Abstract
Background
It is unknown whether a volume–outcome relationship exists for mechanically ventilated admissions to UK critical care units. This study was conducted to evaluate the volume–outcome relationship for mechanically ventilated admissions to adult, general critical care units in the UK with a view to informing policy, service delivery and organisation of specialist, advanced respiratory care.
Methods
A retrospective cohort study using data from the Case Mix Programme Database was conducted. The primary exposure of interest was annual volume (absolute number) of mechanically ventilated admissions per critical care unit per year. The primary outcome was ultimate acute hospital mortality. A multivariable analysis was performed to assess the relationship between annual volume and outcome while adjusting for a priori selected confounders. Two interaction tests were performed. The first interaction test was between annual volume and admission type and the second between annual volume and initial acute severity of respiratory failure. Sensitivity analysis excluding volume outlier units and using restricted cubic splines to model volume was also performed.
Results
After adjusting for confounding, there was a significant relationship between annual volume and ultimate acute hospital mortality (p < 0.02). The first interaction test revealed a strong interaction between annual volume and admission type, with a more pronounced volume–outcome relationship for non-surgical admissions (p < 0.001). The second interaction test between annual volume and initial acute severity of respiratory failure was not statistically significant (p = 0.12). The analysis using restricted cubic splines demonstrated a similar graphical relationship but the results were not statistically significant (p = 0.87).
Conclusions
A volume–outcome relationship was demonstrated for mechanically ventilated admissions to adult, general critical care units in the UK. The relationship is sensitive to the modelling approach used.
Similar content being viewed by others
Introduction
It has been proposed that critically ill adult patients requiring advanced respiratory support be triaged according to severity of illness, case complexity and therapeutic need and the most severe cases be transferred to higher volume, specialist respiratory centres to receive advanced respiratory support [1]. The potential advantages of such centralised care are twofold: first, health care funds can be contained if they are focused on selective, specialised centres; and second, health outcomes may be improved by treatment in higher volume centres. Such centralisation of care has already occurred in the UK for other critically ill patient groups, including trauma, neonatal and paediatric patients [2–4].
The trend towards centralised care is, in large part, based on the body of research evidence evaluating the relationship between volume of cases treated and patient outcomes, both outside and within critical care. A strong volume–outcome association has been demonstrated for complex surgical procedures and for certain medical conditions [5]. Studies in critical care have generally shown an important volume–outcome relationship, with the strongest evidence found for mechanically ventilated admissions [6–8]. However, three previous studies conducted in the UK, including one for mechanically ventilated admissions, were underdeveloped and as such, sufficient evidence for a volume–outcome relationship in mechanically ventilated admissions is lacking [9–11].
Given the complexity of care involved in treating admissions with severe respiratory failure and the recent trend to centralise care for such admissions, this study was carried out to further evaluate the volume–outcome relationship, using a large, representative high quality critical care database, for mechanically ventilated admissions to adult, general critical care units in the UK. The study was performed with a view to informing policy, service delivery and organisation of specialist, advanced respiratory care.
Materials and methods
Study design
A secondary analysis of the Case Mix Programme Database (CMPD) was conducted. The CMPD contains pooled case mix and outcome data on consecutive admissions to adult, general (mixed medical/surgical) critical care units (i.e. both stand-alone intensive care and combined intensive care/high dependency units) in England, Wales and Northern Ireland. Raw physiological and diagnostic data, required for the APACHE II and Intensive Care National Audit and Research Centre (ICNARC) risk prediction models, together with demographic, outcome and activity data are collected as part of the national clinical audit (the Case Mix Programme) coordinated by the ICNARC. These data are collected prospectively and abstracted retrospectively by trained data collectors. Data undergo extensive validation, both locally and centrally, before being pooled in the central CMPD. Details of data collection and validation have been reported previously [12] and the CMPD has been independently assessed to be of high quality [13]. ICNARC has approval for the CMPD under Section 251 of the National Health Service (NHS) Act 2006 (Approval Number PIAG 2-10(f)/2005).
