Abstract
Aims/hypothesis
In skeletal muscle, ceramides may be involved in the pathogenesis of insulin resistance through an attenuation of insulin signalling. This study investigated total skeletal muscle ceramide fatty acid content in participants exhibiting a wide range of insulin sensitivities.
Methods
The middle-aged male participants (n=33) were matched for lean body mass and divided into four groups: type 2 diabetes (T2D, n=8), impaired glucose tolerance (IGT, n=9), healthy controls (CON, n=8) and endurance-trained (TR, n=8). A two step (28 and 80 mU m−2 min−1) sequential euglycaemic–hyperinsulinaemic clamp was performed for 120 and 90 min for step 1 and step 2, respectively. Muscle biopsies were obtained from vastus lateralis at baseline, and after steps 1 and 2.
Results
Glucose infusion rates increased in response to insulin infusion, and significant differences were present between groups (T2D<IGT<CON<TR). At baseline, muscle ceramide content was 108±7, 95±6, 126±12 and 156±25 nmol total ceramide fatty acids/g wet weight of tissue in the T2D, IGT, CON and TR groups, respectively, and muscle ceramide content was higher (p<0.01) in the TR than the IGT group. Muscle ceramide content was not influenced by insulin infusion. Interestingly, a positive correlation (r=0.42, p<0.05) was present between muscle ceramide content at baseline and insulin sensitivity.
Conclusions/interpretation
Total muscle ceramide content was similar between individuals showing marked differences in insulin sensitivity, and therefore does not seem to be a major factor in muscle insulin resistance. Furthermore, aerobic capacity does not appear to influence muscle ceramide content.
Similar content being viewed by others
Introduction
The appearance of insulin resistance is considered one of the early signs of metabolic dysfunction, which, left untreated, will eventually lead to major metabolic derangements and overt diabetes and/or the metabolic syndrome [1]. In obesity and type 2 diabetes, decreased fat metabolism and an accumulation of triacylglycerol has been observed in skeletal muscle, the major site of insulin resistance [2]. In a number of studies, but not all [3], an inverse relationship between insulin sensitivity and intramyocellular triacylglycerol storage has been found [4–7]. Consistent with this notion, an increase in NEFA concentrations by lipid infusion leads to decreased insulin sensitivity [8] and increased intramyocellular triacylglycerol stores [2]. However, excess intramyocellular triacylglycerol storage in itself probably does not decrease muscle insulin sensitivity, but, rather, acts as a source for lipid derivatives, such as diacylglycerol, long chain fatty acyl-CoA or ceramides, that directly influence insulin signalling and, thus, insulin sensitivity [9, 10].
In humans, direct evidence for the involvement of muscle ceramide in attenuation of insulin sensitivity is limited. Two studies have demonstrated higher muscle ceramide content in obese insulin-resistant individuals compared with lean insulin-sensitive individuals [11, 12], and a recent study found that 8weeks of training reduced muscle ceramide content in young obese insulin-resistant individuals and improved glucose tolerance [13]. However, in contrast, we observed similar muscle ceramide content in endurance-trained compared with untrained normal young men [14]. Studies using lipid infusion to decrease insulin sensitivity under a euglycaemic–hyperinsulinaemic clamp have also produced conflicting results: one group observed no change in muscle ceramide levels after 6 h [15], whereas another group found that ceramide levels were increased after 4h [16]. Overall, it is not clear from the literature whether muscle ceramide content plays a major role in skeletal muscle insulin sensitivity. To help elucidate the answer to this question, the aim of the present study was to measure insulin sensitivity and total muscle ceramide content in skeletal muscle in a group of participants exhibiting the full spectrum of insulin sensitivity, from type 2 diabetes to endurance-trained highly insulin-sensitive subjects.
Methods
The 33 male participants of this study were stratified according to their glucose tolerance and training status into four groups: type 2 diabetes (T2D, n=8), overweight or obese participants with impaired glucose tolerance (IGT, n=9), healthy but sedentary controls (CON, n=8), and endurance-trained participants (TR, n=8). The groups were matched for age and lean body mass (Table 1). None of the participants in the CON or TR control groups had a family history of type 2 diabetes. Use of medication generally excluded individuals from the study, but oral hypoglycaemic agents and insulin were accepted for those with type 2 diabetes, provided they were not used on the day of screening or on the day of the experiment. Participants were instructed to abstain from alcohol, tobacco and strenuous exercise for 48 h prior to screening and the experiment. The purpose of the experiment, together with potential risks and unpleasantness were explained to all participants, and all gave signed consent prior to inclusion in the study. The study was approved by the Copenhagen and Fredriksberg Ethical Committee (KF 01-091/02) and was conducted according to the principles of the Declaration of Helsinki.
