Abstract
Background and Aims
Gastric acid plays an important role in the pathogenesis of gastric mucosal lesions. We investigated whether aspirin-induced gastric mucosal injury might have any association with the intragastric pH.
Materials and Methods
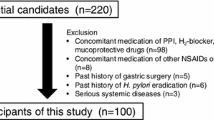
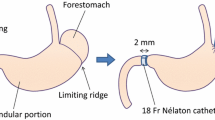
Fifteen healthy, Helicobacter pylori-negative volunteers randomly underwent the four different 7-day regimens: (1) aspirin 100 mg, (2) rabeprazole 10 mg, (3) aspirin 100 mg + rabeprazole 10 mg, and (4) aspirin 100 mg + rabeprazole 40 mg. Gastric mucosal injury based on the modified Lanza score (MLS), 24-h intragastric pH, and histopathology of gastric mucosa were evaluated prior to the start and on day 7 of each regimen.
Results
The median MLSs were 0 in the baseline and the rabeprazole 10 mg regimen. The median MLS in the aspirin regimen was 3, while those in both aspirin + rabeprazole 10 mg and aspirin + rabeprazole 40 mg regimens were 0. Rabeprazole significantly prevented the gastric mucosal injury by aspirin (P = 0.001 for rabeprazole 10 mg and P = 0.005 for rabeprazole 40 mg). The MLSs were negatively correlated with the 24-h intragastric pH (P = −0.711, < 0.001), whereas aspirin had no effect on the intragastric pH. Aspirin expanded the mean diameter of the microvessels of the gastric mucosa, which, in turn, was negatively correlated with the intragastric pH.
Conclusions
Aspirin might induce gastric mucosal injury by affecting the mucosal microvessels in an acid-dependent manner. Sustained maintenance of the intragastric pH at an elevated value is necessary to prevent gastric mucosal damage induced by aspirin.







Similar content being viewed by others
Abbreviations
- COX:
-
Cyclooxygenase
- CYP2C19:
-
Cytochrome P450 2C19
- H. pylori :
-
Helicobacter pylori
- IM:
-
Intermediate metabolizer
- MLS:
-
Modified Lanza score
- NSAID:
-
Non-steroidal anti-inflammatory drug
- PG:
-
Prostaglandin
- PM:
-
Poor metabolizer
- RM:
-
Rapid metabolizer
References
Nishikawa K, Sugiyama T, Kato M, et al. Non-Helicobacter pylori and non-NSAID peptic ulcer disease in the Japanese population. Eur J Gastroenterol Hepatol. 2000;12(6):635–640.
Awtry EH, Loscalzo J. Aspirin. Circulation. 2000;101(10):1206–1218.
Taha AS, Angerson WJ, Knill-Jones RP, Blatchford O. Upper gastrointestinal haemorrhage associated with low-dose aspirin and anti-thrombotic drugs - a 6-year analysis and comparison with non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2005;22(4):285–289.
Collaborative overview of randomised trials of antiplatelet therapy–I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. Bmj. 1994;308(6921):81-106.
Schoen RT, Vender RJ. Mechanisms of nonsteroidal anti-inflammatory drug-induced gastric damage. Am J Med. 1989;86(4):449–458.
Halter F. Mechanism of gastrointestinal toxicity of NSAIDs. Scand J Rheumatol Suppl. 1988;73:16–21.
Yeomans ND, Lanas AI, Talley NJ, et al. Prevalence and incidence of gastroduodenal ulcers during treatment with vascular protective doses of aspirin. Aliment Pharmacol Ther. 2005;22(9):795–801.
Derry S, Loke YK. Risk of gastrointestinal haemorrhage with long term use of aspirin: meta-analysis. BMJ. 2000;321(7270):1183–1187.
Pilotto A, Franceschi M, Leandro G, et al. Proton-pump inhibitors reduce the risk of uncomplicated peptic ulcer in elderly either acute or chronic users of aspirin/non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2004;20(10):1091–1097.
Serrano P, Lanas A, Arroyo MT, Ferreira IJ. Risk of upper gastrointestinal bleeding in patients taking low-dose aspirin for the prevention of cardiovascular diseases. Aliment Pharmacol Ther. 2002;16(11):1945–1953.
Furuta T, Shirai N, Sugimoto M, Ohashi K, Ishizaki T. Pharmacogenomics of proton pump inhibitors. Pharmacogenomics. 2004;5(2):181–202.
Furuta T, Shirai N, Takashima M, et al. Effect of genotypic differences in CYP2C19 on cure rates for Helicobacter pylori infection by triple therapy with a proton pump inhibitor, amoxicillin, and clarithromycin. Clin Pharmacol Ther. 2001;69(3):158–168.
Ishizaki T, Horai Y. Review article: cytochrome P450 and the metabolism of proton pump inhibitors—emphasis on rabeprazole. Aliment Pharmacol Ther. 1999;13(Suppl 3):27–36.
Yasuda S, Horai Y, Tomono Y, et al. Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′-hydroxylation status. Clin Pharmacol Ther. 1995;58(2):143–154.
Adachi K, Katsube T, Kawamura A, et al. CYP2C19 genotype status and intragastric pH during dosing with lansoprazole or rabeprazole. Aliment Pharmacol Ther. 2000;14(10):1259–1266.
