Abstract
Congenital heart disease (CHD) affects almost one in 100 newborn babies worldwide (Hoffman). The continuous advances and availability of noninvasive cardiac imaging has revolutionised the management of these cases, allowing various methods to complement one another. To have a better understanding of the varied and oftencomplex cardiac and extra-cardiac anatomy in patients with CHD, additional imaging may be required as a supplement to more traditional firstline modalities such as echocardiography (ECHO).
Similar content being viewed by others
INTRODUCTION
Congenital heart disease (CHD) affects almost one in 100 newborn babies worldwide (Hoffman). The continuous advances and availability of noninvasive cardiac imaging has revolutionised the management of these cases, allowing various methods to complement one another. To have a better understanding of the varied and oftencomplex cardiac and extra-cardiac anatomy in patients with CHD, additional imaging may be required as a supplement to more traditional firstline modalities such as echocardiography (ECHO). In this report we present a case of an infant with a diagnosis of DiGeorge Syndrome, and tetralogy of fallot (TOF) with severe pulmonary stenosis and complex major aorto-pulmonary collateral arteries (MAPCAs). We will also outline the various roles of imaging modalities used in the management of this child, focusing on the complementary role of Multi-Detector Computed Tomography (MDCT).
Case Report
A 5-month-old female with DiGeorge Syndrome, and TOF with near pulmonary atresia, presented with repeated episodes of collapse and severe respiratory distress. She was born at term via a non-complicated spontaneous vaginal delivery. The diagnosis of TOF was made antenatally and karyotyping confirmed a 22q11 deletion (DiGeorge) genetic abnormality.
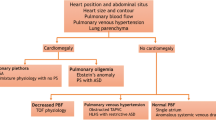
On admission to our institution, she had symptoms of respiratory distress. Her parents reported a twoday history of coryzal symptoms. On examination she was cyanosed, with an arterial oxygen saturation of 50%. She was transferred to the Pediatric Intensive Care Unit (PICU). Chest x-ray showed right upper lobe consolidation, consistent with a lobar pneumonia, and antibiotic therapy was subsequently commenced. The chest x-ray clearly illustrated a right-sided aortic arch, pulmonary artery bay, elevated cardiac apex typical of right ventricular enlargement, but an otherwise normal cardiac silhouette (Figure 1). ECHO showed a large (8mm) perimembranous VSD with a pure right-to-left shunt, an overriding aorta with a right-sided arch, and several collateral branches from the descending aorta to the pulmonary arteries (MAPCAs). The branch pulmonary arteries (PA) were difficult to visualise. A closed Ductus Arteriosus was identified, and there was no coarctation of the aorta. There was a small patent foramen ovale with a predominantly left-to-right shunt. The right ventricle was dilated, with trivial tricuspid regurgitation. Both ventricles displayed good systolic function. A CT angiogram (Siemens, Flash Dual Source, Germany) with iopromide (Ultravist©) contrast was utilised to determine the pulmonary arteries and the MAPCAs more accurately (Figure 2). The patient then successfully underwent surgery to establish antegrade connection between her right ventricle and pulmonary arteries
A CT angiogram of the patient demonstrating a right-sided aorta and MAPCAs (left) and a 3D reconstruction of the CT examination (right). A MAPCA arises from the left side of the aorta, loops superiorly then inferiorly and supplies the left upper lobe (solid white oval); Two MAPCAs arise from the right side of the aorta and supply parts of the right middle and lower lobes (dotted oval).
With the continuous advancement in imaging modalities, clinicians have at their disposal a number of reliable imaging modes for diagnosis.
This is especially true in the setting of congenital heart disease. Since the advent of cardiac catheterisation and echocardiography in the 1960s and 1980s respectively, several other imaging tools have emerged, including Magnetic Resonance Imaging (MRI) and CT angiography. And while each have their own advantages, they also come with their respective shortcomings, which should be taken into account, and minimised. This may include using a combination of imaging methods to complement one another.
With its convenience of use, well-established echocardiographic-morphological correlations, and non-invasive nature, ECHO is always the first-line diagnostic investigation in patients with suspected CHD (2). The additional Doppler techniques (Figure 3), which allowed visualisation and flow velocity quantification, have enhanced the diagnostic accuracy of the ECHO (3). As outlined in our case report above, much of the anatomical and physiological detail could be determined using ECHO. Currently a significant number of CHD cases are referred directly for interventions based chiefly on an echocardiographic diagnosis only (4). While ECHO remains as the most widely used imaging technique in the diagnosis of CHD, it does have its limitations, particularly in complex congenital anomalies involving extracardiac structures, such as small central pulmonary arteries, peripheral pulmonary arteries, the cervical vessels and pulmonary veins (2, 4). This case demonstrates the difficulties in determining the detailed anatomy of hypoplastic central pulmonary arteries and the size, number and distribution of MAPCAs by echocardiography.