Testing procedure
The participants were studied after an overnight fast (approximately 10h) on two separate days—1 day to test and stratify the participants into their respective groups and 1 day to perform the experiment. On the first day, height and weight were measured, and then a venous blood sample was obtained and an OGTT performed. Body composition was determined from dual-energy X-ray absorptiometry (DPX-IQ 240; Lunar, Madison, WI, USA). Peak oxygen uptake (\( {\mathop {V{\text{O}}}\limits^ \cdot }_{{2\max }} \)) was determined using a graded exercise test, starting at 50 W for 5 min followed by increments of 25 W every minute until exhaustion, on a semi-supine bike. Pulmonary oxygen consumption was monitored on an online system (Oxycon Pro system; Jaeger, Hoechberg, Germany). A normal resting and exercise ECG reading, performed during a separate short exercise bout, was a prerequisite for participation in the maximal test.
Experimental procedure
On arrival, body weight was measured and participants were placed in a bed. After a 20 min rest period, a catheter was inserted into the antecubital vein for later infusion of insulin and glucose and another was inserted (retrograde direction) into a superficial hand vein. The hand was placed in a heating pad for sampling of arterialised venous blood. Baseline blood samples were drawn and a muscle biopsy sample was obtained from the vastus lateralis muscle using the Bergström needle technique with suction [17]. Hereafter, a two step sequential euglycaemic–hyperinsulinaemic clamp was initiated, step 1 lasting 120 min and step 2 lasting 90 min. A 50 ml insulin infusate was prepared for each clamp step by mixing insulin (Actrapid, 100 U/ml; Novo Nordisk, Copenhagen, Denmark) with 2.5 ml of the participant’s own plasma and isotonic saline (0.9% [wt/vol.] NaCl) to reach a final volume of 50 ml. After a 2 ml bolus, the insulin infusate was administered by continuous intravenous infusion at rates of 28 mU m−2 min−1 (step 1) and 80 mU m−2 min−1 (step 2). The patients with type 2 diabetes were given extra insulin to achieve euglycemia (target: 5.5 mmol/l). During the clamp, two tablets of potassium were administered orally (40 mmol Kaleroid; LEO, Copenhagen, Denmark) to prevent insulin-induced hypokalaemia. The initial glucose infusion rate was empirically set between 0 and 2 mg min−1 kg−1, depending on the baseline plasma glucose concentration. The glucose infusion rate (GIR) was adjusted according to frequent measurements (~5 min intervals) of plasma glucose concentrations using a whole blood analyser (ABL 625; Radiometer, Copenhagen, Denmark). A muscle biopsy sample from the vastus lateralis muscle was obtained after both steps, either through a new incision or with the biopsy needle inserted in the opposite direction to that of an earlier biopsy. Heart rate was monitored throughout the experiment.
Analyses of plasma substrate and hormones
Blood samples were collected in chilled tubes, immediately centrifuged at 2,500×g at 4°C, and the plasma fraction collected and stored at −80°C and −20°C prior to the determination of plasma NEFA and insulin concentrations, respectively. Insulin concentrations in plasma were determined by ELISA (Dako, Ely, UK) and plasma NEFA concentrations were determined using a Wako NEFA-C test kit (Wako Chemical, Neuss, Germany).
Analysis of muscle biopsy samples
Muscle tissue was frozen in liquid nitrogen within 10–15 s of sampling. Before freezing, a section of each sample was cut off, mounted in embedding medium, and frozen in isopentane cooled to its freezing point in liquid nitrogen. Both parts of each biopsy sample were stored at −80°C until further analysis. Serial transverse muscle sections were cut from the embedded muscle tissue and then stained for myofibrillar ATPase to identify fibre type composition [18]. Muscle triacylglycerol content was analysed as previously described [19, 20].
The muscle biopsies were also analysed for total ceramide fatty acid content and ceramide fatty acid composition via methods previously described [21]. The coefficient of variation for the ceramide content analysis, when analysed in triplicate in rat muscle, was 8.6%.
