Abstract
Speech pathologists are often the first professionals to identify signs of a cricopharyngeal (CP) dysfunction and make recommendations for further care. There are many care options for patients with CP dysfunction, but it is unclear how certain interventions are used in practice. A paper-based survey employing two clinical cases involving suspected CP dysfunction (Case 1 with adequate pharyngeal strength and Case 2 with coexisting pharyngeal weakness) was sent to members of American Speech-Language Hearing Association’s Special Interest Group 13. Respondents ranked the order of management approaches (swallowing therapy, further evaluation, and referral to another medical professional) and selected specific interventions under each approach that they would recommend for each case. Completed surveys from 206 respondents were entered into analysis. The majority of the respondents recommended swallowing therapy as a first approach for each case (Case 1: 64 %; Case 2: 88 %). The most prevalent swallowing exercises recommended were the Shaker (73 %), effortful swallow (62 %), and Mendelsohn maneuver (53 %) for Case 1 and effortful swallow (92 %), Shaker (84 %), and tongue-hold swallow (73 %) for Case 2. 76 % of respondents recommended a referral for Case 1, while 38 % recommended the same for Case 2. Respondents with access to more types of evaluative tools were more likely to recommend further evaluation, and those with access to only videofluoroscopy were less likely to recommend further evaluation. However, the high degree of variability in recommendations reflects the need for best practice guidelines for patients with signs of CP dysfunction.



Similar content being viewed by others
References
Shaker R, Lang IM. Reflex mediated airway protective mechanisms against retrograde aspiration. Am J Med. 1997;103:64S–73S.
Szczesniak MM, Fuentealba SE, Burnett A, Cook IJ. Differential relaxation and contractile responses of the human upper esophageal sphincter mediated by interplay of mucosal and deep mechanoreceptor activation. Am J Physiol Gastrointest Liver Physiol. 2008;294:G982–8.
Chernichenko N, Woo JS, Hundal JS, Sasaki CT. Response of cricopharyngeus muscle to esophageal stimulation by mechanical distension and acid and bile perfusion. Ann Otol Rhinol Laryngol. 2011;120:137–42.
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Kahrilas PJ. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects using solid-state high-resolution manometry. Am J Physiol Gastrointest Liver Physiol. 2006;291:G525–31.
Butler SG, Stuart A, Castell D, Russell GB, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume on pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52:240–53.
Shaker R, Ren J, Kern M, Dodds WJ, Hogan WJ, Li Q. Mechanisms of airway protection and upper esophageal sphincter opening during belching. Am J Physiol. 1992;262:G621–8.
Perera L, Kern M, Hofmann C, Tatro L, Chai K, Kuribayashi S, Lawal A, Shaker R. Manometric evidence for a phonation-induced UES contractile reflex. Am J Physiol Gastrointest Liver Physiol. 2008;294:G885–91.
Kahrilas PJ, Dodds WJ, Dent J, Haeberle B, Hogan WJ, Arndorfer RC. Effect of sleep, spontaneous gastroesophageal reflux, and a meal on upper esophageal sphincter pressure in normal human volunteers. Gastroenterology. 1987;92:466–71.
Pasricha PJ. Effect of sleep on gastroesophageal physiology and airway protective mechanisms. Am J Med. 2003;115(Suppl 3A):114S–8S.
Ekberg O, Nylander G. Dysfunction of the cricopharyngeal muscle: a cineradiographic study of patients with dysphagia. Radiology. 1982;143:481–6.
Curtis DJ, Cruess DF, Berg T. The cricopharyngeal muscle: a videorecording review. AJR Am J Roentgenol. 1984;142:497–500.
Baredes S, Shah CS, Kaufman R. The frequency of cricopharyngeal dysfunction on videofluoroscopic swallowing studies in patients with dysphagia. Am J Otolaryngol. 1997;18:185–9.
