Abstract
Background
Bowel rotation abnormalities in heterotaxy are common. As more children survive cardiac surgery, the management of gastrointestinal abnormalities has become controversial.
Objective
To evaluate imaging of malrotation in heterotaxy with surgical correlation and provide an algorithm for management.
Materials and methods
Imaging reports of heterotaxic children with upper gastrointestinal (UGI) and/or small bowel follow-through (SBFT) were reviewed. Subsequently, fluoroscopic images were re-reviewed in conjunction with CT/MR studies. The original reports and re-reviewed images were compared and correlated with surgical findings.
Results
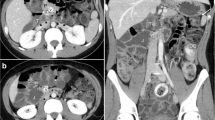
Nineteen of 34 children with heterotaxy underwent UGI, 13/19 also had SBFT. In 15/19 reports, bowel rotation was called abnormal: 11 malrotation, 4 non-rotation, no cases of volvulus. Re-review, including CT (10/19) and MR (2/19), designated 17/19 (90%) as abnormal, 10 malrotation (abnormal bowel arrangement, narrow or uncertain length of mesentery) and 7 non-rotation (small bowel and colon on opposite sides plus low cecum with probable broad mesentery). The most useful CT/MR findings were absence of retroperitoneal duodenum in most abnormal cases and location of bowel, especially cecum. Abnormal orientation of mesenteric vessels suggested malrotation but was not universal. Nine children had elective bowel surgery; non-rotation was found in 4/9 and malrotation was found in 5/9, with discrepancies (non-rotation at surgery, malrotation on imaging) with 4 original interpretations and 1 re-review.
Conclusion
We recommend routine, early UGI and SBFT studies once other, urgent clinical concerns have been stabilized, with elective laparoscopic surgery in abnormal or equivocal cases. Cross-sectional imaging, usually obtained for other reasons, can contribute diagnostically. Attempting to assess mesenteric width is important in differentiating non-rotation from malrotation and more accurately identifies appropriate surgical candidates.





Similar content being viewed by others
References
Daneman A (2009) Malrotation: the balance of evidence. Pediatr Radiol 39:S164–S166
Choi M, Borenstein SH, Hornberger L et al (2005) Heterotaxia syndrome: the role of screening for intestinal rotation abnormalities. Arch Dis Child 90:813–815
Strouse PJ (2004) Disorders of intestinal rotation and fixation ("malrotation"). Pediatr Radiol 34:837–851
Taylor GA (2011) CT appearance of the duodenum and mesenteric vessels in children with normal and abnormal bowel rotation. Pediatr Radiol 41:1378–1383
Yousefzadeh DK (2009) The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol 39:S172–S177
Tashjian DB, Weeks B, Brueckner M et al (2007) Outcomes after a Ladd procedure for intestinal malrotation with heterotaxia. J Pediatr Surg 42:528–531
Lee SE, Kim HY, Jung SE et al (2006) Situs anomalies and gastrointestinal abnormalities. J Pediatr Surg 41:1237–1242
Papillon S, Goodhue CJ, Zmora O et al (2013) Congenital heart disease and heterotaxy: upper gastrointestinal fluoroscopy can be misleading and surgery in an asymptomatic patient is not beneficial. J Pediatr Surg 48:164–169
Yu DC, Thiagarajan RR, Laussen PC et al (2009) Outcomes after the Ladd procedure in patients with heterotaxy syndrome, congenital heart disease, and intestinal malrotation. J Pediatr Surg 44:1089–1095, discussion 1095
Watanabe T, Nakano M, Yamazawa K et al (2011) Neonatal intestinal volvulus and preduodenal portal vein associated with situs ambiguus: report of a case. Surg Today 41:726–729
Pockett CR, Dicken B, Rebeyka IM et al (2013) Heterotaxy syndrome: is a prophylactic Ladd procedure necessary in asymptomatic patients? Pediatr Cardiol 34:59–63
Applegate KE (2009) Evidence-based diagnosis of malrotation and volvulus. Pediatr Radiol 39:S161–S163
Long FR, Kramer SS, Markowitz RI et al (1996) Radiographic patterns of intestinal malrotation in children. Radiographics 16:547–556, discussion 556-560
Karmazyn B (2013) Duodenum between the aorta and the SMA does not exclude malrotation. Pediatr Radiol 43:121–122
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Newman, B., Koppolu, R., Murphy, D. et al. Heterotaxy syndromes and abnormal bowel rotation. Pediatr Radiol 44, 542–551 (2014). https://doi.org/10.1007/s00247-013-2861-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2861-4