Abstract
Purpose
To compare the delivery and neonatal outcome of IVF singleton pregnancies with those conceived spontaneously in primiparous women ≥35 years of age.
Methods
Data were collected by the hospital’s obstetrics and pediatric staff at the time of examination, hospitalization, delivery and discharge. A total of 283 women with in vitro fertilization (IVF) singleton deliveries were matched according to ethnicity, age, gravidity, smoking habits, body mass index, weight gain in pregnancy, site and time of delivery with consecutive 283 women conceived spontaneously. The outcome measures were mode of delivery, birth weight, preterm birth and perinatal mortality.
Results
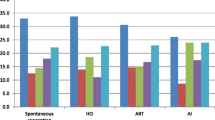
Cesarean delivery rate was more common in IVF pregnancies (39.9% vs. 25.1%; p < 0.001). Preterm delivery rate, specifically of spontaneous onset was significantly higher in IVF group (18.7%) than in spontaneous conception group (10.3%; p < 0.008). No difference was found in birth weight records (SGA, VLBW, LBW and LGA) or perinatal mortality rate. However, average gestational birth weight was lower among infants conceived after IVF (3,050 ± 587 g vs. 3,130 ± 524 g; p < 0.05).
Conclusions
Singleton IVF pregnancies in primiparous women ≥35 years of age have increased perinatal risk associated with higher rates of cesarean section, preterm births and infants of lower average birth weight. Nevertheless, pregnancy and delivery complications, number of infants with low or very low birth weight, small or large birth weight for appropriate gestation did not differ from those of the spontaneous conceptions.

Similar content being viewed by others
References
Tan SL, Doyle P, Campbell S et al (1992) Obstetric outcome of in vitro fertilization pregnancies compared with normally conceived pregnancies. Am J Obstet Gynecol 167:778–784
Though SC, Greene CA, Svenson LW, Belik J (2000) Effects of in vitro fertilization on low birth weight, preterm delivery, and multiple birth. J Pediatr 136:618–622
Perri T, Chen R, Yoeli R et al (2001) Are singleton assisted reproductive technology pregnancies at risk of prematurity? J Assist Reprod Genet 18:245–249
Wang JX, Clark AM, Kirby CA, Philipson G, Petrucco O, Anderson G, Matthews CD (1994) The obstetric outcome of singleton pregnancies following in vitro fertilization/gamete intra-fallopian transfer. Hum Reprod 9:141–146
Wang Y, Sullivan E, Black D, Dean J, Bryant J, Chapman M (2005) Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertil Steril 83:1650–1658
Koivurova S, Hartikainen AL, Gissler M, Hemminki E, Sovio U, Jarvelin MR (2002) Neonatal outcome and congenital malformations in children born after in vitro fertilization. Hum Reprod 17:1391–1398
Rimm AA, Katayama AC, Diaz M, Katayama KP (2004) A meta-analysis of controlled studies comparing major malformation rates in IVF and ICSI infants with naturally conceived children. J Assist Reprod Genet 21:437–443
Isaksson R, Gissler M, Tiitinen A (2002) Obstetric outcome among women with unexplained infertility after IVF: a matched case–control study. Hum Reprod 17:1755–1761
Koudstaal J, Braat DD, Bruinse HW, Naaktgeboren N, Vermeiden JP, Visser GH (2005) Obstetric outcome of singleton pregnancies after IVF: a matched control study in four Dutch university hospitals. Hum Reprod 15:1819–1825
Ochsenkühn R, Strowitzki T, Gurtner M, Strauss A, Schulze A, Hepp H, Hillemanns P (2003) Pregnancy complications, obstetric risks, and neonatal outcome in singleton and twin pregnancies after GIFT and IVF. Arch Gynecol Obstet 268:256–261
Buckett WM, Chian RC, Holzer H, Dean N, Usher R, Tan SL (2007) Obstetric outcomes and congenital abnormalities after in vitro maturation, in vitro fertilization, and intracytoplasmic sperm injection. Obstet Gynecol 110:885–891
Simunic V, Tomic V, Tomic J, Nizic D (2007) Comparative study of the efficacy and tolerability of two vaginal progesterone formulations, Crinone 8% gel and Utrogestan capsules, used for luteal support. Fertil Steril 87:83–87
Jackson RA, Gibson KA, Wu YM, Croughan MS (2004) Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol 103:551–563
McDonalds SD, Murphy K, Beyene J, Ohlsson A (2005) Perinatal outcomes of singleton pregnancies achieved by in vitro fertilization: a systematic review and meta-analysis. J Obstet Gynaecol Can 27:449–459
McGovern PG, Llorens AJ, Skurnick JH, Weiss G, Goldsmith LT (2004) Increased risk of preterm birth in singleton pregnancies resulting from in vitro fertilization-embryo transfer or gamete intrafallopian transfer: a meta-analysis. Fertil Steril 82:1514–1520
Schieve LA, Ferre C, Peterson HB, Macaluso M, Reynolds MA, Wright VC (2004) Perinatal outcome among singleton infants conceived through assisted reproductive technology in the United States. Obstet Gynecol 103:1144–1153
Mushayandebvu TI, Goldsmith LT, Von Hagen S, Santoro N, Thurston D, Weiss G (1998) Elevated maternal serum relaxin concentrations throughout pregnancy in singleton gestations after superovulation. Obstet Gynecol 92:17–20
Weiss G, Goldsmith LT, Sachdev R, Von Hagen S, Lederer K (1993) Elevated first-trimester serum relaxin concentrations in pregnant women following ovarian stimulation predict prematurity risk and preterm delivery. Obstet Gynecol 82:821–828
Luke B, Brown MB (2007) Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil Steril 88:283–293
Suzuki S, Miyake H (2008) Obstetric outcomes in nulliparous women aged 35 and over with singleton pregnancies conceived by in vitro fertilization. Arch Gynecol Obstet 277:225–227
Ahlborg L, Ek S, Fridström M, Kublickas M, Leijon M, Nisell H (2006) Is fetal growth impaired after in vitro fertilization? Acta Obstet Gynecol Scand 85:195–199
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tomic, V., Tomic, J. Neonatal outcome of IVF singletons versus naturally conceived in women aged 35 years and over. Arch Gynecol Obstet 284, 1411–1416 (2011). https://doi.org/10.1007/s00404-011-1873-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-1873-2