Abstract
Aims/hypothesis
The rising prevalence of diabetes worldwide has increased interest in the cost of diabetes. Inpatient costs for all people with diabetes in Scotland were investigated.
Methods
The Scottish Care Information—Diabetes Collaboration (SCI-DC), a real-time clinical information system of almost all diagnosed cases of diabetes in Scotland, UK, was linked to data on all hospital admissions for people with diabetes. Inpatient stay costs were estimated using the 2007–2008 Scottish National Tariff. The probability of hospital admission and total annual cost of admissions were estimated in relation to age, sex, type of diabetes, history of vascular admission, HbA1c, creatinine, body mass index and diabetes duration.
Results
In Scotland during 2005–2007, 24,750 people with type 1 and 195,433 people with type 2 diabetes were identified, accounting for approximately 4.3% of the total Scottish population (5.1 million). The estimated total annual cost of admissions for all people diagnosed with type 1 and type 2 diabetes was £26 million and £275 million, respectively, approximately 12% of the total Scottish inpatient expenditure (£2.4 billion). Sex, increasing age, serum creatinine, previous vascular history and HbA1c (the latter differentially in type 1 and type 2) were all associated with likelihood and total annual cost of admission.
Conclusions/interpretation
Diabetes inpatient expenditure accounted for 12% of the total Scottish inpatient expenditure, whilst people with diabetes account for 4.3% of the population. Of the modifiable risk factors, HbA1c was the most important driver of cost in type 1 diabetes.
Similar content being viewed by others
Introduction
The rising prevalence of diabetes worldwide has increased interest in the costs of diabetes in total and relative to the rest of the population. Estimates of the proportion of total healthcare expenditure spent on people with diabetes have varied widely ranging between 3% and 4% (for type 2 diabetes in eight European countries [1] or Ireland [2]) and 20% (for all people with diabetes) in the USA [3]. Estimates will vary depending on the accuracy of the methods used, success in identifying people with diabetes and costs, population prevalence of diabetes (which ranges between 3% and 5.8% in these studies) and underlying healthcare costs. Most recently it was estimated that people with diabetes in Wales accounted for 12.3% of the total acute hospital expenditure, with diabetes prevalence of 3.5% [4].
In studies of total costs, hospitalisations accounted for approximately half of the costs [1–3]. Drug therapies, ambulatory, outpatient and primary care accounted for the remainder.
In Scotland almost all people with diabetes are included in a national clinical information system (described at www.diabetesinscotland.org.uk). The register is populated by data from all hospital clinics for adults, the nationwide retinopathy screening service and all except five of the approximately 1,000 primary care practices in Scotland. Data on all hospital admissions are collated centrally. Data linkage allows assessment of the national inpatient costs for people with diabetes at the population level along with assessment of factors associated with these costs.
Very few studies have examined the total cost of diabetes [5] and there is a need for accurate and up-to-date estimates. The total inpatient costs of people with diabetes in Scotland were examined. The effects of characteristics such as age, sex, diabetes duration and HbA1c on admission to hospital and cost of admission were investigated to suggest which factors could be focused on to reduce admission and to assist in health services planning.
Methods
Data
The Scottish Care Information—Diabetes Collaboration (SCI-DC) is a dynamic national register of people with diagnosed diabetes in Scotland. SCI-DC contains records for almost all people with a diagnosis of diabetes in Scotland [6], containing detailed clinical information such as BMI, creatinine, age, sex, and HbA1c. Patients were identified by a unique identifier, the Community Health Index (CHI), to allow record linkage to routinely collected datasets.
Data obtained from SCI-DC in November 2009 were linked to Scottish Morbidity Records (SMR-01), the centralised data on hospital admissions collated by Information Services Division (ISD) of National Health Services Scotland (www.isdscotland.org). SMR-01 records contain over 95% of Scotland’s hospital admissions and include information on demographic factors, date and length of admission, and date of discharge. Individual episodes of care are recorded within each admission with up to six International Classification of Disease (ICD) diagnosis codes (1981–1997: ICD-9 [www.icd9data.com/2007/Volume1/240-279/250-259/250/default.htm]; 1997–present: ICD-10 [www.who.int/classifications/icd/en/]). During one admission a patient may have more than one episode of care, for example intensive care unit followed by general medical ward. The SMR-01 and SCI-DC data were linked to General Register Office for Scotland (GROS) death records which provide information on cause and date of death. The linked dataset provides a complete, population-wide picture of morbidity from 1981.