Calculations
Mean plasma glucose and infusion rates were determined for 5 min periods during all clamp steps. During both clamp steps, steady-state conditions were reached for the last 30 min of the clamp step, and steady-state glucose infusion rates were thus calculated over this period.
Statistics
The statistics were performed using Sigma Stat for Windows, version 2.3 (Systat Software, Erkrath, Germany). All data are presented as means±SEM. A p value of <0.05 was regarded as significant. Data were tested for normal distribution, and log transformation was used when data were not normally distributed. Comparisons of participant characteristics were made using one-way ANOVA. Two-way ANOVA with repeated measures was used to test for between-group and between-step differences for parameters measured during the clamp. Whenever the ANOVA tests revealed significant effects, the Tukey’s post hoc test for multiple comparisons was used. Pearson’s product moment correlation coefficient was calculated for correlation analysis.
Results
A total of 33 middle-aged male participants were recruited and divided into four groups that were matched with respect to age and lean body mass (Table 1). The OGTT and the \( {\mathop {V{\text{O}}}\limits^ \cdot }_{{2\max }} \) data collected at baseline were used to classify the four groups. The TR group had a lower BMI than the T2D, IGT and CON groups, which had similar BMIs (Table 1). Body fat content was slightly lower in the CON group than the IGT group, and was significantly lower in the TR group than in the other groups (Table 1). The fibre composition of the vastus lateralis muscle was similar in the T2D, IGT and CON groups, whereas the TR group had a significantly higher type I fibre content and a lower type IIX fibre content (Table 1).
Prior to the initiation of the clamp, plasma glucose concentrations were 11.6±1.4, 5.7±0.2, 5.5±0.2 and 5.2±0.1 mmol/l in the T2D, IGT, CON and TR group, respectively. During the first part of the clamp (step 1), plasma glucose concentrations were reduced to 6.0±0.2 mmol/1 in T2D group, and euglycaemia was well maintained at 5.6±0.1, 5.6±0.1 and 5.6±0.1 mmol/l in the IGT, CON and TR group, respectively. During step 2, there were no differences in plasma insulin concentrations between groups (Table 2).
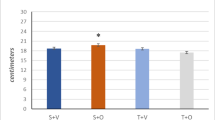
During step 1, at an insulin infusion rate of 28 mU min−1 m−2, there was no significant difference in steady-state GIRs (ssGIRs) between the T2D and IGT groups, but the difference in ssGIR between the CON and T2D groups approached statistical significance (p=0.074; Fig. 1). Furthermore, the TR group had a higher (p<0.05) ssGIR than the other groups. During step 2, at which point insulin infusion rates were raised to 80 mU min−1 m−2, ssGIR was increased in all groups compared with step 1 (Fig. 1). It was significantly higher (p<0.05) in the IGT and CON groups vs the T2D group, and in the TR group vs the IGT and T2D groups (Fig. 1).
ssGIRs during sequential euglycaemic–hyperinsulinaemic clamp steps in the four groups: T2D (n = 8), IGT (n = 9), CON (n = 8) and TR (n = 8). Insulin was infused at 28 (step 1) and 80 (step 2) mU min−1 m−2. Data are the means ± SEM for eight (T2D, CON and TR groups) or nine (IGT group) participants. *p < 0.05 vs T2D, IGT and CON groups; † p < 0.05 for step 1 vs step 2; ‡ p < 0.05 vs TR group; ¶ p < 0.05 vs IGT, CON and TR groups
Insulin sensitivity measured by the euglycaemic–hyperinsulinaemic glucose clamp was in very good agreement with glucose tolerance determined by OGTT, which was used to categorise the participants (Table 1, Fig. 1). In this study we used ssGIR at step 2 as the index for insulin sensitivity, because a similar and well-controlled level of euglycaemia was achieved for all four groups. However, similar differences between groups and correlations are observed if step 1 is used.
At baseline, plasma NEFA was highest in the T2D group and higher in the CON and IGT groups than the TR group (Table 2). During clamp step 1, plasma NEFA concentrations were lower (p<0.01) in the TR group than the other groups (Table 2). At step 2, plasma NEFA concentrations remained significantly higher (p<0.05) in the T2D group compared with the other groups, and were higher (p<0.05) in the CON and IGT groups than in the TR group (Table 2).
