z, Khalil I, Taher A, et al. Underutilization of venous thromboembolism prophylaxis in medical patients in a tertiary care center. J Thromb Thrombolysis. 2008;26(2):138–41.
Tincani E, Crowther M, Turrini F, Prisco D. Prevention and treatment of venous thromboembolism in the elderly population. Clin Interv Aging. 2007;2(2):237–46.
Spicer K, Gibson P, Bloe C, Cross S, Leslie S, et al. Weight assessment in cardiac patients: implications for prescription of low molecular weight heparin. Postgrad Med J. 2009;85(1001):124–7.
Scholten D, Hoedema R, Scholten S. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg. 2002;12(1):19–24.
Ellis M, Hadari R, Tchuvrero N, Shapira S, Kovlenko I, Kozmiakova M, et al. Hemorrhagic complications in patients treated with anticoagulant doses of low molecular weight heparin (enoxaparin) in routine hospital practice. Clin Appl Thromb Hemost. 2006;12(2):199–204.
Nieto J, Solano R, Ruiz-Ribo M, Ruiz-Gimenez N, Prandoni P, Kearon C, et al. Fatal bleeding in patients receiving anticoagulant therapy for venous thromboembolism: findings from the RIETE registry. Thromb Haemostasis. 2010;8(6):1216–22.
The Thrombolysis in Myocardial Infarction (TIMI) 11A Trial Investigators. Dose-ranging trial of enoxaparin for unstable angina: results of TIMT 11A. J Am Coll Cardiol. 1997;29(7):1474–82.
Gouin-Thibalt I, Pautas E, Siguret V. Safety profiles of different low molecular weight heparins used at therapeutic dose. Drug Saf. 2005;28(4):333–49.
Al-Sallami H, Barras M, Green B, Duffull S. Routine plasma anti-Xa monitoring is required for low-molecular-weight heparins. Clin Pharmacokinet. 2010;49(9):567–71.
Funding
No funding was received.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zeitoun, A.A., Nassif, J.G. & Zeineddine, M.M. The appropriateness of enoxaparin use in Lebanese hospitals: a quality evaluation study. Int J Clin Pharm 33, 934–941 (2011). https://doi.org/10.1007/s11096-011-9559-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-011-9559-1