Summary
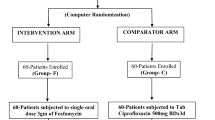
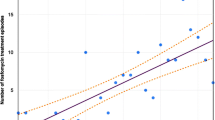
A five day course of calvulanate-potentiated amoxicillin (Augmentin®) has been compared with a single oral dose of fosfomycin trometamol in the treatment of patients complaining of symptoms suggesting urinary tract infection. The study took place in a single urban general practice of 15,000 patients in Cheshire. The microbiology was performed at a London Teaching Hospital. 141 patients entered the trial. 65 had a significant bacteriuria, 62 of which were assessable for the ability of the trial drugs to eradicate bacteriuria: 29 patients received clavulanate-potentiated amoxicillin and 33 fosfomycin trometamol. The cure rates, assessed at five to ten days and at four to six weeks post treatment, were 72% and 65%, respectively for clavulanate-potentiated amoxicillin and 85% and 81%, respectively for fosfomycin trometamol. Side effects, assessed in all 141 patients, occurred in 11.6% receiving clavulanate-potentiated amoxicillin and in 8.3% receiving fosfomycin. Statistically there is no difference between any of these findings and the effect of sample size is discussed. 69 patients were symptomatic but did not have a significant bacteriuria (“urethral syndrome”). These patients were assessed for the effect of treatment in relieving symptoms: 33 received fosfomycin trometamol and 36 clavulanate-potentiated amoxicillin. The success and speed of relieving the symptoms were very similar in the two groups. The finding that both groups responded equally well appears to refute an aetiological role for lactobacilli and diphtheroids in the “urethral syndrome”, since these organisms are resistant to fosfomycin but sensitive to clavulanate-potentiated amoxicillin.
Zusammenfassung
Patienten, die Beschwerden einer Harnwegsinfektion hatten, wurden entweder fünf Tage lang mit Amoxicillin-Clavulansäure (Augmentan®) oder mit einer oralen Einzeldosis von Fosfomycin Trometamol behandelt. Die Studie wurde in einer Allgemeinpraxis in Cheshire durchgeführt, die 15 000 Patienten versorgt. 141 Patienten wurden in die Studie aufgenommen. 65 hatten eine signifikante Bakteriurie, davon konnten 62 in die Auswertung bezüglich Eradikation der Bakteriurie durch das Prüfmedikament einbezogen werden; 29 Patienten erhielten Amoxicillin-Clavulansäure und 33 Fosfomycin Trometamol. In der ersten Gruppe waren am 5.–10. Tag und vier bis sechs Wochen nach Therapieende 72% beziehungsweise 65% geheilt, die entsprechenden Zahlen für Fosfomycin Trometamol waren 85% und 81%. Bei 11,6% der insgesamt ausgewerteten 141 Patienten traten Nebenwirkungen unter Amoxicillin-Clavulansäure und bei 8,3% unter Fosfomycin Trometamol auf. Ein statistischer Unterschied zwischen diesen Befunden besteht nicht, die Bedeutung der Probengröße hierfür wird diskutiert. 69 Patienten klagten über Beschwerden, hatten jedoch keine signifikante Bakteriurie (urethrales Syndrom). Sie wurden im Hinblick auf eine Linderung ihrer Beschwerden durch Fosfomycin Trometamol (n=33) oder Amoxicillin-Clavulansäure (n=36) geprüft. In beiden Gruppen war der Einfluß auf die Beschwerden nach Grad und Geschwindigkeit sehr ähnlich. Das vergleichbar gute Ansprechen der beiden Gruppen scheint gegen eine ätiologische Bedeutung von Laktobazillen und Diphtheroiden beim „urethralen Syndrom“ zu sprechen, denn diese Bakterien sind gegen Fosfomycin Trometamol resistent, gegen Amoxicillin-Clavulansäure hingegen empfindlich.
Similar content being viewed by others
References
Waters, W. E. Prevalence of symptoms of urinary tract infection in women. Br. J. Prevent. Soc. Med. 23 (1969) 263–266.
Brooks, D.: A general practitioner's view of the laboratory examination of urine. In:Meers, P. D. (ed.): The bacteriological examination of urine: report of a workshop on needs and methods. HMSO-London 1978, pp. 39–40.
Walker, M., Heady, J. A., Shaper, A. G. The prevalence of dysuria in women in London. J. R. Coll. Gen. Practit. 33 (1983) 411–415.
Charlton, C. A. C., Crowther, A., Davies, J. G., Dynes, J., Howard, M. R. A., Mann, P. G., Rye, S. Three day and ten day chemotherapy for urinary tract infections in general practice. Br. Med. J. i (1976) 124–126.