At baseline, total muscle ceramide fatty acid content was similar between groups (Fig. 2). After both clamp step 1 and step 2 the total muscle ceramide fatty acid content was similar in all groups, and neither low nor moderately high insulin stimulation affected total muscle ceramide fatty acid content (Fig. 2). Ceramide fatty acid composition was also studied, and the distribution of individual fatty acids is presented in Table 3. At baseline, ceramide fatty acid composition was similar between groups (Table 3). Furthermore, ceramide fatty acid composition was not influenced by insulin stimulation. Muscle triacylglycerol was only measured in the baseline biopsies, as no measurable changes were expected for this parameter based on the experimental design. In agreement with this notion, no significant differences were found between the groups at baseline, with triacylglycerol levels of 68.9±21.4, 38.5±6.8, 35.6±10.0 and 49.7±12.6nmol/mg in T2D, IGT, CON and TR, respectively.
We observed a weak positive (r=0.42, p<0.05) correlation between insulin sensitivity and muscle ceramide content measured at baseline (Fig. 3). Of interest, this correlation is not present if the data for the TR group are excluded from the statistical analyses. The inverse correlation between insulin sensitivity and muscle triacylglycerol did not reach statistical significance (r = −0.33, p = 0.08) in this study. Furthermore, total muscle ceramide content was not significantly correlated with either intramuscular triacylglycerol or fasting plasma NEFA concentration. However, we did find a significant inverse correlation between total muscle ceramide fatty acid concentration and body fat mass (Fig. 3). Again, this significant correlation disappears if the data for the TR group are excluded.
Correlations of total muscle ceramide content in the T2D (squares, n = 8), IGT (triangles, n = 9), CON (circles, n = 8) and TR (diamonds, n = 8) groups with (a) GIR during an euglycaemic–hyperinsulinaemic clamp (step 2) with insulin infused at 80 mU min−1 m−2 and (b) total body fat mass. Data are means ± SEM. Pearson’s correlation: (a) r = 0.42, p = 0.02; (b) r = −0.53, p < 0.01
Discussion
The novel finding of this study is the similar ceramide concentration in skeletal muscle from middle-aged men over a very wide variety of insulin sensitivities, ranging from type 2 diabetes patients to healthy controls. In fact, a positive, albeit weak, correlation was observed between muscle ceramide concentration and insulin sensitivity, which is somewhat surprising given that two prior studies have suggested the presence of an inverse correlation between muscle ceramide content and insulin sensitivity [12, 16]. Moreover, as neither low nor high insulin influenced muscle ceramide content, it seems that, in man, muscle ceramide does not play a key role in insulin-mediated glucose uptake. We did not observe any differences in the relative levels of ceramide fatty acid species between these groups, which further implies that muscle content of specific ceramide fatty acids species is not the major effector of insulin sensitivity in man.
Muscle ceramide content and insulin resistance
In vitro work in cell lines and studies of rat muscle have demonstrated that increased skeletal muscle ceramide content attenuates insulin signalling through serine/threonine phosphorylation of Akt/protein kinase B, which leads to impaired translocation of GLUT4 to the plasma membrane and an attenuated activation of glycogen synthase [9, 22]. However, it is yet not clear to what extent ceramide influences insulin sensitivity in vivo in skeletal muscle in man. In this study, muscle ceramide concentrations were similar in four groups of men, ranging from type 2 diabetic to endurance-trained individuals, thus representing a very broad range of insulin sensitivities. This observation is consistent with our results in a previous study on young male untrained and endurance-trained participants, presumably having different insulin sensitivities, in which muscle ceramide content was similar in the resting overnight fasted condition [14]. As mentioned above, our finding is in contrast to two studies that found higher muscle ceramide content in young obese insulin-resistant participants compared with lean controls [11, 12]. This discrepancy could be explained by the presence of an increased muscle ceramide concentration in obese individuals. However, Serlie and colleagues found lean and overweight individuals to have similar muscle ceramide concentrations [23], and we observed no differences in muscle ceramide levels despite a difference in body weight between the TR group and the other three groups in the present study. There is evidence from rat skeletal muscle that ceramide content in IIX muscle fibres is lower than that in I and IIA muscle [18]. Therefore, markedly higher muscle fibre type I content in the TR group compared with the three other groups in this study would counter a possible difference in muscle ceramide content related to insulin resistance. It is not easy to reconcile these findings, but it can be speculated that a threshold of obesity may exist, above which muscle ceramide accumulates and influences insulin signalling and thus insulin sensitivity. Furthermore, unlike the studies described above, the present study enrolled middle-aged men, and it is possible that age could influence muscle ceramide concentrations. However, the observation of higher muscle ceramide content in offspring of type 2 diabetic individuals compared with age- and BMI-matched healthy men [12], and the knowledge that this group have an increased or similar skeletal muscle type IIX fibre content compared with lean controls [24, 25], clearly indicates that factors other than age and BMI must be considered if the mechanisms that regulate muscle ceramide content are to be understood.