Patient selection
Data were extracted for the years 2008–2010. Admissions, aged 16 years or older, who were mechanically ventilated at any point during the first 24 h following admission to a critical care unit, were selected.
Units with less than 6 months of data for the years 2008–2010 were excluded. Admissions transferred either directly into a unit from another critical care unit or transferred out (within 24 h) directly to another critical care unit were excluded to avoid confounding results with outcomes from other units. In addition, subsequent readmissions of the same patient to the same critical care unit during the same acute hospital stay were also excluded to ensure outcomes were independent.
Exposure, outcome and confounding variables
The primary exposure of interest was annual volume (absolute number) of mechanically ventilated admissions per critical care unit per year. Admissions were deemed to be mechanically ventilated where ventilation was delivered by any mode of conventional ventilation (also including bi-level positive airway pressure ventilation, high frequency and jet ventilation, negative pressure ventilation and bag and mask ventilation) and identified prospectively by a trained data collector by the recording of a ventilated respiratory rate. For critical care units contributing less than 1 year of data (but at least 6 months in the years 2008–2010; see above), annual volume was extrapolated from available data. All mechanically ventilated admissions, excluding units with less than 6 months of data, were included in the calculation of annual volume.
The primary outcome was ultimate acute hospital mortality defined as death before final discharge from an acute hospital and included deaths after direct transfer to another acute hospital from the acute hospital housing the critical care unit.
For critical care admissions, data were available on age, sex, ethnicity, acute severity of illness, medical history, admission type, location prior to admission and length of stay. Ethnicity was categorised as white or non-white. Acute severity of illness was measured using the ICNARC physiology score from the ICNARC model [14] and the APACHE II score [15]. Medical history was defined by severe co-morbidities, defined by the APACHE II method (severe cardiovascular disease, severe respiratory disease, chronic renal disease, chronic liver disease, haematological malignancy, metastatic disease, immunological dysfunction), in the 6 months prior to admission; by activities of daily living in the 6 months prior to admission; and by receipt of cardiopulmonary resuscitation (CPR) in the 24 h prior to admission. Admission type was categorised into surgical and non-surgical admissions. A surgical admission was defined as any direct admission to the critical care unit from the operating theatre. All other admissions were considered non-surgical. Location prior to admission to the critical care unit was categorised as operating theatre (subdivided by urgency of surgery into emergency/urgent or elective/scheduled), hospital ward, high dependency unit or emergency department. Length of stay was divided into critical care unit and acute hospital stay where acute hospital stay included continuous stay in acute hospital, even if transferred from one to another acute hospital. Finally, hospital type was defined by the hospital’s university status.
Statistical analysis
An analysis of baseline characteristics was performed for the whole cohort and by annual volume, grouped by quartiles of critical care units. A univariable analysis was conducted to assess the relationship between variables of interest and ultimate acute hospital mortality. A multivariable analysis was performed to assess the relationship between annual volume (of mechanically ventilated admissions) and outcome (ultimate acute hospital mortality) while adjusting for a priori selected confounders (age, sex, ICNARC physiology score, severe comorbidities, activities of daily living, prior CPR, location prior to admission and hospital type). All variables were entered into the model simultaneously with no statistical selection process applied. A logistic regression model was fitted with generalised estimating equations and robust standard errors to adjust for clustering of outcome at the critical care unit level. Hypothesis tests were carried out using Wald and likelihood ratio tests. Multivariable fractional polynomial modelling (degree 2) was used to select the best functional form for continuous factors (annual volume, age and ICNARC physiology score).
In order to further explore the volume–outcome relationship for mechanically ventilated admissions, two interaction tests were performed. The first, between annual volume and admission type, was conducted to test the hypothesis that mechanically ventilated medical admissions, which were potentially sicker and more likely to have pulmonary pathology, would derive greater benefit from being treated in higher volume units. The second, between annual volume and PaO2/FiO2 ratio, was conducted to test the hypothesis that patients with initial acute severe respiratory failure would benefit more from being treated in higher volume units. We used the “MPFIgen” procedure to explore interactions with continuous variables [16]. Briefly, we constructed multiplicative interaction terms between the fractional polynomial transformations selected in the main model without interactions. The model was then refitted with the interaction terms added and all interaction terms jointly tested using a Wald test.
