Abstract
Objective
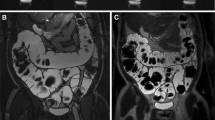
To assess the feasibility and utility of magnetic resonance (MR) imaging of the bowel in concurrent small- and large-bowel evaluation for the presence of inflammatory bowel disease (IBD).
Methods
Over a 5-year period, 62 MR examinations performed on 53 patients demonstrated evidence of IBD. Sixteen of these 53 (30.1%) patients had imaging findings of colonic disease and underwent 19 formal MR small bowel examinations. These were further evaluated for bowel distention and image quality. The sensitivity and specificity of the technique compared with colonoscopy as the ‘gold standard’ was evaluated.
Results
Simultaneous imaging of the colon is feasible at MR small bowel follow-through with moderate-to-excellent colonic visibility and colon distention obtained when the contrast medium is present in the colon at the time of image acquisition. MR imaging had a sensitivity of 80% (0.56–0.93), specificity of 100% (0.77-1.00), positive predictive value (PPV) of 1 and a negative predictive value (NPV) of 0.8 for the identification of colitis (based on available concurrent correlation of 38/62 examinations with colonoscopy).
Conclusion
Small and large bowel MR imaging with orally consumed contrast medium represents a promising, feasible, non-invasive, non-radiating single mode of assessment of the entire gastrointestinal tract, performed at a single sitting.





Similar content being viewed by others
References
Paonessa NJ, Rosen L, Stasik JJ (2005) Using the gastroscope for incomplete colonoscopy. Dis Colon Rectum 48:851–854
Dafnis G, Granath F, Påhlman L et al (2005) Patient factors influencing the completion rate in colonoscopy. Dig Liver Dis 37:113–118
Langhorst J, Kühle CA, Ajaj W et al (2007) MR colonography without bowel purgation for the assessment of inflammatory bowel diseases: diagnostic accuracy and patient acceptance. Inflamm Bowel Dis 13:1001–1008
Schreyer AG, Rath HC, Kikinis R et al (2005) Comparison of magnetic resonance imaging colonography with conventional colonoscopy for the assessment of intestinal inflammation in patients with inflammatory bowel disease: a feasibility study. Gut 54:250–256
Röttgen R, Herzog H, Lopez-Hänninen E et al (2005) Combination of dynamic MR enteroclysis (Sellink) and MR colonography to diagnose Crohn’s disease. Rofo 177:1131–1138
Fidler J (2007) MR imaging of the small bowel. Radiol Clin North Am 45:317–331
Masselli G, Casciani E, Polettini E et al (2008) Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur Radiol 18:438–447
Negaard A, Paulsen V, Sandvik L et al (2007) A prospective randomized comparison between two MRI studies of the small bowel in Crohn’s disease, the oral contrast method and MR enteroclysis. Eur Radiol 17:2294–2301
Lee SS, Kim AY, Yang SK et al (2009) Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology 251:751–761
Laghi A, Carbone I, Catalano C et al (2001) Polyethylene glycol solution as an oral contrast agent for MR imaging of the small bowel. AJR Am J Roentgenol 177:1333–1334
McKenna DA, Roche CJ, Murphy JM et al (2006) Polyethylene glycol solution as an oral contrast agent for MRI of the small bowel in a patient population. Clin Radiol 61:966–970
Laghi A, Paolantonio P, Catalano C et al (2003) MRI of the small bowel using polyethylene glycol solution as an oral contrast agent in adults and children with celiac disease: preliminary observations. AJR Am J Roentgenol 180:191–194
Cronin CG, Lohan DG, Ni Mhuircheartaigh J et al (2008) MR small bowel follow through (MRSBFT)—prone versus supine patient positioning for best small bowel distension and lesion detection. AJR Am J Roentgenol 191:502–506
Lohan DG, Alhajeri AN, Cronin CG et al (2008) MR enterographic appearances of small bowel lymphoma: potential for suggestion of histological subtype and presence of underlying celiac disease. AJR Am J Roentgenol 190:287–293
Cronin CG, Lohan DG, Delappe E et al (2008) Duodenal pathology at MR Small Bowel Follow-Through (MRSBFT)—the duodenum revisited. AJR Am J Roentgenol 191:1082–1092
Lohan D, Cronin C, Meehan C et al (2007) MR small bowel enterography: optimization of imaging timing. Clin Radiol 62:804–807
Paolantonio P, Tomei E, Rengo M et al (2007) Adult celiac disease: MRI findings. Abdom Imaging 32:433–440
Paolantonio P, Rengo M, Iafrate F et al (2006) Diagnosis of Taenia saginata by MR enterography. AJR Am J Roentgenol 187:W238
Acknowledgments
In the ‘Introduction’ and ‘Methods’ the authors acknowledge that their currently analysed patient group is from a similar database to previous papers (e.g. references [13–15]). However this study is unique in its objective of assessing the ability of MRSBFT to allow single-study depiction of IBD, enteritis and colitis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cronin, C.G., Lohan, D.G., Browne, A.M. et al. Does MRI with oral contrast medium allow single-study depiction of inflammatory bowel disease enteritis and colitis?. Eur Radiol 20, 1667–1674 (2010). https://doi.org/10.1007/s00330-009-1701-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1701-2