There is evidence from a rodent model that excess glucocorticoids and saturated fatty acids leads to increased muscle ceramide concentration and subsequent insulin resistance, and that this could be reversed through pharmacological agents [26]. In the same study it was demonstrated that unsaturated fatty acids did not induce insulin resistance through muscle ceramide accumulation, but, rather, through increased muscle diacylglycerol content [26]. This implies that, at least in rodents, the type of fatty acid available, which is dependent upon both dietary consumption and stored fatty acids, may play a very important role in the metabolic events that lead to insulin resistance. Similar data are not available for humans, but there is evidence that lipid infusion using primarily unsaturated fatty acids leads to insulin resistance without a change in muscle ceramide [15, 27]. In the present study, we cannot exclude the possibility that the composition of the available fatty acids may have influenced the muscle ceramide concentration and that this may be an important factor for the mechanisms that determine insulin sensitivity. Further studies in humans are needed to elucidate the influence of specific fatty acids on muscle ceramide content.
Effect of insulin on muscle ceramide content
In the present study, muscle ceramide content was not influenced by stimulation with low or high insulin levels during the clamp, which is consistent with prior observations showing no effect of insulin on muscle ceramide content in human skeletal muscle [11, 15, 16]. Muscle ceramides are generated primarily through de novo synthesis from palmitate and serine, or through the breakdown of sphingomyelin in the membranes [22, 28, 29]. During insulin stimulation, plasma fatty acids are markedly decreased through insulin-induced inhibition of adipose tissue lipolysis, and de novo synthesis is therefore very limited as a result of reduced palmitate availability. When plasma NEFA levels were increased by lipid infusion during an euglycaemic–hyperinsulinaemic clamp, muscle ceramide content remained unchanged [15] or was increased [16] in healthy men. This inconsistency between studies may have been due to the somewhat higher plasma NEFA concentrations observed after lipid heparin infusion in the study by Straczkowski [16]. It is not clear whether the generation of ceramide from sphingomyelin degradation in human skeletal muscle is influenced by insulin infusion and/or the ceramide degradation is influenced by insulin. However, the presence of unchanged muscle ceramide content in this and prior studies [11, 15] and the unchanged muscle ceramide fatty acid composition in the present study suggest that this is not the case.
Effect of training on muscle ceramide content
In a recent training study, muscle ceramide content was decreased in obese individuals after 8 weeks of endurance training [13]. In rats, 6 weeks of endurance training also led to a decreased muscle ceramide content [30]. In contrast, muscle ceramide content was similar between the four groups in the present study. Furthermore, we did not observe any difference in muscle ceramide content between untrained and trained young male healthy participants in our prior study [14]. The two latter studies used a cross-sectional design as opposed to the longitudinal design of the two aforementioned training studies [13, 30] and therefore further studies on humans using a longitudinal design are important to further our understanding of the role of training on muscle ceramide content.
Triacylglycerol and ceramide in muscle
In the present study, muscle triacylglycerol stores were not significantly different between the four groups, and there was no significant coupling between intramuscular triacylglycerol and insulin sensitivity. Since the present study included an endurance-trained group, this is consistent with data from Goodpaster and colleagues [31], and is in line with previous studies that did not find coupling when muscle triacylglycerol was measured biochemically in samples of muscle tissue [3, 32].
It is generally thought that excess intramyocellular lipid storage results in decreased insulin sensitivity because an increased fatty acid precursor supply leads to increased concentrations of one or more of the lipid intermediates: diacylglycerol, long-chain fatty acyl-CoA or ceramide [9, 33, 34]. In support of this notion, Itani and colleagues found that insulin sensitivity was decreased after increasing plasma NEFA with a lipid infusion during an euglycaemic–hyperinsulinaemic clamp, and this occurred in parallel with an increase in intramuscular diacylglycerol, but not ceramide [15]. Using a similar approach, Straczkowski and colleagues [16] showed that lipid infusion reduced insulin sensitivity, and this coincided with increased muscle ceramide content. Lastly, Bruce and colleagues [13] found that glucose tolerance was increased and muscle ceramide levels were decreased after 8 weeks of training. Although these studies did not actually document changes in muscle triacylglycerol stores [13, 15, 16], they lend some support for relationships between muscle triacylglycerol, changes in insulin sensitivity and increased concentrations of the lipid intermediates diacylglycerol or ceramide. In the present study, no relationship was found between intramuscular triacylglycerol content and muscle ceramide content. However, we cannot exclude the possibility that muscle diacylglycerol or long chain fatty acyl-CoA may have influenced insulin sensitivity.