Individuals were excluded from the analysis where there were inconsistencies in date of birth or sex (2,993 people), no date of diagnosis (1,484 people), or no clinical or hospital admission data existed for the years 2005–2007 (3,317 people). Only people with type 1 or type 2 diabetes were included.
Estimation of direct formal costs
The Scottish National Tariff project [7], established in 2005, is a collaborative project between ISD and the Scottish Government Health Directorate. The aim of the Scottish National Tariff is to estimate standard prices for procedures. The Scottish National Tariff uses both the Scottish Costs Book [8] which provides costs of care at a specialty level, and a weighted version of the English NHS reference costs [9], which provides costs at the Healthcare Resource Groups (HRG) level. The HRGs are standard groupings of clinically similar treatments which use common levels of healthcare resource and are currently used as a means of determining fair and equitable reimbursement for care services delivered by providers [10]. Each episode of care is associated with one HRG code, generated using the HRG Grouper v3.5 and matched to the 2007–2008 Scottish National Tariff to generate a cost per episode. For admissions with single episodes of care, the cost for this admission is simply the HRG cost provided by the Scottish National Tariff; for admissions with multiple episodes, the most expensive episode is used as the cost for that admission to avoid double counting. Average costs for the non-diabetic population (by age and sex) were also obtained from the Scottish National Tariff team, with the exclusion of information on all those defined as having diabetes on the SCI-DC register, in order to calculate cost of diabetes relative to the non-diabetic population.
Outcomes
The primary outcomes of the study were any admission to hospital and, if admitted at least once, total cost of admission for that year. Outcomes were examined in relation to clinical variables including age, sex, type of diabetes, history of vascular admissions (ICD-9: 410-414, 430-438, 443; ICD-10: I20-25, I60-69, I73), HbA1c, serum creatinine, BMI and diabetes duration. BMI, serum creatinine and HbA1c were calculated as the yearly mean of all observations recorded between 2005 or date of diagnosis (if after 1 January 2005), and 2007 or date of death if before 31 December 2007. As well as looking at all admissions (excluding obstetric and psychiatric), subgroups of admission (hypoglycaemic, hyperglycaemic, cancer and vascular admissions) were determined using ICD-10 codes (see electronic supplementary material [ESM]).
Statistical methods
A two-part model clustered by person was used to examine which variables were associated with at least one admission within 1 year, and which variables were associated with the total cost of all admissions for people admitted within each year. The first part of the model estimated the probability of one or more hospital admission in a given year using logistic regression. The second part of the model estimated total cost of all admissions per year conditional on admission using generalised linear models (GLM) assuming a gamma distribution to handle right skew in the data. The expected (unconditional) cost of admission is calculated from the two-part model by combining the estimated cost of hospital admission in 1 year, conditional on an admission occurring, and the probability of admission. Following convention, costing estimates are given as mean and standard deviation [11]. Parametric relationships between continuous variables and outcomes were examined using the grouped smoothing and fractional polynomial methods [12]. Analyses were conducted in Stata version 11. Only linear relationships were included in final models as higher order relationships did not improve model fit.
Results
In total, 24,750 people (11%) with type 1 diabetes and 195,433 people (89%) with type 2 diabetes were identified with a prevalence of approximately 4.3% (total Scottish population 5.1 million) (Table 1). People with type 1 diabetes were younger, had lower BMI, and were less likely to have had prior vascular admission than those with type 2 diabetes, but had a longer duration of diabetes and a higher HbA1c.
Cost of admission
For both types of diabetes, the majority of admissions were single episode admissions (84%). In 2007, the crude rate of admission in people with diabetes was 546 admissions per 1,000 person-years (analysing 108,610 admissions) compared with 224 admissions per 1,000 person-years in the non-diabetic population (1.1 million admissions). The age- and sex-adjusted rate of 475 admissions per 1,000 person-years among people with diabetes reflects the 2.1-fold greater admission rate than among the non-diabetic population. Similarly costs were 2.2-fold higher in people with diabetes after adjustment for age and sex. The largest proportionate increase in rates of admission were in the youngest age groups (age < 25) where admission rates were increased 4.4-fold in male and 4.9-fold in female patients. Similarly, relative costs were increased most markedly in the youngest ages (4.0-fold in male and 4.7-fold in female patients). Average cost per admission was increased in people with diabetes with the largest relative increase in those aged 35–64 years.