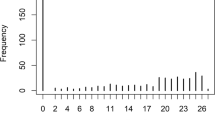
A sensitivity analysis was performed to assess the relationship between annual volume of mechanically ventilated admissions and ultimate acute hospital mortality using multivariable regression analysis excluding outlier units with respect to annual volume. Two critical care units with annual volumes of mechanically ventilated admissions exceeding 750 were excluded. A further analysis was also performed modelling volume with restricted cubic spline regression models using five knots.
Statistical analyses were performed using Stata Version 10.1 (StataCorp LP, College Station TX, USA).
Results
Of 279,315 admissions to 200 adult, general critical care units from 1 January 2008 to 31 December 2010, 122,341 (43.8 %) were mechanically ventilated during the first 24 h following admission to the unit (Fig. 1). After excluding seven units with less than 6 months of data for the time period studied [698 (0.6 %) admissions] and 1,350 admissions (1.1 %) aged less than 16 years, 120,293 mechanically ventilated admissions to 193 adult, general critical care units were used to calculate the annual volume (number) of mechanically ventilated admissions per unit per year. After excluding admissions directly transferred into the unit from another critical care unit (10,549, 8.8 %), directly transferred out of the unit to another critical care unit within 24 h (1,616, 1.3 %) and subsequently readmitted to the critical care unit during the same acute hospital stay (3,284, 2.7 %), 104,844 mechanically ventilated admissions to 193 adult, general critical care units were included in the final analysis.
For descriptive purposes, the cohort was grouped by quartiles of critical care units. The median number of mechanically ventilated admissions in the lowest quartile was 141 and rose to 480 in the highest quartile (Electronic Supplementary Material, Table 1). Over half the cohort was male and admissions were predominantly white (Table 1). The median APACHE II score was 17 and 15 % of admissions had one or more severe comorbidities. Roughly one-third of patients were admitted directly from the operating theatre with two-thirds of these following emergency/urgent procedures. Over 98 % of all admissions that were ventilated were invasively ventilated with no difference across volume quartiles. The median number of days in the critical care unit was 3 and the median number of days spent in acute hospital was 13. Critical care unit mortality was 27.7 % and ultimate acute hospital mortality was 36.7 %.
When grouped into quartiles of critical care units, a few notable differences in the admissions’ baseline characteristics were observed (Table 1). Admissions in the higher volume quartile had higher rates of severe comorbidities, with increased chronic renal and chronic liver disease but a lower incidence of prior CPR. In addition, they were more likely to be admitted directly following a surgical procedure, for both emergency/urgent and elective/scheduled procedures. The higher volume quartile units were also more likely to be in university or university-affiliated hospitals. Unadjusted, critical care unit and ultimate acute hospital mortality were lowest in the higher volume quartile.
After adjusting for confounding, there was a significant relationship between annual volume and ultimate acute hospital mortality with a higher volume of mechanically ventilated admissions associated with lower mortality (Fig. 2, p < 0.02). There was an increase in ultimate acute hospital mortality in units with the highest volume.
Relationship between annual volume of mechanically ventilated admissions and ultimate acute hospital mortality. Volume modelled using fractional polynomials (degree 2) relative to mean volume of 332 admissions per year. Model adjusted for age (fractional polynomials degree 2), sex, ICNARC physiology score (fractional polynomials degree 2), comorbidities, activities of daily living, CPR prior to admission, location prior to admission and hospital type. The dashed lines represent 95 % confidence intervals
The first interaction test revealed a strong interaction between annual volume and admission type, with a more pronounced volume–outcome relationship for non-surgical admissions (p < 0.001) (Electronic Supplementary Material, Fig. 1). The second interaction test, however, indicated no significant interaction between annual volume and initial PaO2/FiO2 ratio suggesting the volume–outcome relationship is not stronger for admissions with higher initial acute severe respiratory failure (p = 0.12) (Electronic Supplementary Material, Fig. 2).