Shirai N, Furuta T, Moriyama Y, et al. Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther. 2001;15(12):1929–1937.
Ieiri I, Kishimoto Y, Okochi H, et al. Comparison of the kinetic disposition of and serum gastrin change by lansoprazole versus rabeprazole during an 8-day dosing scheme in relation to CYP2C19 polymorphism. Eur J Clin Pharmacol. 2001;57(6–7):485–492.
Horai Y, Kimura M, Furuie H, et al. Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther. 2001;15(6):793–803.
Lanza FL, Royer GL Jr, Nelson RS, Chen TT, Seckman CE, Rack MF. A comparative endoscopic evaluation of the damaging effects of nonsteroidal anti-inflammatory agents on the gastric and duodenal mucosa. Am J Gastroenterol. 1981;75(1):17–21.
Naito Y, Yoshikawa T, Iinuma S, et al. Rebamipide protects against indomethacin-induced gastric mucosal injury in healthy volunteers in a double-blind, placebo-controlled study. Dig Dis Sci. 1998;43(9 Suppl):83S–89S.
Dixon MF, Genta RM, Yardley JH, Correa P. Classification, grading of gastritis. The updated Sydney System. International workshop on the histopathology of gastritis Houston, 1994. Am J Surg Pathol. 1996;20(10):1161–1181.
Svedlund J, Sjodin I, Dotevall G. GSRS—a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988;33(2):129–134.
Funatsu T, Chono K, Hirata T, Keto Y, Kimoto A, Sasamata M. Mucosal acid causes gastric mucosal microcirculatory disturbance in nonsteroidal anti-inflammatory drug-treated rats. Eur J Pharmacol. 2007;554(1):53–59.
Elliott SL, Ferris RJ, Giraud AS, Cook GA, Skeljo MV, Yeomans ND. Indomethacin damage to rat gastric mucosa is markedly dependent on luminal pH. Clin Exp Pharmacol Physiol. 1996;23(5):432–434.
Kitchingman GK, Prichard PJ, Daneshmend TK, Walt RP, Hawkey CJ. Enhanced gastric mucosal bleeding with doses of aspirin used for prophylaxis and its reduction by ranitidine. Br J Clin Pharmacol. 1989;28(5):581–585.
Savarino V, Mela GS, Zentilin P, et al. Effect of one-month treatment with nonsteroidal antiinflammatory drugs (NSAIDs) on gastric pH of rheumatoid arthritis patients. Dig Dis Sci. 1998;43(3):459–463.
Janssen M, Baak LC, Jansen JB, Dijkmans BA, Vandenbroucke JP, Lamers CB. Effects of indomethacin on intragastric pH and meal-stimulated serum gastrin secretion in rheumatoid arthritis patients. Aliment Pharmacol Ther. 1993;7(4):393–400.
Odashima M, Otaka M, Jin M, et al. Attenuation of gastric mucosal inflammation induced by aspirin through activation of A2A adenosine receptor in rats. World J Gastroenterol. 2006;12(4):568–573.
Wallace JL, Zamuner SR, McKnight W, et al. Aspirin, but not NO-releasing aspirin (NCX-4016), interacts with selective COX-2 inhibitors to aggravate gastric damage and inflammation. Am J Physiol Gastrointest Liver Physiol. 2004;286(1):G76–G81.
Yao T, Kato M, Asaka M. Pathology of gastric mucosal injury induced by low-dose aspirin. Gi Forefr. 2007;3(1):32–36. Japanese.
Kitahora T, Guth PH. Effect of aspirin plus hydrochloric acid on the gastric mucosal microcirculation. Gastroenterology. 1987;93(4):810–817.
Shimatani T, Inoue M, Kuroiwa T, et al. Acid-suppressive efficacy of a reduced dosage of rabeprazole: comparison of 10 mg twice daily rabeprazole with 20 mg twice daily rabeprazole, 30 mg twice daily lansoprazole, and 20 mg twice daily omeprazole by 24-hr intragastric pH-metry. Dig Dis Sci. 2005;50(7):1202–1206.
Acknowledgments
This study was supported by a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (20590718) and (20014007) and grants from Ministry of Health, Labour and Welfare (19-19). The abstract of the study was presented at the Annual Meeting of the American Gastroenterological Association held in San Diego, CA, USA, in May 2008. We greatly appreciate the help of our endoscopy room staff, Ms. Chieko Matsumoto, Ms Kinuko Maruyama, Ms Satoko Takebayashi, Ms Keiko Kikuchi and Ms Hitomi Tanaka.
Conflict of Interest Statement
None of the authors have any conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Study highlights: we demonstrate for the first time that low dose aspirin induces gastric mucosal injury in the intragastric acidity-dependent manner in humans. We also show that aspirin induces dilatation of gastric subepithelial microvessels, which also depends on intragastric acidity. These endoscopic and histopathological changes can be prevented by concomitant treatment with rabeprazole, a proton-pump inhibitor.
Rights and permissions
About this article
Cite this article
Nishino, M., Sugimoto, M., Kodaira, C. et al. Relationship Between Low-Dose Aspirin-Induced Gastric Mucosal Injury and Intragastric pH in Healthy Volunteers. Dig Dis Sci 55, 1627–1636 (2010). https://doi.org/10.1007/s10620-009-0920-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0920-3