Abstract
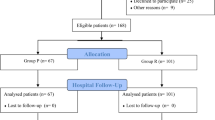
Cesarean section (CS) is the commonest major operation carried out in many low income countries. A new technique for CS, called the Misgav Ladach procedure, was evaluated in a randomized trial in Nazareth Hospital (Kiambu District, Kenya). A total of 160 patients were assigned to the Misgav Ladach procedure (n=80) or to the traditional CS as performed in most rural hospitals in low income countries (n=80). The two groups were analyzed by operating time, presence of infection and febrile morbidity, grade of postoperative pain, starting of fluid and solid alimentation, and development of incisional hernia and hypertrophic scar. The operating time of the Misgav Ladach procedure was significantly shorter. 20.4 (SD 6.1) minutes versus 30.4 (SD 6.1) minutes (p< 0.001). A total of 5 wound infections (6.2%) were seen with the Misgav Ladach procedure versus 16 (20.0%) in the control group (p=0.01). The number of analgesic doses required during the postoperative period were significantly less in the Misgav Ladach group: 1.3 (SD 0.6) versus 1.9 (SD 0.7) ampuls of pethidine (p<0.001) and 15.1 (SD 2.0) versus 16.4 (SD 1.8) tablets of ibuprofen (p<0.001). Incisional pain was significantly less in the Misgav Ladach group: Visual Analogue Scale score 3.0 (SD 1.5) versus 4.9 (SD 2.0),p<0.01. The patients in the Misgav Ladach group began drinking fluids voluntarily [19.1 (SD 4.5) hours versus 20.6 (SD 4.0) hours;p=0.01] and eating solid food [41.2 (SD 9.3) hours versus 46.1 (SD 9.0) hours;p<0.01] significantly before than those in the control group. At the 6-week follow-up, the presence of hypertrophic scar was significantly associated with the traditional procedure (2.1% vs. 48.8%;p<0.001). We conclude that the Misgav Ladach operation should become the standard method for performing CS in low income countries, particularly in rural hospitals.
Résumé
La césarienne (CS) est l’intervention majeure la plus fréquemment réalisée dans beaucoup de paysà basse économie. Pour évaluer une nouvelle technique de césarienne, appelé le procédé de «Misgav Ladach», dans une étude randomiséeà l’hôpital Nazareth Hospital (Kiambu District, Kenya), 160 patientes ont été allouées soit au procédé de «Misgav Ladach» (n=80) soità la césarienne traditionnelle CS (n=80), comme réalisée dans la plus grande majorité des hôpitaux ruraux dans les paysà revenu peu élevé. On a analysé la durée de l’opération, la présence d’infection et la morbidité hyperthermique, le degré de la douleur postopératoire, le début de l’alimentation liquidienne et solide, le développement d’une éventration, et la survenue d’une cicatrice hypertrophique. La durée opératoire pour le procédé de «Misgav Ladach» a été significativement plus courte (20.4 (SD=6.1) versus 30.4 (SD=6.1) minutes (p<0.001)). On a noté cinq cas d’infection pariétale (6,2%) dans la technique de Misgav Ladach comparésà 16 cas (20.0%) dans le groupe contrôle (p=0.01). Les patientes dans le groupe Misgav Ladach ont eu besoin de moins de doses d’analgésiques dans la période postopératoire: 1.3 (SD=0.6) versus 1.9 (SD=0.7) ampoules de Péthidine (p<0.001) et 15.1 (SD=2.0) versus 16.4 (SD=1.8) compresses d’ibuprofène (p<0.001). La douleur au niveau de la cicatrice était significativement moindre dans le groupe «Misgav Ladach» avec un scoreà l’échelle visuelle analogue de 3,0 (SD=1.5) versus 4,9 (SD=2.0), p<0.01. De plus, les patients dans le groupe «Misgav Ladach» ont commencéà boire des liquides (19.1, SD=4.5, versus 20.6, SD=4.0 heures, p=0.01) et a mangé des aliments solides (41.2, SD=9.3, versus 46.1, SD=9.0 heures, p<0.01) plus tôt que celles du group de contrôle. A six semaines, il y avait plus de femmes qui avaient une cicatrice hypertrophique dans le groupe de césarienne classique (2.1% versus 48.8%, p<0.001). Nous concluons que le procédé de «Misgav Ladach» devrait être la méthode de référence pour césarienne dans les paysà revenue bas, surtout dans les hôpitaux ruraux.