The sensitivity analysis examining the relationship between annual volume and ultimate acute hospital mortality, with exclusion of the two highest volume outlying critical care units, revealed a statistically significant result with a more linear volume–outcome relationship (Fig. 3). Examination of these two outlier units revealed that one differed from the rest in the higher volume quartile (Electronic Supplementary Material, Table 1). Admissions to this unit were younger with lower severity of illness scores and less severe comorbidities and fewer surgical admissions.
Relationship between annual volume of mechanically ventilated admissions and ultimate acute hospital mortality after excluding outlier critical care units. Volume modelled using fractional polynomials (degree 2) relative to mean volume of 321 admissions per year. Model adjusted for age (fractional polynomials degree 2), sex, ICNARC physiology score (fractional polynomials degree 2), comorbidities, activities of daily living, CPR prior to admission, location prior to admission and hospital type. The dashed lines represent 95 % confidence intervals
Similarly, for the two interaction tests, the sensitivity analysis excluding the two highest volume outlying critical care units demonstrated a strong interaction for non-surgical admissions and no significant interaction with PaO2/FiO2 ratio (Electronic Supplementary Material, Figs. 3, 4).
The analysis was also performed using restricted cubic splines, instead of fractional polynomials, and revealed a similar graphical relationship between annual volume of mechanically ventilated admissions and ultimate acute hospital mortality but the results using restricted cubic splines were not statistically significant (p = 0.87) (Electronic Supplementary Material, Figs. 5, 6). When the two highest volume outlying critical care units were excluded, the relationship remained non-significant.
Discussion
The results of this study demonstrate a significant volume–outcome relationship for mechanically ventilated admissions to adult, general critical care units in the UK with a stronger interaction for non-surgical admissions. However, the results did vary depending on the modelling strategy used. These results tend to support the recent policy proposal from the UK Department of Health expert group to centralise service delivery and organisation of specialist, advanced respiratory care for admissions with the most severe respiratory failure [1].
The strengths of this study are worth noting. First, this study is the largest and most representative, both in terms of number of admissions and the number of critical care units included in the analysis. Second, adjustment for confounding was performed using a previously validated risk model developed and calibrated specifically for UK critical care. The main limitation of this study relates to all non-randomised comparisons, namely the potential for unmeasured confounding. However, given the detailed data collected, validated and pooled in the CMPD and the sophistication of the adjustment for confounding conducted, it is anticipated that the impact of any residual confounding should be minimal.
The existing international literature on the volume–outcome relationship for mechanically ventilated admissions to critical care is conflicting—only four of the nine previous studies demonstrate a relationship [6, 7, 17, 18] with the remaining five demonstrating no relationship [11, 19–22]. One of the negative studies employed an administrative database and may have failed to sufficiently adjust for confounders, particularly acute severity of illness, whereas the three other negative studies undertook detailed risk adjustment, employing validated risk models and employed statistical techniques to account for clustering of admissions. Of these, the study by Gopal et al. was conducted in the UK and the lack of demonstration of a volume–outcome relationship may be explained by the small sample size (units and patients) and regional location. The two other negative studies with detailed risk adjustment were conducted outside the UK and international differences in health care may partially explain the discrepant results [23–25]. Furthermore, one of these, the study by Cooke et al., had a small variation in volume range across units and a small sample size and may not, therefore, have been adequately powered to detect a volume–outcome relationship. Similarly, the study by Fernandez et al. [22] had a small number of critical care unit admissions and was likely underpowered.
There are several possible explanations for the volume–outcome relationship that was observed for mechanically ventilated admissions to UK critical care units in our study. First, higher volume centres may just have more experience dealing with complex pulmonary cases and in delivering mechanical ventilation. Second, higher volume centres may have access to newer ventilator technologies. Third, higher volume centres may adhere more to effective therapeutic standards such as low tidal volume ventilation and conservative fluid therapy [26, 27]. Fourth, higher volume centres may have greater resources permitting higher staffing levels, higher nurse to patient ratios, larger multidisciplinary teams and/or intensivist-led staffing models [28–30]. Finally, the relationship observed may be related to a combination of some or all of these.
