Abstract
Introduction
Cardiac right-to-left shunt (RLS), mainly due to patent foramen ovale (PFO), is a risk factor for paradoxical embolism and stroke. Results of studies about brain lesions in diffusion-weighted imaging (DWI) in PFO patients were controversial. DWI only detects acute ischemic lesions. We assessed the hypothesis that, in T2-weighted magnetic resonance imaging (T2WI) of stroke patients, RLS is associated with a typical distribution of small white matter lesions.
Materials and methods
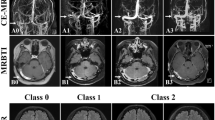
In this retrospective case–control study, T2WI images of 162 stroke patients were evaluated. From stroke patients admitted between 1999 and 2003, 81 stroke patients with RLS were identified with contrast-enhanced transcranial Doppler (bubble test). Controls were 81 age-matched stroke patients without RLS (negative bubble test). In T2WI images, small lesions (<2 cm) were categorized depending on their location in subcortical white matter, peritrigonal white matter, deep and paraventricular white matter, and basal ganglia. Additionally, larger territorial infarcts were rated.
Results
In T2WI frontal or predominantly frontal-located subcortical small white matter, lesions are significantly associated with RLS (p < 0.0001, chi-square test). Forty-three patients with RLS (53%) and only 19 control patients (23%) showed this frontal dominance. Odds ratio is 3.7 (95% confidence interval = 1.9–7.1) for having a RLS when T2WI shows this lesion pattern in a stroke patient. No patient of the RLS group and 6% of the control group had parietal dominance. Distribution of small lesions in other locations like basal ganglia or deep white matter showed no significant difference for the groups.
Conclusion
A distribution of mainly frontal subcortical small white matter lesions in T2WI is significantly associated with RLS in stroke patients.


Similar content being viewed by others
References
Cabanes L, Mas JL, Cohen A et al (1993) Atrial septal aneurysm and patent foramen ovale as risk factors for cryptogenic stroke in patients less than 55 years of age. A study using transesophageal echocardiography. Stroke 24:1865–1873
Mas JL, Arquizan C, Lamy C et al (2001) Patent Foramen Ovale and Atrial Septal Aneurysm Study Group. Recurrent cerebrovascular events associated with patent foramen ovale, atrial septal aneurysm, or both. N Engl J Med 345:1740–46
Di Tullio M, Sacco RL, Gopal A et al (1992) Patent foramen ovale as a risk factor for cryptogenic stroke. Ann Intern Med 117:461–465
De Castro S, Cartoni D, Fiorelli M et al (2000) Morphological and functional characteristics of patent foramen ovale and their embolic implications. Stroke 31:2407–2413
Handke M, Harloff A, Olschewski M et al (2007) Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med 357:2262–2268. doi:10.1056/NEJMoa071422
Jauss M, Wessels T, Trittmacher S et al (2006) Embolic lesion pattern in stroke patients with patent foramen ovale compared with patients lacking an embolic source. Stroke 37:2159–2161. doi:10.1161/01.STR.0000231645.22128.ab
Bonati LH, Kessel-Schaefer A, Linka AZ et al (2006) Diffusion-weighted imaging in stroke attributable to patent foramen ovale: significance of concomitant atrial septum aneurysm. Stroke 37:2030–2034. doi:10.1161/01.STR.0000231655.52686.ab
Santamarina E, González-Alujas MT, Muñoz V et al (2006) Stroke patients with cardiac atrial septal abnormalities: differential infarct patterns on DWI. J Neuroimaging 16:334–340
Prabhakaran S, Wright CB, Yoshita M et al (2008) Prevalence and determinants of subclinical brain infarction: the Northern Manhattan Study. Neurology 70:425–430. doi:10.1212/01.wnl.0000277521.66947.e5
Teague SM, Sharma MK (1991) Detection of paradoxical cerebral echo contrast embolization by transcranial Doppler ultrasound. Stroke 22:740–745
