Abstract
Introduction and hypothesis
The objective of this study was to validate the Pelvic Floor Distress Inventory (PFDI-20) and Pelvic Floor Impact Questionnaire (PFIQ-7) in Dutch women.
Methods
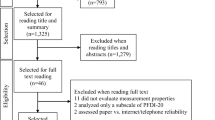
Patients with pelvic floor dysfunction completed the Dutch questionnaires at (1) inclusion to evaluate internal consistency, (2) 1 week later to assess test-retest reliability, and (3) 6 months later to assess responsiveness and interpretability of change. To assess validity, floor and ceiling effects and construct validity were tested. A population-based sample (reference group) completed the questionnaires once.
Results
Data of 111 patients and 283 reference group participants were analyzed. Internal consistency of baseline scores in patient and reference groups was moderate (Cronbach’s alpha 0.52–0.60) to adequate in the PFDI-20 (Cronbach’s alpha 0.71–0.84) and adequate in the PFIQ-7 (Cronbach’s alpha 0.88–0.94). Both measures presented adequate test-retest reliability (intraclass correlation coefficient 0.79–0.91) and adequate responsiveness (area under the receiver-operating characteristic curve both 0.77). Interpretability was adequate for PFDI-20 and acceptable for PFIQ-7 with a clinically relevant minimally important change of −23 and −29 points, respectively. At baseline, the scales of the PFIQ-7 showed floor effects (44–55 %) in patients, though the PFIQ-7 summary score did not. No ceiling effects were observed. Construct validity was adequate with all predefined hypotheses confirmed regarding subgroup discrimination using pooled patient and reference group baseline data.
Conclusions
For assessing distress and health-related quality of life of pelvic floor dysfunction, the Dutch PFDI-20 and PFIQ-7 are reliable and valid in the general Dutch population, and also responsive and interpretable among tertiary care-seeking women.


Similar content being viewed by others
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26. doi:10.1007/s00192-009-0976-9
Barber MD (2007) Questionnaires for women with pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 18(4):461–465. doi:10.1007/s00192-006-0252-1
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC (2001) Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 185(6):1388–1395. doi:10.1067/mob.2001.118659
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–113. doi:10.1016/j.ajog.2004.12.025
Barber MD, Chen Z, Lukacz E, Markland A, Wai C, Brubaker L, Nygaard I, Weidner A, Janz NK, Spino C (2011) Further validation of the short form versions of the Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ). Neurourol Urodyn 30(4):541–546. doi:10.1002/nau.20934
de Tayrac R, Deval B, Fernandez H, Marès P, Mapi Research Institute (2007) [Development of a linguistically validated French version of two short-form, condition-specific quality of life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7)] Validation linguistique en francais des versions courtes des questionnaires de symptomes (PFDI-20) et de qualite de vie (PFIQ-7) chez les patientes presentant un trouble de la statique pelvienne. J Gynecol Obstet Biol Reprod (Paris) 36(8):738–748. doi:10.1016/j.jgyn.2007.08.002
El-Azab AS, Abd-Elsayed AA, Imam HM (2009) Patient reported and anatomical outcomes after surgery for pelvic organ prolapse. Neurourol Urodyn 28(3):219–224. doi:10.1002/nau.20626
Kaplan PB, Sut N, Sut HK (2012) Validation, cultural adaptation and responsiveness of two pelvic-floor-specific quality-of-life questionnaires, PFDI-20 and PFIQ-7, in a Turkish population. Eur J Obstet Gynecol Reprod Biol 162(2):229–233. doi:10.1016/j.ejogrb.2012.03.004
Lowenstein L, Levy G, Chen KO, Ginath S, Condrea A, Padoa A (2012) Validation of Hebrew versions of the Pelvic Floor Distress Inventory, Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire, and the Urgency, Severity and Impact Questionnaire. Female Pelvic Med Reconstr Surg 18(6):329–331. doi:10.1097/SPV.0b013e31827268fa
Teleman P, Stenzelius K, Iorizzo L, Jakobsson U (2011) Validation of the Swedish short forms of the Pelvic Floor Impact Questionnaire (PFIQ-7), Pelvic Floor Distress Inventory (PFDI-20) and Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Acta Obstet Gynecol Scand 90(5):483–487. doi:10.1111/j.1600-0412.2011.01085.x