Given the limitations of echocardiographic diagnosis in certain CHD cases, other imaging modality may be needed to provide additional information. Cardiac MRI is the gold standard technique for depicting aortic anomalies and relevant collateral vessels (5). Furthermore, the ability of MRI to assess volume and mass of peculiar ventricular shapes, which may be a feature of CHD, with optimal accuracy, is especially desirable (6). Compared to other imaging modalities such as cardiac catheterisation and CT, MRI studies do not involve exposure to ionising radiation. As such, accepted pediatric indications for cardiac MRI include: segmental depiction of cardiac morphology, detailed evaluation of aortic and other major vessel and systemic venous anomalies, quantification of shunts, stenoses, and regurgitation, and post-operative study (6-9). However, certain drawbacks do limit the utilisation of MRI. Study time is a key limitation for MRI, with a typical congenital cardiac study using a 1.5 T magnet requiring 45-60 min (10). And while this is less of an issue with adult patients, children may require sedation, or general anaesthesiae, which may confer additional risks (11). Furthermore, there are technical barriers to sequence optimisation in the use of MRI particularly in the young paediatric age group; which include: fast heart rate requiring high temporal resolution for optimal ventricular volume and flow assessments, and small cardiac size and vessels which require great spatial resolution (12). Another potential challenge that one should keep in mind is the resuscitation of a critically ill patient in the confines of the magnet, which require removal of the patient from the scanning room (13). Although diagnostic cardiac catheterisation with selective angiography in each MAPCA provides precise diagnostic information, it also carries a significant risk (14). Thus, given the young age and clinical state of our patient, we felt that although MRI and cardiac catheterisation would have provided an accurate anatomical depiction, the benefits did not justify the potential risks, and CT was a more suitable imaging option.
Given the limitations of echocardiographic diagnosis in certain CHD cases, other imaging modality may be needed to provide additional information. Cardiac MRI is the gold standard technique for depicting aortic anomalies and relevant collateral vessels (5). Furthermore, the ability of MRI to assess volume and mass of peculiar ventricular shapes, which may be a feature of CHD, with optimal accuracy, is especially desirable (6). Compared to other imaging modalities such as cardiac catheterisation and CT, MRI studies do not involve exposure to ionising radiation. As such, accepted pediatric indications for cardiac MRI include: segmental depiction of cardiac morphology, detailed evaluation of aortic and other major vessel and systemic venous anomalies, quantification of shunts, stenoses, and regurgitation, and post-operative study (6-9). However, certain drawbacks do limit the utilisation of MRI. Study time is a key limitation for MRI, with a typical congenital cardiac study using a 1.5 T magnet requiring 45-60 min (10). And while this is less of an issue with adult patients, children may require sedation, or general anaesthesiae, which may confer additional risks (11). Furthermore, there are technical barriers to sequence optimisation in the use of MRI particularly in the young paediatric age group; which include: fast heart rate requiring high temporal resolution for optimal ventricular volume and flow assessments, and small cardiac size and vessels which require great spatial resolution (12). Another potential challenge that one should keep in mind is the resuscitation of a critically ill patient in the confines of the magnet, which require removal of the patient from the scanning room (13). Although diagnostic cardiac catheterisation with selective angiography in each MAPCA provides precise diagnostic information, it also carries a significant risk (14). Thus, given the young age and clinical state of our patient, we felt that although MRI and cardiac catheterisation would have provided an accurate anatomical depiction, the benefits did not justify the potential risks, and CT was a more suitable imaging option.
The development of CT technology, with the multidetector scanners and 16-, 32-, 64- and 128-detector technology has allowed extremely fast image acquisition (10 ± 2s) without significant compromise to image quality (4, 10). It provides high spatial resolution and detailed 3D reconstruction of extra-cardiac anatomical structures, such as pulmonary vessels e.g. pulmonary sling (Figure 4), aortic arch anomalies e.g. right-sided aortic arch (Figure 5), and coronary arteries (15-16). In addition to its minimal invasiveness, MDCT has also been shown to be more superior than conventional cardiac catheterization in delineating MAPCAs, in particular for identifying segmental pulmonary blood flow (17). The difficulties in precise diagnosis of right-sided heart anomalies potentially can be overcome by CT (2). The short acquisition times of CT are advantageous over MRI since it effectively provides a means for accurate, detailed imaging without the need for sedation or general anaesthesia in paediatric patients (10), even for small infants. Nevertheless, the benefits of CT need to be weighed up against the associated exposure to ionizing radiation and contrast agents. The risk of cancer associated with radiation exposure needs to be considered, especially in children, who are at greater risk given they are inherently more radiosensitive (18). This may be minimised by adjusting the dose for the child’s weight to target the minimum possible radiation exposure, while maintaining diagnostic image quality (19).