Schultz AR, Niemtzow P, Jacobs SR, Naso F. Dysphagia associated with cricopharyngeal dysfunction. Arch Phys Med Rehabil. 1979;60:381–6.
Yip HT, Leonard R, Kendall KA. Cricopharyngeal myotomy normalizes the opening size of the upper esophageal sphincter in cricopharyngeal dysfunction. Laryngoscope. 2006;116:93–6.
Mason RJ, Bremner CG, DeMeester TR, Crookes PF, Peters JH, Hagen JA, DeMeester SR. Pharyngeal swallowing disorders: selection for and outcome after myotomy. Ann Surg. 1998;228:598–607.
Ozgursoy OB, Salassa JR. Manofluorographic and functional outcomes after endoscopic laser cricopharyngeal myotomy for cricopharyngeal bar. Otolaryngol Head Neck Surg. 2010;142:735–40.
Brøndbo K. Treatment of cricopharyngeal dysfunction by endoscopic laser myotomy. Acta Otolaryngol Suppl. 2000;543:222–4.
Cook IJ. Cricopharyngeal function and dysfunction. Dysphagia. 1993;8:244–51.
Kristmundsdottir F, Mahon M, Froes MM, Cumming WJ. Histomorphometric and histopathological study of the human cricopharyngeus muscle: in health and in motor neuron disease. Neuropathol Appl Neurobiol. 1990;16:461–75.
Laurikainen E, Aitasalo K, Halonen P, Falck B, Kalimo H. Muscle pathology in idiopathic cricopharyngeal dysphagia. Enzyme histochemical and electron microscopic findings. Eur Arch Otorhinolaryngol. 1992;249:216–23.
Williams RB, Wallace KL, Ali GN, Cook IJ. Biomechanics of failed deglutitive upper esophageal sphincter relaxation in neurogenic dysphagia. Am J Physiol Gastrointest Liver Physiol. 2002;283:G16–26.
Alfonsi E, Versino M, Merlo IM, Pacchetti C, Martignoni E, Bertino G, Moglia A, Tassorelli C, Nappi G. Electrophysiologic patterns of oral-pharyngeal swallowing in parkinsonian syndromes. Neurology. 2007;68:583–9.
Speyer R, Baijens L, Heijnen M, Zwijnenberg I. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25:40–65.
Bartolome G, Neumann S. Swallowing therapy in patients with neurological disorders causing cricopharyngeal dysfunction. Dysphagia. 1993;8:146–9.
Shaker R, Kern M, Bardan E, Taylor A, Stewart ET, Hoffmann RG, Arndorfer RC, Hofmann C, Bonnevier J. Augmentation of deglutitive upper esophageal sphincter opening in the elderly by exercise. Am J Physiol Gastrointest Liver Physiol. 1997;272:G1518–22.
Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, Grande B, Kazandjian M, Dikeman K. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002;122:1314–21.
Logemann JA, Rademaker A, Pauloski BR, Kelly A, Stangl-McBreen C, Antinoja J, Grande B, Farquharson J, Kern M, Easterling C, Shaker R. A randomized study comparing the Shaker exercise with traditional therapy: a preliminary study. Dysphagia. 2009;24:403–11.
Regan J, Walshe M, McMahon BP. Current evaluation of upper oesophageal sphincter opening in dysphagia practice: an international SLT survey. Int J Lang Commun Disord. 2012;47:156–65.
Ali GN, Wallace KL, Laundl TM, Hunt DR, deCarle DJ, Cook IJ. Predictors of outcome following cricopharyngeal disruption for pharyngeal dysphagia. Dysphagia. 1997;12:133–9.
Born LJ, Harned RH, Rikkers LF, Pfeiffer RF, Quigley EM. Cricopharyngeal dysfunction in Parkinson’s disease: role in dysphagia and response to myotomy. Move Disord. 1996;11:53–8.
Schneider I, Pototschnig C, Thumfart WF, Eckel HE. Treatment of dysfunction of the cricopharyngeal muscle with botulinum A toxin: introduction of a new, noninvasive method. Ann Otol Rhinol Laryngol. 1994;103:31–5.