Resumen
La operación de cesárea (CS) es la intervención más frecuente en paises subdesarrollados. Con objeto evaluar una nueva técnica de CS, denominada Misgaw Ladach, se efectuó un estudio randomizado en el Hospital de Nazareth (distrito de Kiambu, Kenya). Se recopilaron 160 pacientes en las que se realizó la técnica de Misgaw Ladach (n=80) o la CS convencional, como se realiza en la mayoria de los hospitales rurales en los paises en vias de desarrollo (n=80). Ambos grupos se analizaron para valorar el tiempo operatorio, la infección y la morbilidad febril, el grado de dolor postoperatorio, el momento en que se comenzó la ingesta liquida y sólida, el desarrollo de eventraciones y de cicatrización queloidea. El tiempo operatorio con la técnica de Misgaw Ladach es significativamente más cortö 20.4 (SD=6.1) vs 30.4 (SD=6.1) minutos (p<0.001). Con la técnica de Misgaw Ladach se observaron 5 infecciones de la herida operatoria (6.2%) frente a 16 (20%) en el grupo control (p=0.01). El número de dosis analgésicas requeridas por las operadas con la técnica de Misgaw Ladach fue significativamente menor: 1.3 (SD=0.6) vs 1.9 (SD=0.7) ampollas de petidina (p<0.001) y 15.1 (SD=2.0) vs 16.4 (SD=1.8) apósitos de Ibuprofen (p<0.001). El dolor de la herida operatoria fue significativamente menor con la técnica de Misgaw Ladach: En la escala analógica visual alcanzó un grado de 3.0 (SD=1.5) vs 4.9 (SD=2.0), (p<0.01). Además, las pacientes operadas con la técnica de Misgaw Ladach empezaron voluntariamente a beber (19.1, SD=4.5 vs 20.6 SD=4.0 horas, p=0.01) y a ingerir alimentos sólidos (41.2 SD=9.3 vs 46.1 SD=9.0 horas, p<0.01), mucho antes que las del grupo control. Tras un seguimiento de 6 semanas se observaron cicatrices queloideas en el 2.1% de las intervenciones realizadas con la técnica de Misgaw Ladach frente a un 48.8% de las operadas de cesárea con la técnica tradicional (p<0.001). Concluimos senãlando que la técnica de Misgaw Ladach CS debe convertirse en el método estándar para la realización de una cesárea en pueblos económicamente débiles y, especialmente en los hospitales rurales.
Similar content being viewed by others
References
Stark, M.: Technique of caesarean section: the Misgav Ladach method. In Women’s Health Today: Perspectives on Current Research and Clinical Practice, Popkin, D.R., Peddle, L.J., editors, New York, Parthenon, 1994, pp. 81–85
Joel-Cohen, S.: Abdominal and Vaginal Hysterectomy: New Techniques Based on Time and Motion Studies. London, William Heinemann, 1970, p. 170
Stark, M., Finkel, A.R.: Comparison between the Joel-Cohen and Pfannenstiel incisions in caesarean section. Eur. J. Obstet. Gynecol. Reprod. Biol.53:121, 1994
Hauth, J.C., Owen, J., Davis, R.O., Lincoln, T., Piazza, J.: Transverse uterine incision closure: one versus two layers. Am. J. Obstet. Gynecol.166:398, 1992
Pierantoni, M., Parsons, M.T., O’Brien, W.F., Collins, E., Knuppel, R.A., Spellacy, W.N.: Peritoneal closure and non-closure at caesarean. Obstet. Gynecol.77:293, 1991
Hull, D.B., Varner, M.W.: A randomised study of closure of the peritoneum at caesarean delivery. Obstet. Gynecol.77:818, 1991
Duffy, D.M., diZerega, G.S.: Is peritoneal closure necessary? Obstet. Gynecol. Surv.49:817, 1994
Irion, O., Luzuy, F., Beguin, F.: Nonclosure of the visceral and parietal peritoneum at caesarean section: a randomised controlled trial. Br. J. Obstet. Gynaecol.103:690, 1996
Nagele, F., Karas, H., Spitzer, D., Staudach, A., Karasegh, S., Beck, A., Husslein, P.: Closure or nonclosure of the visceral peritoneum at cesarean delivery. Am. J. Obstet. Gynecol.174:1366, 1996
Stark, M., Chavkin, Y., Kupfersztain, C., Guedj, P., Finkel, A.R.: Evaluation of combinations of procedures in cesarean section. Int. J. Gynaecol. Obstet.48:273, 1995
Darj, E., Nordstrom, M.L.: The Misgav Ladach method for cesarean section compared to the Pfannenstiel method. Acta Obstet. Gynecol. Scand.78:37, 1999
Federici, D., Lacelli, B., Muggiasca, L., Agarossi, A., Cipolla, L., Conti, M.: Cesarean section using the Misgav Ladach method. Int. J. Gynaecol. Obstet.57:273, 1997