In each year (2005–2007) approximately 6,000 people with type 1 diabetes (24% of all people with type 1) had one or more admission with a mean (SD) number of admissions in this group of 1.9 (2.2). People with type 2 diabetes, approximately 48,000 people (25%), had one or more admission (Table 1). Table 2 details the cost per admission for all causes, any diagnosis of hypoglycaemia and hyperglycaemia, and a primary diagnosis of vascular disease or cancer. The mean cost for any admission for type 1 diabetes was £2,424 (£2,013) with an annual estimated total cost of admissions of £26.7 million. For type 2 diabetes, the mean cost for any admission was £3,034 (£2,298) with an annual estimated total cost of admission of £275 million.
Predictors of hospital admission and cost of admission
To aid interpretation, the model using untransformed data was taken as the final model, because transformed variables provided minimally better model fit. Owing to missing data in the explanatory variables, the numbers of people included in the models were 19,753 for type 1 and 154,044 for type 2 diabetes (see Table 1). For type 1 diabetes, those with diabetes for less than 180 days were excluded.
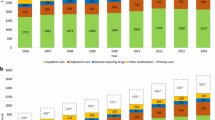
Increasing age and creatinine, female sex and previous vascular history in people with both type 1 and type 2 diabetes as well as insulin prescription in type 2 diabetes were associated with increased probability of admission to hospital in multivariate models (Table 3). Interestingly, greater BMI was associated with a reduced probability of hospital admission in both type 1 and type 2 diabetes (Table 3 and Fig. 1a, b). Higher HbA1c was associated with a marked increase in probability of admission in type 1 diabetes, but had a significant, if small, decreasing effect in type 2 diabetes. People with a shorter history of diabetes had slightly higher likelihood of admission to hospital.
Probability of at least one admission (a, b), the cost of admission per person per year in those with at least one admission (c, d), and expected, or unconditional cost (for all people with diabetes) of all admissions (e, f) for type 1 and type 2 diabetes, respectively, in a given year, as predicted by the models. Except where stated below the bars, the values for all model predictors are set to be the average values from Table 1 for a man with no previous vascular admission and, for type 2 diabetes, who had never taken insulin. For details of the units of the variables listed on the x-axes, please refer to Table 1. Creat., creatinine; PVE, previous vascular event
In both type 1 and type 2 diabetes, the cost of admission per person per year in the group with at least one admission increased with age, creatinine and previous vascular history, and decreased with greater BMI. Higher HbA1c was also associated with lower costs in type 2 diabetes (Table 3 and Fig. 1c, d).
Expected, or unconditional costs (Fig. 1e, f) describe the combination of the cost of an admission per person per year in the group with at least one admission and the probability of an admission, as demonstrated in the following example. A man with type 1 diabetes, who has no previous admission for vascular reasons, and with characteristics set to reflect the average values provided in Table 1, has a probability of admission of 0.22. The total cost of all admissions in a given year, conditional on at least one admission, was £3,854 and the expected cost of admission to hospital would be £855 (0.22 × £3,854).
In both type 1 and type 2 diabetes, younger age, no previous vascular admissions, shorter diabetes duration and lower creatinine were associated with lower costs per person per year for all those with diabetes (Fig. 1e, f). For type 2 diabetes, insulin prescription was associated with increased expected costs compared with those not prescribed insulin.
The results of analyses using the secondary outcomes of hypoglycaemia, hyperglycaemia, vascular disease, diabetic-related admission, and cancer are presented in Table 4. In type 1 diabetes, diabetes duration has a reduced effect on hyperglycaemia and diabetes-related admissions. In both types of diabetes HbA1c has an increased effect and age has a reduced effect on admission for hyperglycaemia. For both type 1 and type 2 diabetes, men are more likely to be admitted for vascular reasons, and HbA1c has a reduced effect on likelihood of admission for cancer. Those with type 2 diabetes receiving insulin have an increased risk of any admission, particularly for hyperglycaemia.