Schindler JS, Kelly JH. State of the art review: swallowing disorders in the elderly. Laryngoscope. 2002;112:589–602.
St Guily JL, Moine A, Perie S, Bokowy C, Angelard B, Chaussade S. Role of pharyngeal propulsion as an indicator for upper esophageal sphincter myotomy. Laryngoscope. 1995;105:723–7.
Institute of Medicine Roundtable on Evidence-Based Medicine. The National Academies Collection: Reports funded by National Institutes of Health. In: Yong PL, Saunders RS, Olsen LA, editors. The healthcare imperative: lowering costs and improving outcomes: Workshop series summary. Washington, DC: National Academies Press; 2010.
Alfonsi E, Merlo IM, Ponzio M, Montomoli C, Tassorelli C, Biancardi C, Lozza A, Martignoni E. An electrophysiological approach to the diagnosis of neurogenic dysphagia: implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatr. 2010;81:54–60.
Chiu MJ, Chang YC, Hsiao TY. Prolonged effect of botulinum toxin injection in the treatment of cricopharyngeal dysphagia: case report and literature review. Dysphagia. 2004;19:52–7.
Masiero S, Briani C, Marchese-Ragona R, Giacometti P, Costantini M, Zaninotto G. Successful treatment of long-standing post-stroke dysphagia with botulinum toxin and rehabilitation. J Rehabil Med. 2006;38:201–3.
Terre R, Valles M, Panades A, Mearin F. Long-lasting effect of a single botulinum toxin injection in the treatment of oropharyngeal dysphagia secondary to upper esophageal sphincter dysfunction: a pilot study. Scand J Gastroenterol. 2008;43:1296–303.
Allen J, White CJ, Leonard R, Belafsky PC. Effect of cricopharyngeus muscle surgery on the pharynx. Laryngoscope. 2010;120:1498–503.
Murry T, Wasserman T, Carrau RL, Castillo B. Injection of botulinum toxin A for the treatment of dysfunction of the upper esophageal sphincter. Am J Otolaryngol. 2005;26:157–62.
Solt J, Bajor J, Moizs M, Grexa E, Horvath PO. Primary cricopharyngeal dysfunction: treatment with balloon catheter dilatation. Gastrointest Endosc. 2001;54:767–71.
Kelly JH. Management of upper esophageal sphincter disorders: indications and complications of myotomy. Am J Med. 2000;108(Suppl 4a):43S–6S.
Jacobs JR, Logemann J, Pajak TF, Pauloski BR, Collins S, Casiano RR, Schuller DE. Failure of cricopharyngeal myotomy to improve dysphagia following head and neck cancer surgery. Arch Otolaryngol Head Neck Surg. 1999;125:942–6.
Oh TH, Brumfield KA, Hoskin TL, Kasperbauer JL, Basford JR. Dysphagia in inclusion body myositis: clinical features, management, and clinical outcome. Am J Phys Med Rehabil. 2008;87:883–9.
Shama L, Connor NP, Ciucci MR, McCulloch TN. Surgical treatment of dysphagia. Phys Med Rehabil Clin N Am. 2008;19:817–35.
Campbell BH, Tuominen TC, Toohill RJ. The risk and complications of aspiration following cricopharyngeal myotomy. Am J Med. 1997;103:61S–3S.
Takes RP, van den Hoogen FJ, Marres HA. Endoscopic myotomy of the cricopharyngeal muscle with CO2 laser surgery. Head Neck. 2005;27:703–9.
Krause E, Schirra J, Gurkov R. Botulinum toxin A treatment of cricopharyngeal dysphagia after subarachnoid hemorrhage. Dysphagia. 2008;23:406–10.