Stark, M.: Adhesion-free cesarean section [letter to the editor]. World J. Surg.17:419, 1993
Holmgren, G., Sjoholm, L.: The Misgav Ladach method of caesarean section: evolved by Joel-Cohen and Michael Stark in Jerusalem. Trop. Doct.26:150, 1996
Nordberg, E.M.: Incidence and estimated need of caesarean section, inguinal hernia repair, and operation for strangulated hernia in rural Africa. B.M.J.289:92, 1984
Holmberg, S., Nordberg, E.: Surgical rates in Africa: variations and their possible explanations. Trop. Geogr. Med.42:352, 1990
Ameh, E.A., Mbibu, H.N., Adams, L.M., Nmadu, P.T.: Role of a general surgeon in obstetrics and gynaecology in a rural setting. East Afr. Med. J.75:27, 1998
Pereira, C., Bugalho, A., Bergström, S., Vaz, F., Cotiro, M.: A comparative study of caesarean deliveries by assistant medical officers and obstetricians in Mozambique. Br. J. Obstet. Gynaecol.103:508, 1996
Green, S.L., Sarubbi, F.A., Bishop, E.H.: Prophylactic antibiotics in high-risk cesarean section. Obstet. Gynecol.51:569, 1978
McCowan, L., Jackson, P.: The prophylactic use of metronidazole in caesarean section. N.Z. Med. J.92:153, 1980
Reggiori, A., Ravera, M., Cocozza, E., Andreata, M., Mukasa, F.: Randomized study of antibiotic prophylaxis for general and gynaecological surgery from a single centre in rural Africa. Br. J. Surg.83:356, 1996
Guedj, P., Eldor, J., Stark, M.: Immediate postoperative oral hydration after caesarean section. Asia Oceania J. Obstet. Gynaecol.17: 125, 1991
Abd Rabbo, S.: Early oral hydration: a novel regimen for management after elective cesarean section. J. Obstet. Gynaecol.21:563, 1995
Soriano, D., Dulitzki, M., Keidar, N., Barkai, G., Mashiach, S., Seidman, D.S.: Early oral feeding after cesarean delivery. Obstet. Gynecol.87:1006, 1996
Morgan, P.: Spinal anaesthesia in obstetrics. Can. J. Anaesth.42:1145, 1995
Longombe, A., Nyankunde, C.M.E.: Postoperative dressing: are they really necessary? Trop. Doct.20:41, 1990
Cruse, P.J.E.: Wound infections: epidemiology and clinical characteristics. In Surgical Infectious Diseases, Simmons R.L., Howard R.J., editors, Norwalk, CT, Appleton-Century-Crofts, 1982, pp. 429–441
Karl, R.C., Mertz, J.J., Veith, F.J., Dineen, P.: Prophylactic antimicrobial drugs in surgery. N. Engl. J. Med.275:305, 1966
Adeloye, A.: Davey’s Companion to Surgery in Africa. Edinburgh, Churchill Livingstone, 1987, pp. 59–68
Field, C.S.F.: Surgical techniques for cesarean section. Obstet. Gynecol. Clin. North Am.15:657, 1988
Halasz, N.A.: Dehiscence of laparotomy wounds. Am. J. Surg.116: 210, 1968
Mowat, J., Bonnar, J.: Abdominal dehiscence after caesarean section. B.M.J.2:256, 1971
Blomstedt, B., Welin-Berger, T.: Incisional hernias: a comparison between midline, oblique and transrectal incisions. Acta Chir. Scand.138:275, 1972
Tera, H., Åberg, C.: Tissue strength of structures involved in musculoaponeurotic layer sutures in laparotomy incisions. Acta Chir. Scand.142:349, 1976
Biswas, K.K.: Why not Pfannenstiel’s incision? Obstet. Gynecol.41: 303, 1973
Greenall, M.J., Evans, M., Pollock, A.V.: Midline or transverse laparotomy? A random controlled clinical trial. Part I. Influence on healing. Br. J. Surg.67:188, 1980
Ayers, J.W.T., Morley, G.W.: Surgical incision for cesarean section. Obstet. Gynecol.70:706, 1987
Hauth, J.C., Owen, J., Davis, R.O.: Transverse uterine incision closure: one versus two layers. Am. J. Obstet. Gynecol.167:1108, 1992
Tucker, J.M., Hauth, J.C., Hodgkins, P., Owen, J., DuBard, M., Winkler, C.L.: Trial of labor after a one or two layer closure of a low transverse uterine incision. Am. J. Obstet. Gynecol.166:408, 1992
Chapman, S.J., Owen, J., Hauth, J.C.: One- versus two-layer closure of a low transverse cesarean: the next pregnancy. Obstet. Gynecol.89:16, 1997
Jelsema, R.D., Wittingen, J.A., Vander Kolk, K.J.: Continuous, nonlocking, single-layer repair of the low transverse uterine incision. J. Reprod. Med.38:393, 1993
Lal, K., Tsomo, P.: Comparative study of single layer and conventional closure of uterine incision in cesarean section. Int. J. Gynecol. Obstet.27:349, 1988