Discussion
Of the total Scottish inpatient expenditure (£2.4 billion), 12% of the cost of hospitalisations was attributable to the 4.3% of people in Scotland with diagnosed diabetes, a similar estimate to that achieved by the Welsh study [4]. In part, this increased expenditure reflects the older age of people with diabetes. However, we also show a doubling of hospital admission rates compared with the background population, after adjustment for age and sex. Younger age groups had the most marked increase in admission rate and total costs, while those in older age groups had the largest relative increase in cost per admission.
A number of risk factors and complications—including higher age, creatinine and previous vascular admission—have a predictable influence on the probability of admission and cost of admission. Longer duration of diabetes exerted only a small effect among people with type 2 diabetes and, indeed, reduced the probability of admission in type 1 diabetes. The effect of duration in type 1 diabetes appears to reflect admission early after diagnosis, as duration of diabetes has no effect when those who had diabetes for less than 180 days are included, but is a positive predictor of admission after excluding these people.
Less predictably, higher BMI appeared to be associated with lower likelihood of admission and costs in both type 1 and type 2 diabetes. One explanation is the possible concomitant effects of acute or chronic disease on BMI, with lower BMI acting as a marker of co-morbidity. Notably, a J-shaped relationship has been shown to exist between BMI and mortality [13], and a similar relationship between BMI and mortality appears to be present in the Scottish population [14]. Low BMI may also reflect undertreatment of hyperglycaemia, but we think that this is unlikely to be the explanation as we found that the effect of BMI was independent of recent HbA1c.
The relationship between HbA1c and admission was divergent in type 1 and type 2 diabetes. Higher HbA1c was associated with an increased risk of total admission in type 1 but slightly reduced overall risk of admission in type 2 diabetes. One obvious explanation of this is that, while HbA1c acts as a predictor of hyperglycaemia admissions in both type 1 and type 2 diabetes (Table 4), such admissions form a much larger proportion of total admissions in type 1 than type 2 diabetes (Table 2: 14.5% vs 0.3%). The population with type 2 diabetes is almost 30 years older on average and would be expected to have a much higher rate of admission for conditions either unrelated, or less directly related, to HbA1c. There are also important clinical differences between the two diseases. It is notable that the rates of hyperglycaemia admission are much higher in type 1 than type 2 diabetes with almost 0.06 admissions per year per person with type 1 diabetes, compared with 0.002 admissions per year per person with type 2 diabetes. Some of this may reflect hospital coding, but much will reflect underlying differences in the two conditions.
For type 1 diabetes, the effect of HbA1c was large. With all other variables held constant, the estimated probability of admission doubles if HbA1c was 12% compared with 6.5%. This is a clinically important effect given that 9% of people with type 1 diabetes had HbA1c >12% compared with 4% of people with HbA1c <6.5%. The result suggests that HbA1c is an important indicator of likelihood of both clinical complications and costs in people with type 1 diabetes. Along with attempts to avoid microvascular complications, the data suggest that those individuals with the highest HbA1c might usefully be supported in attempts to reduce hospital admissions and costs in type 1 diabetes but not type 2 diabetes. This is not to suggest that HbA1c is always necessarily causal in these admissions, but indicates that it is acting as a marker of risk of admission.
The relationship between admission and HbA1c in type 2 diabetes shows that those at the lowest levels of HbA1c have a slightly higher likelihood of admission and higher unconditional costs. This may reflect the influence of other co-morbidities and illness leading to reduction in HbA1c and increased probability of hospital admission. Notably, a recent study has also shown J-shaped relationships between HbA1c and survival [15] so that, while the relationship between HbA1c and admission may predominantly reflect reverse causality, a direct effect of lower HbA1c on risk of admission cannot be excluded.
This study took advantage of linked data for both hospital admissions (SMR-01) and clinical information (SCI-DC), providing almost 100% coverage of all data for people with diagnosed diabetes in Scotland during the period 2005–2007. This allowed accurate estimation of associations between patient characteristics and admission, avoiding underestimation as a result of underreporting of diabetes [3, 16] in hospital admission data. Few studies have estimated the cost of diabetes [5], and fewer have been able to examine type 1 and type 2 diabetes separately. These are distinct conditions and, although it has been recognised that the cost information should be estimated separately [17], this has only recently been possible.