Toprak Celenay S, Akbayrak T, Kaya S, Ekici G, Beksac S (2012) Validity and reliability of the Turkish version of the Pelvic Floor Distress Inventory-20. Int Urogynecol J 23(8):1123–1127. doi:10.1007/s00192-012-1729-8
Treszezamsky AD, Karp D, Dick-Biascoechea M, Ehsani N, Dancz C, Montoya TI, Olivera CK, Smith AL, Cardenas R, Fashokun T, Bradley CS, Society of Gynecologic Surgeons Fellows’ Pelvic Research Network (2013) Spanish translation and validation of four short pelvic floor disorders questionnaires. Int Urogynecol J 24(4):655–670. doi:10.1007/s00192-012-1894-9
Yoshida M, Murayama R, Ota E, Nakata M, Kozuma S, Homma Y (2013) Reliability and validity of the Japanese version of the pelvic floor distress inventory-short form 20. Int Urogynecol J 24(6):1039–1046. doi:10.1007/s00192-012-1962-1
Zhu L, Yu S, Xu T, Yang X, Lu Y, Li B, Lang J (2011) Chinese validation of the Pelvic Floor Impact Questionnaire Short Form. Menopause 18(9):1030–1033. doi:10.1097/gme.0b013e31820fbcbe
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC (2010) The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 63(7):737–745. doi:10.1016/j.jclinepi.2010.02.006
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012
Guillemin F, Bombardier C, Beaton D (1993) Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 46(12):1417–1432
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A, Standardisation Sub-committee of the International Continence Society (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21(2):167–178. doi:10.1002/nau.10052
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, Cottenden A, Davila W, de Ridder D, Dmochowski R, Drake M, Dubeau C, Fry C, Hanno P, Smith JH, Herschorn S, Hosker G, Kelleher C, Koelbl H, Khoury S, Madoff R, Milsom I, Moore K, Newman D, Nitti V, Norton C, Nygaard I, Payne C, Smith A, Staskin D, Tekgul S, Thuroff J, Tubaro A, Vodusek D, Wein A, Wyndaele JJ, Members of Committees, Fourth International Consultation on Incontinence (2010) Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 29(1):213–240. doi:10.1002/nau.20870
Hays RD, Sherbourne CD, Mazel RM (1993) The RAND 36-Item Health Survey 1.0. Health Econ 2(3):217–227
Zee vdK, Sanderman R Het meten van de algemene gezondheidstoestand met de RAND-36. Een handleiding. NCG reeks meetinstrumenten. Groningen
Flycatcher Academic Support Centre. http://www.flycatcher.eu/nld/academic-support/. 2012
de Vet HCW, Terwee CB, Mokkink LB, Knol DL (2011) Measurement in medicine. Practical guides to biostatistics and epidemiology, 1st edn. Cambridge University Press, Cambridge
McGraw K, Wong S (1996) Forming inferences about some intraclass correlation coefficients. Psychol Methods 1(1):30–46
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Korfage IJ, Hak T, de Koning HJ, Essink-Bot ML (2006) Patients’ perceptions of the side-effects of prostate cancer treatment–a qualitative interview study. Soc Sci Med 63(4):911–919. doi:10.1016/j.socscimed.2006.01.027
Milsom I (2009) Epidemiology of urinary and faecal incontinence and pelvic organ prolapse. In: Abrams P, Cardozo L, Khoury S, Wein A (eds) 4th International Consultation on Incontinence, 4th edn. Health Publication, Paris
van der Vaart CH, de Leeuw JR, Roovers JP, Heintz AP (2000) [The influence of urinary incontinence on quality of life of community-dwelling, 45–70 year old Dutch women] De invloed van urine-incontinentie op de kwaliteit van leven bij thuiswonende Nederlandse vrouwen van 45–70 jaar. Ned Tijdschr Geneeskd 144(19):894–897
Pretlove SJ, Radley S, Toozs-Hobson PM, Thompson PJ, Coomarasamy A, Khan KS (2006) Prevalence of anal incontinence according to age and gender: a systematic review and meta-regression analysis. Int Urogynecol J Pelvic Floor Dysfunct 17(4):407–417. doi:10.1007/s00192-005-0014-5
Acknowledgments
Part of this study was funded by the Urological Research Foundation [Stichting Urologisch Wetenschappelijk Onderzoek (SUWO), Rotterdam, the Netherlands]. SUWO was not involved in the design, conduct, interpretation, and analysis of the study or review or approval of the manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix




Rights and permissions
About this article
Cite this article
Utomo, E., Blok, B.F., Steensma, A.B. et al. Validation of the Pelvic Floor Distress Inventory (PFDI-20) and Pelvic Floor Impact Questionnaire (PFIQ-7) in a Dutch population. Int Urogynecol J 25, 531–544 (2014). https://doi.org/10.1007/s00192-013-2263-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2263-z