Gruneberg, R. N., Brumfitt, W. Single dose treatment of acute urinary tract infection: a controlled trial. Br. Med. J. iii (1967) 649–651.
Bailey, R. R. (ed.): Single dose therapy of urinary tract infection. Adis Press, Sydney 1983.
Brumfitt, W., Hamilton-Miller, J. M. T. Single dose antibiotic therapy in urinary tract infections. In:Andreucci, V. E. (ed.): International Yearbook of Nephrology 1989. Kluwer, Massachusetts 1989, pp. 49–63.
ABPI Data Sheet Compendium 1988–89: Datapharm Publications, London 1988.
Ferrari, V., Bonanomi, L., Borcia, M., Lodola, E., Marca, G.: A new fosfomycin derivative with much improved bioavailability by oral route. Chemother. Antimicrob. iv (1981) 59–63.
Gallego, A., Rodriguez, A., Mata, J. M. Fosfomycin: pharmacological studies. Drugs of Today 10 (1974) 161–168.
Maskell, R.: Are fastidious organisim an important cause of dysuria and frequency? — the case for. In:Asscher, A. W., Brumfitt, W. (eds.): Microbial diseases in nephrology. Wiley, Chichester 1986, pp. 1–18.
Kunin, C. M. Foreword. In:Bailey, R. R. (ed.): Single dose therapy of urinary tract infection. Adis Press, Sydney 1983, pp. viii-x.
Brumfitt, W., Hamilton-Miller, J. M. T. The optimal duration of antibiotic treatment of urinary infections. In:Neu, H. C., Williams, J. D. (eds.): New trends in urinary tract infections. Karger, Basel 1988, pp. 62–77.
Loulerque, J., Pinon, G., Laudat, P., Audurier, A. La résistance a la fosfomycine chezStaphylococcus saprophyticus et chez les autres espèces de stapylococcus coagulase negative. Ann. Microbiol. (Institut Pasteur) 135A (1984) 239–247.
Stamboulian, D., Sarachian, B., Arguelllo, E., Belforte, B. Evaluation of amoxicillin with and without BRL 14151 in the treatment of urinary tract infections. In:Nelson, J. D., Grassi, C. (eds.): Current Chemotherapy and Infectious Diseases. American Society of Medicine-Washington 1980, pp. 338–340.
Nishiura, T. Efficacy of Augmentin (BRL 25 000) in urinary tract infections. In:Leigh, D. A., Robinson, O. P. W. (eds.): Augmentin: clavulanate-potentiated amoxicillin. Excerpta Medica, Amsterdam 1982, pp. 65–77.
Gurwith, M. J., Stein, G. E., Gurwith, D. Prospective comparison of amoxicillin-clavulanic acid and cefaclor in treatment of uncomplicated urinary tract infections. Antimicrob. Agents Chemother. 24 (1983) 716–719.
Karachalios, G. N., Georgiopoulos, A. N. Treatment of acute urinary tract infections with amoxicillin and clavulanic acid combination. IRCS Med. Sci. 12 (1984) 1042–1043.
Iravani, A., Richard, G. A. Treatment of urinary infections with a combination of amoxicillin and clavulanic acid. Antimicrob. Agents Chemother. 22 (1982) 672–677.
Cooper, J., Brumfitt, W., Hamilton-Miller, J. M. T. A comparative trial of co-trimoxazole and cephradine in patients with recurrent urinary infections. J. Antimicrob. Chemother. 6 (1980) 231–239.
The Urinary Tract Infection Study Group Coordinated multicenter study of norfloxacin versus trimethoprim-sulphamethoxazole treatment of symptomatic urinary tract infections. J. Infect. Dis. 155 (1987) 170–177.
Silverblatt, F. J. Clinical trials and statistical rigor — are the benefits necessarily worth the cost? J. Infect. Dis. 155 (1987) 168–169.
Stamm, W. E., Wagner, K. F., Amsel, R., Alexander, E. R., Turck, M., Counts, G. W., Holmes, K. K. Causes of the acute urethral syndrome in women. New Engl. J. Med. 303 (1980) 409–415.
O'Dowd, T. C., Pill, R., Smail, J. E., Davis, R. H. Irritable urethral syndrome: follow-up study in general practice. Br. Med. J. 292 (1986) 30–32.
Brumfitt, W., Hamilton-Miller, J. M. T., Smith, G. W. Comparative trial of cefuroxime axetil in recurrent urinary tract infections, illustrating importance of 6-week follow-up. Antimicrob. Agents Chemother. 31 (1987) 1442–1443.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cooper, J., Raeburn, A., Brumfitt, W. et al. Single dose and conventional treatment for acute bacterial and non-bacterial dysuria and frequency in general practice. Infection 18, 65–69 (1990). https://doi.org/10.1007/BF01641417
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/BF01641417