People with diabetes accounted for 4.3% of the population but 12% of inpatient costs. This cost estimate is similar to that reported by investigators in Wales [4]. The estimates in both studies were also considerably higher than the previous studies conducted in Europe [1, 2], but lower than the USA [3]. There are several reasons why this may be the case. First, in contrast with our methods (individual patient records for hospitalisation), these studies use national data averages and small samples in order to extrapolate costs to the wider population. These methods may under- or over-estimate costs depending on the accuracy of the national estimates and the methods used. Second, the European study [1] uses data from eight countries, each with different national healthcare systems and data collection tools and methods. The US study [3] makes use of several medical claims databases, which the authors identify as being less accurate than clinical reports as a result of the under- or over-diagnosis of conditions. Our study has the advantage of using data from a single data source for hospitalisations, which is linked to the clinical registry for people with diabetes in Scotland. Finally, our study includes all people with diabetes in Scotland, while two of the studies only included those with type 2 diabetes who were over 30 years of age [1, 2], giving a lower prevalence and, therefore, lower cost estimates.
A number of factors suggest that costs may still be underestimated. First, costs were attributed for different types of admission using HRG codes using the Scottish National Tariff. This system does not account for differences in individual length of stay [8]. As has been suggested by others [18], these may be systematically higher in people with diabetes, leading to underestimation of costs. This is also the case in our data where, while people with diabetes account for 12% of admissions, they account for 18% of hospital days. Second, for admissions with multiple episodes of care, the most expensive episode was chosen as the cost of admission. The estimates of cost for such admissions are therefore conservative since additional episodes are not taken into account, although this approach has the advantage of avoiding double counting of shared costs.
Third, this analysis was restricted to inpatient cost of diabetes and does not include ambulatory care or prescription costs. Previous studies suggest that inpatient costs will account for around 50% of total healthcare costs for people with diabetes [1–3]. Prescription costs were not available on an individual basis. Data from the Scottish Prescription Costs Analysis [19] shows that prescription costs for drugs used in the direct treatment of diabetes (£163 million) was 5.6% of the total Scottish expenditure for all drugs (£2.9 billion) for years 2005–2007. The cost of all drugs used in the care of people with diabetes will be higher.
Fourth, costs in this analysis relate to diagnosed diabetes while those as yet undiagnosed may comprise a further 1% of the population [20]. Finally, indirect costs such as lost productivity were not included. It is likely, then, that the costs presented are a lower limit of the total cost burden of diabetes.
In summary, this study shows that people with diabetes account for a high proportion of inpatient costs. The findings reinforce the importance of addressing modifiable risk factors for cardiovascular and renal disease in both type 1 and type 2 diabetes, and optimal glycaemic control in type 1 diabetes. This suggests that HbA1c might be useful as a marker for programmes supporting people with diabetes to remain well and out of hospital.
Abbreviations
- CHI:
-
Community Health Index
- GLM:
-
Generalised linear models
- GROS:
-
General Register Office for Scotland
- HRG:
-
Healthcare Resource Groups
- ICD:
-
International Classification of Disease
- ISD:
-
Information Services Division
- SCI-DC:
-
Scottish Care Information—Diabetes Collaboration
- SDRN:
-
Scottish Diabetes Research Network
- SHIP:
-
Scottish Health Informatics Programme
- SMR-01:
-
Scottish morbidity records
References
Jönsson B, CODE-2 Advisory Board (2002) Revealing the cost of type II diabetes in Europe. Diabetologia 45:S5–S12
Nolan JJ, O'Halloran D, McKenna TJ, Firth R, Redmond S (2006) The cost of treating type 2 diabetes (CODEIRE). Ir Med J 99:307–310
American Diabetes Association (2008) Economic costs of diabetes in the U.S. in 2007. Diabetes Care 31:596–615