Conclusion
With the increasing number of imaging modalities available in the practice of paediatric cardiology, clinicians need to be familiar with the benefits and limitations of each technique, and always consider the options to complement, or substitute, one tool with another, to provide optimal patient management.
References
Hoffman JIE & Kaplan S. The incidence of Congenital heart disease. J Am Coll Cardiol 2002; 39: 1890–1900.
Gilkeson RC, Ciancibello L & Zahka K. Multidetector CT evaluation of congenital heart disease in pediatric and adult patients. AJR; 2003: 973–980.
Ascah KJ, Stewart WJ, Jiang L et al. A Doppler-twodimensional echocardiographic method for quantitation of mitral regurgitation. Circulation 1985; 72: 377–383.
Mertens L, Ganame J & Eyskens B. What is new in pediatric cardiac imaging? Eur J Pediatr 2008; 167: 1–8.
Julsrud PR, Breen JF, Felmlee JP, Warner CA, Connolly HM, Schaff HV. Coarctation of the aorta: collateral flow assessment with phase-contrast MR angiography. AJR 1997; 169: 1735–1742.
Weinberg PM, Fogel MA. Cardiac MR imaging in congenital heart disease. Cardiol Clin 1998; 16(2): 315–348.
Geva T, Sahn DJ, Powell AJ. Magnetic resonance imaging of congenital heart disease in adults. Prog Pediatr Cardiol 2003; 17: 21–39.
Didier D, et al. Morphologic and functional evaluation of congenital heart disease by magnetic resonance imaging. JMRI 1999; 10: 639–655.
Manning WJ, Pennell DJ. Cardiovascular Magnetic Resonance. New York: Churchill Livingstone/Elsevier Science, 2002.
Samyn MM. A review of the complementary information available with cardiac magnetic resonance imaging and multi-slice computed tomography (CT) during the study of congenital heart disease. Int J Cardiovasc Imaging 2004; 20: 569–578.
Girshin M, Shapiro V, Rhee A, Ginsberg S, Inchiosa MA. Increased risk of general anesthesia for high-risk patients undergoing MRI. Journal of Computer Assisted Tomography 2009; 33(2): 312–315.
Bailliard F, et al. Introduction to cardiac imaging in infants and children: Techniques, potential, and role in the imaging work-up of various cardiac malformations and other pediatric heart conditions. Eur J Radiol 2008; 68: 191–8.
Odegard KC, et al. Anaesthesia considerations for cardiac MRI in infants and small children. Pediatr Anesthes 2004; 14: 471–476.
Kennedy JW. Complications associated with cardiac catheterization and angiography. Catheter Cardio Diag 1982; 8: 5–11.
Lambert V, Sigal-Cinqualbre A, Belli E, et al. Preoperative and postoperative evaluation of airways compression in pediatric patients with 3-dimensional multislice computed tomographic scanning: effect on surgical management. J Thorac Cardiovasc Surg 2005; 129: 1111–1118.
Ley S, Zaporozhan J, Arnold R, Eichhorn J, Schenk JP, Ulmer H, Kreitner KF, Kauczor HU. Preoperative assessment and follow-up of congenital abnormalities of the pulmonary arteries using CT and MRI. Eur Radiol 2007; 17: 151–162.
Toole B, et al. Comparison of cardiac catheterization vs computed tomography angiography in evaluating MAPCA in children with pulmonary atresia and ventricular septal defect. J Am Coll Cardiol 2012; 5–9.
Brenner DJ & Hall EJ. Computed Tomography - An Increasing Source of Radiation Exposure. NEJM 2007; 357: 2277–84.
Kim JE & Newman B. Evaluation of a radiation dose reduction strategy for pediatric chest CT. AJR 2010; 194: 1188–1193.
Author information
Authors and Affiliations
Corresponding author
Additional information
Open Access:
This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Listijono, D., Rubens, M. & Rigby, M. Complementary Use of Imaging modalities in Diagnosis of Complex Congenital Heart Disease. Asean Heart J 22, 10 (2014). https://doi.org/10.7603/s40602-014-0010-4
Published:
DOI: https://doi.org/10.7603/s40602-014-0010-4