Abstract
Background
Patient-reported outcomes (PROs) have become a focus in postoperative surgical care. Unfortunately, studies using PROs can be subject to missing data, which may lead to biases or inaccurate conclusions. Multiple imputation (MI) is a statistical method for addressing missing data in clinical research. The aim of this study was to explore MI as a way to address missing data in PRO research.
Methods
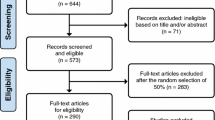
A working example of MI using real-world data was performed using the BREAST-Q PRO measure in postmastectomy reconstruction. A retrospective review of immediate tissue expander breast reconstruction patients in 2019 was conducted to compare BREAST-Q physical well-being of the chest scores between prepectoral and subpectoral cohorts at 2 weeks postoperatively. The observed dataset and three hypothetical missingness situations were created to assess how increasing missingness affects MI results.
Results
Overall, 916 patients were included in the analysis. When excluding patients with missing information and solely performing analysis on the completed cases, prepectoral patients had significantly higher physical well-being of the chest scores at 2 weeks postoperatively; however, this trend was reversed with increasing missingness scenarios, where subpectoral patients had higher scores. In comparison, all MI results showed that prepectoral patients had higher scores on average compared with subpectoral patients regardless of missingness scenario.
Conclusions
MI demonstrated consistent results with increasing missingness scenarios, whereas performing analysis in higher missingness scenarios without MI led to varying results. This working example emphasizes the need for missing data methodology to be considered in PRO research.


Similar content being viewed by others
References
Biering K, Hjollund NH, Frydenberg M. Using multiple imputation to deal with missing data and attrition in longitudinal studies with repeated measures of patient-reported outcomes. Clin Epidemiol. 2015;7:91–106.
Cano SJ, Klassen AF, Scott AM, Pusic AL. A closer look at the BREAST-Q(©). Clin Plast Surg. 2013;40:287–96.
Fuzesi S, Cano SJ, Klassen AF, Atisha D, Pusic AL. Validation of the electronic version of the BREAST-Q in the army of women study. Breast. 2017;33:44–9.
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–53.
Seth I, Seth N, Bulloch G, Rozen WM, Hunter-Smith DJ. Systematic review of breast-Q: a tool to evaluate post-mastectomy breast reconstruction. Breast Cancer (Dove Med Press). 2021;13:711–24.
Nelson JA, Allen RJ Jr, Polanco T, et al. Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg. 2019;270:473–83.
Cohen WA, Mundy LR, Ballard TN, et al. The BREAST-Q in surgical research: a review of the literature 2009–2015. J Plast Reconstr Aesthet Surg. 2016;69:149–62.
Hardouin JB, Conroy R, Sébille V. Imputation by the mean score should be avoided when validating a patient reported outcomes questionnaire by a Rasch model in presence of informative missing data. BMC Med Res Methodol. 2011;11:105.
Ayilara OF, Zhang L, Sajobi TT, Sawatzky R, Bohm E, Lix LM. Impact of missing data on bias and precision when estimating change in patient-reported outcomes from a clinical registry. Health Qual Life Outcomes. 2019;17:106.
Little RJ, Rubin DB. Bayes and multiple imputation. In: RJ Little, DB Rubin, editors. Statistical analysis with missing data. John Wiley & Sons; 2002. p. 200–20.
Donders AR, van der Heijden GJ, Stijnen T, Moons KG. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59:1087–91.
Austin PC, White IR, Lee DS, van Buuren S. Missing data in clinical research: a tutorial on multiple imputation. Can J Cardiol. 2021;37:1322–31.
Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393.
Rubin DB. Multiple Imputation for Nonresponse in Surveys: John Wiley & Sons;1987.
Jakobsen JC, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials—a practical guide with flowcharts. BMC Med Res Methodol. 2017;17:162.
Sun, S., Luo, N., Stenberg, E., et al. Sequential Multiple Imputation for Real-World Health-Related Quality of Life Missing Data after Bariatric Surgery. Int J Environ Res Public Health 2022;19.
Erbes CR, Ferguson J, Yang K, et al. Amputation-specific and generic correlates of participation among Veterans with lower limb amputation. PLoS ONE. 2022;17:e0270753.
Lee PT, Krecko LK, Savage S, et al. Which hospital-acquired conditions matter the most in trauma? An evidence-based approach for prioritizing trauma program improvement. J Trauma Acute Care Surg. 2022;93:446–52.
Cole SR, Chu H, Greenland S. Multiple-imputation for measurement-error correction. Int J Epidemiol. 2006;35:1074–81.
Author information
Authors and Affiliations
Contributions
JAN had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. KH and CS contributed equally to this manuscript. Conceptualization: KH, CS, JAN. Data curation: KH, CS, MGS, LB. Formal analysis: KH, CS, MGS, LB. Methodology: KH, CS, MGS, LB, FDG. Supervision: CS, JAN, FDG. Writing—original draft: KH, CS, FDG, MGS, LB. Writing—reviewing and editing: All authors.
Corresponding author
Ethics declarations
Disclosures
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748, which supports Memorial Sloan Kettering Cancer Center’s research infrastructure. This study received Institutional Review Board approval from Memorial Sloan Kettering Cancer Center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haglich, K., Stern, C., Graziano, F.D. et al. Missing Data in Patient-Reported Outcomes Research: Utilizing Multiple Imputation to Address an Unavoidable Problem. Ann Surg Oncol 30, 8074–8082 (2023). https://doi.org/10.1245/s10434-023-14345-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14345-y