Ellis, H., Heddle, R.: Does the peritoneum need to be closed at laparotomy? Br. J. Surg.64:733, 1977
Ellis, H., Moran, B.J., Thompson, J.N., Parker, M.C., Wilson, M.S., Menzies, D., McGuire, A., Lower, A.M., Hawthorn, R.J.S., O’Brien, F., Buchan, S., Crowe, A.M.: Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet353:1476, 1999
Hubbard, T.B., Khan, M.Z., Carag, V.R., Albites, V.E., Hricko, G.M.: The pathology of peritoneal repair: its relation to the formation of adhesions. Ann. Surg.165:908, 1967
Holmdahl, L.: The role of fibrinolysis in adhesion formation. Eur. J. Surg.163(Suppl. 577):24, 1997
Raferty, A.T.: Regeneration of parietal and visceral peritoneum: a light microscopical study. Br. J. Surg.60:293, 1973
DiZerega, G.S.: Biochemical events in peritoneal tissue repair. Eur. J. Surg.163(Suppl. 577):10, 1997
Ellis, H.: The aetiology of post-operative abdominal adhesions: an experimental study. Br. J. Surg.50:10, 1962
Thompson, J.N., Paterson-Brown, S., Harbourne, T., Whawell, S.A., Kalodiki, E., Dudley, H.A.F.: Reduced human peritoneal plasminogen activating activity: possible mechanism of adhesion formation. Br. J. Surg.76:382, 1989
Vipond, M.N., Whawell, S.A., Thompson, J.N., Dudley, H.A.F.: Peritoneal fibrinolytic activity and intra-abdominal adhesions. Lancet335: 1120, 1990
Connoly, W.B., Stephens, F.O.: Factors influencing the incidence of intraperitoneal adhesions: an experimental study. Surgery63:976, 1968
Raferty, A.T.: Effect of peritoneal trauma on peritoneal fibrinolytic activity and intraperitoneal adhesion formation: an experimental study in the rat. Eur. Surg. Res.13:397, 1981
Elkins, T.E., Stovall, T.G., Warren, J., Ling, F.W., Meyer, N.L.: A histologic evaluation of peritoneal injury and repair: implications for adhesion formation. Obstet. Gynecol.70:225, 1987
McDonald, M.N., Elkins, T.E., Wortham, G.F., Stovall, T.G., Ling, F.W., McNeeley, S.G.: Adhesion formation and prevention after peritoneal injury and repair in the rabbit. J. Reprod. Med.33:436, 1988
Tulandi, T., Hum, H.S., Gelfand, M.M.: Closure of laparotomy incisions with or without peritoneal suturing and second-look laparoscopy. Am. J. Obstet. Gynecol.158:536, 1988
McCurdy, C.M., Magann, E.F., McCurdy, C.J., Saltzman, A.K.: The effect of placental management at cesarean delivery on operative blood loss. Am. J. Obstet. Gynecol.167:1363, 1992
Magann, E.F., Washburne, J.F., Harris, R.L., Bass, J.D., Duff, W.P., Morrison, J.C.: Infectious morbidity, operative blood loss, and length of the operative procedure after cesarean delivery by method of placental removal and site of uterine repair. J. Am. Coll. Surg.181: 517, 1995
Atkinson, M.W., Owen, J., Wren, A., Hauth, J.C.: The effect of manual removal of the placenta on post-cesarean endometritis. Obstet. Gynecol.87:99, 1996
Magann, E.F., Dodson, M.K., Allbert, J.R., McCurdy, C.M., Martin, R.W., Morrison, J.C.: Blood loss at time of cesarean section by method of placental removal and exteriorization versus in situ repair of uterine incision. Surg. Gynecol. Obstet.177:389, 1993
Hershey, D.W., Quilligan, E.J.: Extraabdominal uterine exteriorization at cesarean section. Obstet. Gynecol.52:189, 1978
Baker, E.R., D’Alton, M.E.: Cesarean section birth and cesarean hysterectomy. Clin. Obstet. Gynecol.37:806, 1994
Down, R.H., Whitehead, R., Watts, J.M.: Do surgical packs cause peritoneal adhesions? Aust. N.Z.J. Surg.49:379, 1979
Thadepalli, H., Bach, V.T., Davidson, E.: Antimicrobial effect of amniotic fluid. Obstet. Gynecol.52:198, 1978
Larsen, B., Davis, B., Charles, D.: Critical assessment of antibacterial properties of human amniotic fluid. Gynecol. Obstet. Invest.18:100, 1984
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansaloni, L., Brundisini, R., Morino, G. et al. Prospective, randomized, comparative study of Misgav Ladach versus traditional cesarean section at Nazareth Hospital, Kenya. World J. Surg. 25, 1164–1172 (2001). https://doi.org/10.1007/BF03215866
Issue Date:
DOI: https://doi.org/10.1007/BF03215866