Jauss M, Kaps M, Keberle M et al (1994) A comparison of transesophageal echocardiography and transcranial Doppler sonography with contrast medium for detection of patent foramen ovale. Stroke 25:1265–1267
Jauss M, Zanette E (2000) Detection of right-to-left shunt with ultrasound contrast agent and transcranial Doppler sonography. Cerebrovasc Dis 10:490–496. doi:10.1159/000016119
Bokura H, Kobayashi S, Yamaguchi S (1998) Distinguishing silent lacunar infarction from enlarged Virchow-Robin spaces: a magnetic resonance imaging and pathological study. J Neurol 245:116–122. doi:10.1007/s004150050189
Jung DK, Devuyst G, Maeder P et al (2001) Atrial fibrillation with small subcortical infarcts. J Neurol Neurosurg Psychiatry 70:344–349. doi:10.1136/jnnp.70.3.344
Knipp SC, Matatko N, Schlamann M et al (2005) Small ischemic brain lesions after cardiac valve replacement detected by diffusion-weighted magnetic resonance imaging: relation to neurocognitive function. Eur J Cardiothorac Surg 28:88–96. doi:10.1016/j.ejcts.2005.02.043
de Leeuw FE, de Groot JC, Achten E et al (2001) Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J Neurol Neurosurg Psychiatry 70:9–14. doi:10.1136/jnnp.70.1.9
Vermeer SE, Koudstaal PJ, Oudkerk M et al (2002) Prevalence and risk factors of silent brain infarcts in the population-based Rotterdam Scan Study. Stroke 33:21–25. doi:10.1161/hs0102.101629
Droste DW, Jekentaite R, Stypmann J et al (2002) Contrast transcranial Doppler ultrasound in the detection of right-to-left shunts: comparison of Echovist-200 and Echovist-300, timing of the Valsalva maneuver, and general recommendations for the performance of the test. Cerebrovasc Dis 13:235–241. doi:10.1159/000057849
Droste DW, Kriete JU, Stypmann J et al (1999) Contrast transcranial Doppler ultrasound in the detection of right-to-left shunts: comparison of different procedures and different contrast agents. Stroke 30:1827–1832
Nedeltchev K, Mattle HP (2006) Contrast-enhanced transcranial Doppler ultrasound for diagnosis of patent foramen ovale. Front Neurol Neurosci 21:206–215. doi:10.1159/000092432
Belvís R, Leta RG, Martí-Fàbregas J et al (2006) Almost perfect concordance between simultaneous transcranial Doppler and transesophageal echocardiography in the quantification of right-to-left shunts. J Neuroimaging 16:133–138
Pearson AC, Labovitz AJ, Tatineni S et al (1991) Superiority of transesophageal echocardiography in detecting cardiac source of embolism in patients with cerebral ischemia of uncertain etiology. J Am Coll Cardiol 17:66–72
Strandberg M, Marttila RJ, Helenius H et al (2002) Transoesophageal echocardiography in selecting patients for anticoagulation after ischemic stroke or transient ischemic attack. J Neurol Neurosurg Psychiatry 73:29–33. doi:10.1136/jnnp.73.1.29
Reynolds HR, Tunick PA, Kronzon I (2003) Role of transesophageal echocardiography in the evaluation of patients with stroke. Curr Opin Cardiol 18:340–345. doi:10.1097/00001573-200309000-00003
Kang DW, Chalela JA, Ezzeddine MA et al (2003) Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 60:1730–1734. doi:10.1001/archneur.60.12.1730
Vermeer SE, Hollander M, van Dijk EJ et al (2003) Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke 34:1126–1129. doi:10.1161/01.STR.0000068408.82115.D2
Vermeer SE, Prins ND, den Heijer T et al (2003) Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med 348:1215–1222. doi:10.1056/NEJMoa022066
Giele JL, Witkamp TD, Mali WP et al (2004) Silent brain infarcts in patients with manifest vascular disease. Stroke 35:742–746. doi:10.1161/01.STR.0000117572.56058.2A
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, JR., Plötz, BM., Rohr, A. et al. Association of right-to-left shunt with frontal white matter lesions in T2-weighted MR imaging of stroke patients. Neuroradiology 51, 299–304 (2009). https://doi.org/10.1007/s00234-009-0496-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-009-0496-9