Conclusion
In this study we demonstrate similar muscle ceramide concentrations in middle-aged men over a very wide range of insulin sensitivities, from type 2 diabetes to healthy controls. Moreover, muscle ceramide content was not measurably influenced by low or high insulin levels, suggesting that muscle ceramide content does not seem to play a key role in insulin sensitivity in man. It was not possible to discern differences in ceramide fatty acid species between groups, which supports the observation of similar muscle ceramide content across the groups and interventions. However, further studies are needed to fully elucidate the role of muscle ceramide, ceramide fatty acid species and ceramide intermediates in insulin sensitivity, and the mechanisms involved.
Abbreviations
- GIR:
-
glucose infusion rate
- ssGIR:
-
steady-state glucose infusion rate
- \( {\mathop {V{\text{O}}}\limits^ \cdot }_{{2\max }} \) :
-
peak oxygen uptake
References
Reaven GM (2005) The metabolic syndrome: requiescat in pace. Clin Chem 51:931–938
Boden G, Lebed B, Schatz M, Homko C, Lemieux S (2001) Effects of acute changes of plasma free fatty acids on intramyocellular fat content and insulin resistance in healthy subjects. Diabetes 50:1612–1617
Helge JW, Dela F (2003) Effect of training on muscle triacylglycerol and structural lipids: a relation to insulin sensitivity? Diabetes 52:1881–1887
Pan DA, Lillioja S, Kriketos AD et al (1997) Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 46:983–988
Sinha R, Dufour S, Petersen KF et al (2002) Assessment of skeletal muscle triglyceride content by 1H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes 51:1022–1027
Virkamaki A, Korsheninnikova E, Seppala-Lindroos A et al (2001) Intramyocellular lipid is associated with resistance to in vivo insulin actions on glucose uptake, antilipolysis, and early insulin signaling pathways in human skeletal muscle. Diabetes 50:2337–2343
Greco AV, Mingrone G, Giancaterini A et al (2002) Insulin resistance in morbid obesity: reversal with intramyocellular fat depletion. Diabetes 51:144–151
Boden G, Chen X, Ruiz J, White JV, Rossseti L (1994) Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest 93:2438–2446
Summers SA (2006) Ceramides in insulin resistance and lipotoxicity. Prog Lipid Res 45:42–72
Summers SA, Garza LA, Zhou H, Birnbaum MJ (1998) Regulation of insulin-stimulated glucose transporter GLUT4 translocation and Akt kinase activity by ceramide. Mol Cell Biol 18:5457–5464
Adams JM, Pratipanawatr T, Berria R et al (2004) Ceramide content is increased in skeletal muscle from obese insulin-resistant humans. Diabetes 53:25–31
Straczkowski M, Kowalska I, Baranowski M et al (2007) Increased skeletal muscle ceramide level in men at risk of developing type 2 diabetes. Diabetologia 50:2366–2373
Bruce CR, Thrush AB, Mertz VA et al (2006) Endurance training in obese humans improves glucose tolerance, mitochondrial fatty acid oxidation and alters muscle lipid content. Am J Physiol Endocrinol Metab 291:E99–E107
Helge JW, Dobrzyn A, Saltin B, Gorski J (2004) Exercise and training effects on ceramide metabolism in human skeletal muscle. Exp Physiol 89:119–127
Itani SI, Ruderman NB, Schmieder F, Boden G (2002) Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IkappaB-alpha. Diabetes 51:2005–2011
Straczkowski M, Kowalska I, Nikolajuk A et al (2004) Relationship between insulin sensitivity and sphingomyelin signaling pathway in human skeletal muscle. Diabetes 53:1215–1221
Bergström J (1962) Muscle electrolytes in man: determined by neutron activation analysis on needle biopsy specimens. A study on normal subjects, kidney patients and patients with chronic diarrhea. Scand J Clin Lab Invest Suppl 68:11–13