The volume–outcome relationship demonstrated in this study, yet not shown in a previously published study using the same database but evaluating the relationship for admissions with severe sepsis to UK critical care units [9], reveals the heterogeneity of the volume–outcome relationship for different technologies and in different critically ill patient groups. It is possible that a volume–outcome relationship will be more likely to be apparent when involving the more technical aspects of care, such as using a mechanical ventilator or performing a surgical procedure.
The volume–outcome relationship observed in the subgroup of non-surgical admissions suggests that more complex admissions may benefit more from treatment in higher volume centres. The group of surgical admissions was intermixed with admissions following elective/scheduled procedures that may only require routine, short-term mechanical ventilation and would unlikely derive extra benefit from treatment in a higher volume centre. Although it is surprising that admissions with lower PaO2/FiO2 ratios did not demonstrate a stronger volume–outcome relationship, this is most likely explained by the availability of only one P/F ratio value from the first 24 h and would, therefore, likely include those with a transient low value as well as those with sustained low P/F ratios over time. Additionally, this result may be further explained by lack of statistical power.
Of note, the volume–outcome relationship was sensitive to the modelling strategy used. Using restricted cubic splines the volume–outcome relationship was non-significant despite a similar graphical relationship to the fractional polynomial modelling strategy. This suggests that caution is needed when interpreting results from volume outcome studies as there may be differences depending on the modelling strategy employed. It is unclear as to why this difference would occur but it may be related to type II error.
Future research will be needed to examine possible ramifications of centralised care on admissions with severe respiratory failure. One concern is the potential for harm incurred from transportation of critically ill admissions to the designated centralised unit. A second concern is the effect of centralisation on the relationship between families, patients and their health-care team. As patients are transported away from their local acute hospital, they may lose the benefit of the relationship that they have with their original health-care team [31]. Both of these issues may lead to increased strain and impact on families’ and patients’ satisfaction with care? (The families and patients are not doing the caring!).
Conclusion
A volume–outcome relationship was demonstrated for mechanically ventilated admissions to adult, general critical care units in the UK. The relationship is sensitive to the modelling approach used. Care should be taken when applying these results to other countries or health-care systems as international differences in critical care unit provision, structure and organisation exist and may limit the generalisability of our findings [23, 24].
References
UK Expert Group (2010) Management of severe refractory hypoxia in critical care in the UK in 2010. Report commissioned by the UK Department of Health, London
Tilford JM, Simpson PM, Green JW, Lensing S, Fiser DH (2000) Volume-outcome relationships in pediatric intensive care units. Pediatrics 106:289–294
Ramnarayan P, Thiru K, Parslow RC, Harrison DA, Draper ES, Rowan KM (2010) Effect of specialist retrieval teams on outcomes in children admitted to paediatric intensive care units in England and wales: a retrospective cohort study. Lancet 376:698–704
London Trauma Office (2010) London trauma system. http://www.Londontraumaoffice.nhs.uk/londons-trauma-system/about-the-london-trauma-system/. Accessed 30 Jan 2014
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137:511–520
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD (2006) Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 355:41–50
Darmon M, Azoulay E, Fulgencio JP, Garrigues B, Gouzes C, Moine P et al (2011) Procedure volume is one determinant of centre effect in mechanically ventilated patients. Eur Respir J 37:364–370
Kahn JM (2013) What’s new in ICU volume-outcome relationships? Intensive Care Med 39:1635–1637
Shahin J, Harrison DA, Rowan KM (2012) Relation between volume and outcome for patients with severe sepsis in United Kingdom: retrospective cohort study. BMJ 344:e3394