Morgan CL, Peters JR, Dixon S, Currie CJ (2010) Estimated costs of acute hospital care for people with diabetes in the United Kingdom: a routine record linkage study in a large region. Diabet Med 27:1066–1073
Gray A, Fenn P, McGuire A (1995) The cost of insulin-dependent diabetes mellitus (IDDM) in England and Wales. Diabet Med 12:1068–1076
Colhoun HM, SDRN Epidemiology Group (2009) Use of insulin glargine and cancer incidence in Scotland: a study from the Scottish Diabetes Research Network Epidemiology Group. Diabetologia 52:1755–1765 (Erratum 52:2469)
Information Services, NHS National Services Scotland (2010) Scottish National Tariff Project. www.isdscotland.org/isd/3552.html. Accessed September 2010
Information Services, NHS National Services Scotland (2009) Scottish Health Service Costs. www.isdscotland.org/isd/360.html. Accessed September 2010
Department of Health, NHS England (2010) NHS Costing and Cost Collection. www.dh.gov.uk/en/Managingyourorganisation/Financeandplanning/NHScostingmanual/index.htm. Accessed September 2010
The Health and Social Care Information Centre (2010) What are Healthcare Resource Groups (HRGs)? www.ic.nhs.uk/services/the-casemix-service/new-to-this-service/what-are-healthcare-resource-groups-hrgs. Accessed September 2010
Briggs A (1998) Given the distributional nature of costing and resource utilisation, is it more approriate to use median or mean descriptive statistics? J Health Serv Res Policy 3:127
Hosmer DW, Lemeshow S (2000) Applied logistic regression, 2nd edn. Wiley, New York
Prospective Studies Collaboration (2009) Body-mass index and cause-specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet 373:1083–1096
Wild S, SDRN Epidemiology Group (2010) Body mass index and mortality among people with diabetes: a retrospective population based cohort study. American Diabetes Association 0328-OR (Abstract)
Currie CJ, Peters JR, Tynan A et al (2010) Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet 375:481–489
Leslie PJ, Patrick AW, Hepburn DA, Scougal IJ, Frier BM (1992) Hospital in-patient statistics underestimate the morbidity associated with diabetes mellitus. Diabet Med 9:379–385
Gerard K, Donaldson C, Maynard AK (1989) The cost of diabetes. Diabet Med 6:164–170
Laditka SB, Mastanduno MP, Laditka JN (2001) Health care use of individuals with diabetes in an employer-based insurance population. Arch Intern Med 161:1301–1308
Information Services, NHS National Services Scotland (2009) Prescription Cost Analysis Scotland. www.isdscotland.org/isd/information-and-statistics.jsp?pContentID=2241&p_applic=CCC&p_service=Content.show. Accessed September 2010
Holt TA, Stables D, Hippisley-Cox J, O'Hanlon S, Majeed A (2008) Identifying undiagnosed diabetes: cross-sectional survey of 3.6 million patients' electronic records. Br J Gen Pract 58:192–196
Acknowledgements
These data were available for analysis by members of the Scottish Diabetes Research Network (SDRN) thanks to the hard work and dedication of NHS staff across Scotland who enter the data and people and organisations (SCI-DC Steering Group, the Scottish Diabetes Group, the Scottish Diabetes Survey Group, the managed clinical network managers and staff in each Health Board) involved in setting up, maintaining and overseeing SCI-DC. The SDRN receives core support from the Chief Scientist’s Office at the Scottish Government Health Department. The cost data linkage were covered by the Scottish Government Health Department. This work was funded by the Wellcome Trust through the Scottish Health Informatics Programme (SHIP) Grant (ref. WT086113). SHIP is a collaboration between the Universities of Aberdeen, Dundee, Edinburgh, Glasgow and St Andrews and the Information Services Division of NHS Scotland.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The SDRN Epidemiology Group: H. Anwar, J. Chalmers, S. Cunningham, T. deWees, A. Emslie-Smith, C. M. Fischbacher, S. Hynd, A. Judson, J. Kernthaler, G. P. Leese, S. Livingstone, R. McAlpine, M. McGilchrist, S. Philip, F. Sullivan, J. J. Walker
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
Description of outcomes and their ICD-10 codes (PDF 14 kb)
Rights and permissions
About this article
Cite this article
Govan, L., Wu, O., Briggs, A. et al. Inpatient costs for people with type 1 and type 2 diabetes in Scotland: a study from the Scottish Diabetes Research Network Epidemiology Group. Diabetologia 54, 2000–2008 (2011). https://doi.org/10.1007/s00125-011-2176-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-011-2176-7