Brooke MH, Kaiser KK (1970) Three ‘myosin ATPase’ systems: the nature of their pH lability and sulfhydryl dependence. J Histochem Cytochem 18:670–672
Kiens B, Richter EA (1996) Types of carbohydrate in an ordinary diet affect insulin action and muscle substrates in humans. Am J Clin Nutr 63:47–53
Helge JW, Biba TO, Galbo H, Gaster M, Donsmark M (2006) Muscle triacylglycerol and hormone-sensitive lipase activity in untrained and trained human muscles. Eur J Appl Physiol 97:566–572
Dobrzyn A, Gorski J (2002) Ceramides and sphingomyelins in skeletal muscles of the rat: content and composition. Effect of prolonged exercise. Am J Physiol Endocrinol 282:E277–E285
Gorski J, Dobrzyn A, Zendzian-Piotrowska M (2002) The sphingomyelin-signaling pathway in skeletal muscles and its role in regulation of glucose uptake. Ann N Y Acad Sci 967:236–248
Serlie MJ, Meijer AJ, Groener JE et al (2007) Short-term manipulation of plasma free fatty acids does not change skeletal muscle concentrations of ceramide and glucosylceramide in lean and overweight subjects. J Clin Endocrinol Metab 92:1524–1529
Nyholm B, Qu Zq, Kaal A et al (1997) Evidence of an increased number of type IIB muscle fibers in insulin resistant first degree relatives of patients with NIDDM. Diabetes 46:1822–1828
Ostergard T, Andersen JL, Nyholm B et al (2006) Impact of exercise training on insulin sensitivity, physical fitness, and muscle oxidative capacity in first-degree relatives of type 2 diabetic patients. Am J Physiol Endocrinol Metab 290:E998–E1005
Holland WL, Brozinick JT, Wang LP et al (2007) Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance. Cell Metab 5:167–179
Vistisen B, Hellgren LI, Vadset T et al (2008) Effect of gender on lipid-induced insulin resistance in obese subjects. Eur J Endocrinol 158:61–68
Schmitz-Peiffer C (2000) Signalling aspects of insulin resistance in skeletal muscle: mechanisms induced by lipid oversupply. Cell Signal 12:583–594
Schmitz-Peiffer C, Craig DL, Biden TJ (1999) Ceramide generation is sufficient to account for the inhibition of the insulin-stimulated PKB pathway in C2C12 skeletal muscle cells pretreated with palmitate. J Biol Chem 274:24202–24210
Dobrzyn A, Zendzian-Piotrowska M, Gorski J (2004) Effect of endurance training on the sphingomyelin-signalling pathway activity in the skeletal muscles of the rat. J Physiol Pharmacol 55:305–313
Goodpaster BH, He J, Watkins S, Kelley DE (2001) Skeletal muscle lipid content and insulin resistance: evidence for a paradox in endurance-trained athletes. J Clin Endocrinol Metab 86:5755–5761
Kiens B (2006) Skeletal muscle lipid metabolism in exercise and insulin resistance. Physiol Rev 86:205–243
Goodpaster BH, Kelley DE (2002) Skeletal muscle triglyceride: marker or mediator of obesity-induced insulin resistance in type 2 diabetes mellitus? Curr Diab Rep 2:216–222
Kelley DE, Goodpaster BH (2001) Skeletal muscle triglyceride. An aspect of regional adiposity and insulin resistance. Diabetes Care 24:933–941
Acknowledgements
Financial support from The 1991 Pharmacy Foundation, NOVO Nordic Foundation, Direktør Verner Richter og Hustrus Fond, The Foundation of 1870, Direktør Jacob og Olga Madsens Foundation, Aase and Ejnar Danielsens foundation, Simon Fougner Hartmanns Foundation, Eva and Hans Carl Adolf Holms Grant, Else and Mogens Wedell-Wedellsborgs Foundation and EU project EXGENESIS 005272 is gratefully acknowledged. Furthermore, we thank T. Beck, J. Bach and R. Kraunsøe for providing excellent technical assistance.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Skovbro, M., Baranowski, M., Skov-Jensen, C. et al. Human skeletal muscle ceramide content is not a major factor in muscle insulin sensitivity. Diabetologia 51, 1253–1260 (2008). https://doi.org/10.1007/s00125-008-1014-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1014-z