Jones J, Rowan K (1995) Is there a relationship between the volume of work carried out in intensive care and its outcome? Int J Technol Assess Health Care 11:762–769
Gopal S, O’Brien R, Pooni J (2011) The relationship between hospital volume and mortality following mechanical ventilation in the intensive care unit. Minerva Anestesiol 77:26–32
Harrison DA, Brady AR, Rowan K (2004) Case mix, outcome and length of stay for admissions to adult, general critical care units in England, Wales and Northern Ireland: the Intensive Care National Audit and Research Centre Case Mix Programme Database. Crit Care 8:R99–111
Harrison DA, Rowan KM (2008) Outcome prediction in critical care: the ICNARC model. Curr Opin Crit Care 14:506–512
Harrison DA, Parry GJ, Carpenter JR, Short A, Rowan K (2007) A new risk prediction model for critical care: the Intensive Care National Audit and Research Centre (ICNARC) model. Crit Care Med 35:1091–1098
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Royston P, Sauerbrei W (2008) Multivariable model-building: a pragmatic approach to regression analysis based on fractional polynomials for modelling continuos variables. Wiley, New York
Kahn JM, Ten Have TR, Iwashyna TJ (2009) The relationship between hospital volume and mortality in mechanical ventilation: an instrumental variable analysis. Health Serv Res 44:862–879
Dres M, Tran TC, Aeqerter P, Rabbat A, Guidet B, Huchon G et al (2013) Influence of ICU case-volume on the management and hospital outcomes of acute exacerbations of chronic obstructive pulmonary disease. Crit Care Med 2013(41):1884–1892. doi:10.1097/CCM.0b013e31828a2bd8
Needham DM, Bronskill SE, Rothwell DM, Sibbald WJ, Pronovost PJ, Laupacis A et al (2006) Hospital volume and mortality for mechanical ventilation of medical and surgical patients: a population-based analysis using administrative data. Crit Care Med 34:2349–2354
Moran JL, Solomon PJ (2012) Mortality and intensive care volume in ventilated patients from 1995 to 2009 in the Australian and New Zealand binational adult patient intensive care database. Crit Care Med 40:800–812
Cooke CR, Kennedy EH, Wiitala WL, Almenoff PL, Sales AE, Iwashyna TJ (2012) Despite variation in volume, veterans affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit Care Med 40:2569–2575
Fernandez R, Altaba S, Cabre L, Lacueva V, Santos A, Solsona JF, Anon JM, Catalan RM et al (2013) Relationship between volume and survival in closed intensive care units is weak and apparent only in mechanically ventilated patients. Anesthesiology 119:871–879
Wunsch H, Angus DC, Harrison DA, Collange O, Fowler R, Hoste EA et al (2008) Variation in critical care services across North America and Western Europe. Crit Care Med 36(2787–2793):e2781–e2789
Wunsch H, Rowan KM, Angus DC (2007) International comparisons in critical care: a necessity and challenge. Curr Opin Crit Care 13:725–731
Urbach DR, Croxford R, MacCallum NL, Stukel TA (2005) How are volume-outcome associations related to models of health care funding and delivery? A comparison of the United States and Canada. World J Surg 29:1230–1233
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, de Boisblanc B et al (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A et al (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL (2002) Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 288:2151–2162
Kane SL, Weber RJ, Dasta JF (2003) The impact of critical care pharmacists on enhancing patient outcomes. Intensive Care Med 29:691–698
Curtis JR, Cook DJ, Wall RJ, Angus DC, Bion J, Kacmarek R et al (2006) Intensive care unit quality improvement: a “how-to” guide for the interdisciplinary team. Crit Care Med 34:211–218
Kahn JM, Branas CC, Schwab CW, Asch DA (2008) Regionalization of medical critical care: what can we learn from the trauma experience? Crit Care Med 36:3085–3088
Acknowledgments
This work was supported by internal funding from the Intensive Care National Audit & Research Centre.
Conflicts of interest
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted in the previous 3 years; no other relationship or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: A volume–outcome relationship was demonstrated for mechanically ventilated admissions to adult, general critical care units in the UK.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shahin, J., Harrison, D.A. & Rowan, K.M. Is the volume of mechanically ventilated admissions to UK critical care units associated with improved outcomes?. Intensive Care Med 40, 353–360 (2014). https://doi.org/10.1007/s00134-013-3205-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3205-4