Acknowledgments
This study was supported by National Institutes of Health grant number R21 DC011130A from the National Institute on Deafness and Other Communicative Disorders and by the Diane M. Bless Chair in Otolaryngology at University of Wisconsin-Madison. The authors acknowledge Department of Surgery biostatistician Glen Leverson, Ph.D., for his assistance with statistical analysis.
Conflict of interest
The authors declare that they have no conflict of interest associated with this article.
Author information
Authors and Affiliations
Corresponding author
Appendix: Transcript of Survey
Appendix: Transcript of Survey
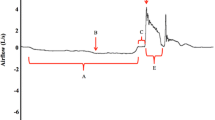
Case #1: You saw an 81-year-old female with complaints of food sticking in her throat and needing a long time to eat meals. She is eating a diet consisting of soft solids and thin liquids. She has no history of recent pneumonia and has had a gradual weight loss of 15 lb. over 5 years. She is cognitively intact, has no significant neurological history, and has no history of gastroesophageal reflux. A VFSS revealed a swallow pattern characterized by:
-
Functional oral phase
-
Adequate tongue base to posterior pharyngeal wall retraction and bolus propulsion
-
Timely pharyngeal swallow trigger for age
-
Reduced hyolaryngeal excursion
-
Narrow UES opening with a CP prominence needing multiple swallows to clear bolus
-
Stasis in the valleculae and pyriform sinuses
-
Penetration of thin liquid to the vocal folds without a cough response
-
No aspiration events
Neither postural changes (e.g., head turn, chin tuck) nor swallow maneuvers (e.g., Mendelsohn) reduced the degree of stasis or penetration or the amount of material that cleared through the UES on the initial swallow.
Case #2: You saw a 70-year-old male who is 1-year status post a fall that resulted in a right subdural hematoma and has been discharged from a rehab facility for 2 months. An oral mechanism exam revealed decreased lingual range of motion and strength (though his speech is intelligible), but no other significant findings. He is currently NPO, expectorating saliva/secretions instead of swallowing, and is getting nutrition/hydration via PEG tube. He is cognitively intact and hoping to return to an oral diet soon. A VFSS revealed a swallow pattern characterized by:
-
Functional oral phase
-
Dilated pharynx with poor tongue base propulsion and reduced pharyngeal constriction
-
Delay of pharyngeal swallow to the valleculae with thin liquids
-
Reduced hyolaryngeal excursion
-
Narrow UES opening needing multiple swallows to clear bolus
-
Stasis in the pyriform sinuses
-
Aspiration of thin liquid from stasis in the pyriform sinus without a cough response
A left head turn mildly improved the amount of material that cleared through the UES on the initial swallow but did not reduce the degree of stasis or aspiration.
After each case, respondents were given the following options:
Given the resources currently at your disposal, please indicate your primary and subsequent management approach(es) (e.g., 1, 2, etc.) and mark the specific interventions you would pursue under each approach.
-
Swallowing therapy
-
Oral motor exercises (range-of-motion and/or resistance)
-
Supraglottic and/or super-supraglottic swallow
-
Vocal fold adduction exercises
-
Falsetto exercise
-
Effortful swallow
-
Masako maneuver (tongue-hold swallow)
-
Mendelsohn maneuver
-
Shaker (head lift) exercise
-
Therapy with external device (e.g., IOPI)
-
Biofeedback therapy (e.g., submental surface EMG)
-
Thermal-tactile stimulation
-
Neuromuscular Electrical Stimulation (NMES)
-
-
Further evaluation
-
FEES
-
Conventional manometry (1–6 pressure transducers)
-
High-resolution manometry (20+ pressure transducers)
-
Intraluminal impedance
-
EMG
-
EGG
-
-
Consult physician for surgical management
Rights and permissions
About this article
Cite this article
Jones, C.A., Knigge, M.A. & McCulloch, T.M. Speech Pathologist Practice Patterns for Evaluation and Management of Suspected Cricopharyngeal Dysfunction. Dysphagia 29, 332–339 (2014). https://doi.org/10.1007/s00455-013-9513-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9513-6