Abstract
Background
Limited evidence exists for the safety and oncologic efficacy of minimally invasive surgery (MIS) for nonfunctioning pancreatic neuroendocrine tumors (NF-PNETs) according to tumor location. This study aimed to compare the surgical outcomes of MIS and open surgery (OS) for right- or left-sided NF-PNETs.
Methods
The study collected data on patients who underwent surgical resection (pancreatoduodenectomy, distal/total/central pancreatectomy, duodenum-preserving pancreas head resection, or enucleation) of a localized NF-PNET between January 2000 and July 2017 at 14 institutions. The inverse probability of treatment-weighting method with propensity scores was used for analysis.
Results
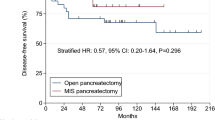
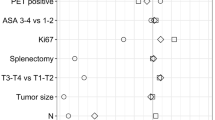
The study enrolled 859 patients: 478 OS and 381 MIS patients. A matched analysis by tumor location showed no differences in resection margin, intraoperative blood loss, or complications between MIS and OS. However, MIS was associated with a longer operation time for right-sided tumors (393.3 vs 316.7 min; P < 0.001) and a shorter postoperative hospital stay for left-sided tumors (8.9 vs 12.9 days; P < 0.01). The MIS group was associated with significantly higher survival rates than the OS group for right- and left-sided tumors, but survival did not differ for the patients divided by tumor grade and location. Multivariable analysis showed that MIS did not affect survival for any tumor location.
Conclusion
The short-term outcomes offered by MIS were comparable with those of OS except for a longer operation time for right-sided NF-PNETs. The oncologic outcomes were not compromised by MIS regardless of tumor location or grade. These findings suggest that MIS can be performed safely for selected patients with localized NF-PNETs.


Similar content being viewed by others
References
Halfdanarson TR, Rubin J, Farnell MB, Grant CS, Petersen GM. Pancreatic endocrine neoplasms: epidemiology and prognosis of pancreatic endocrine tumors. Endocr Relat Cancer. 2008;15:409–27.
Cloyd JM, Poultsides GA. Non-functional neuroendocrine tumors of the pancreas: advances in diagnosis and management. World J Gastroenterol. 2015;21:9512–25.
Fendrich V, Waldmann J, Bartsch DK, Langer P. Surgical management of pancreatic endocrine tumors. Nat Rev Clin Oncol. 2009;6:419–28.
Drymousis P, Raptis DA, Spalding D, et al. Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. HPB Oxf. 2014;16:397–406.
Han SH, Han IW, Heo JS, et al. Laparoscopic versus open distal pancreatectomy for nonfunctioning pancreatic neuroendocrine tumors: a large single-center study. Surg Endosc. 2018;32:443–9.
Kim H, Song KB, Hwang DW, Lee JH, Alshammary S, Kim SC. Laparoscopic versus open pancreaticoduodenectomy for pancreatic neuroendocrine tumors: a single-center experience. Surg Endosc. 2019;33:4177–85.
Tamburrino D, Partelli S, Renzi C, et al. Systematic review and meta-analysis on laparoscopic pancreatic resections for neuroendocrine neoplasms (PNENs). Expert Rev Gastroenterol Hepatol. 2017;11:65–73.
Tian F, Hong XF, Wu WM, et al. Propensity score-matched analysis of robotic versus open surgical enucleation for small pancreatic neuroendocrine tumours. Br J Surg. 2016;103:1358–64.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Bosman F, Hruban R, Theise N. WHO classification of tumours of the digestive system, 4th ed. International Agency for Research on Cancer, Lyon, 2010.
Shim JH, Yoon DL, Han S, et al. Is serum alpha-fetoprotein useful for predicting recurrence and mortality specific to hepatocellular carcinoma after hepatectomy? A test based on propensity scores and competing risks analysis. Ann Surg Oncol. 2012;19:3687–96.
Vaughan AS, Kelley CF, Luisi N, del Rio C, Sullivan PS, Rosenberg ES. An application of propensity score-weighting to quantify the causal effect of rectal sexually transmitted infections on incident HIV among men who have sex with men. BMC Med Res Methodol. 2015;15:25.
Elze MC, Gregson J, Baber U, et al. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol. 2017;69:345–57.
Harrell FE Jr, Califf RM, Pryor DB, Lee KL, Rosati RA. Evaluating the yield of medical tests. JAMA. 1982;247:2543–6.
Heagerty PJ, Zheng Y. Survival model predictive accuracy and ROC curves. Biometrics. 2005;61:92–105.
Keutgen XM, Nilubol N, Glanville J, et al. Resection of primary tumor site is associated with prolonged survival in metastatic nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2016;159:311–8.
Nigri GR, Rosman AS, Petrucciani N, et al. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc. 2011;25:1642–51.
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg. 2012;255:1048–59.
Zhang XF, Lopez-Aguiar AG, Poultsides G, et al. Minimally invasive versus open distal pancreatectomy for pancreatic neuroendocrine tumors: an analysis from the U.S. neuroendocrine tumor study group. J Surg Oncol. 2019;120:231–40.
Hernan MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–70.
Curtis LH, Hammill BG, Eisenstein EL, Kramer JM, Anstrom KJ. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45:S103–7.
Ennis RD, Hu L, Ryemon SN, Lin J, Mazumdar M. Brachytherapy-based radiotherapy and radical prostatectomy are associated with similar survival in high-risk localized prostate cancer. J Clin Oncol. 2018;36:1192–8.
Weintraub WS, Grau-Sepulveda MV, Weiss JM, et al. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467–76.
Song KB, Kim SC, Lee W, et al. Laparoscopic pancreaticoduodenectomy for periampullary tumors: lessons learned from 500 consecutive patients in a single center. Surg Endosc. 2020;34:1343–52.
Kim S, Yoon YS, Han HS, Cho JY, Choi Y, Lee B. Evaluation of a single surgeon’s learning curve of laparoscopic pancreaticoduodenectomy: risk-adjusted cumulative summation analysis. Surg Endosc. 2020. https://doi.org/10.1007/s00464-020-07724-z.
van Hilst J, de Rooij T, Bosscha K, et al. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4:199–207.
Tanaka M, Heckler M, Mihaljevic AL, et al. Systematic review and metaanalysis of lymph node metastases of resected pancreatic neuroendocrine tumors. Ann Surg Oncol. 2020. https://doi.org/10.1245/s10434-020-08850-7.
Gao Y, Gao H, Wang G, et al. A meta-analysis of prognostic factor of pancreatic neuroendocrine neoplasms. Sci Rep. 2018;8:7271.
Dong DH, Zhang XF, Lopez-Aguiar AG, et al. Tumor burden score predicts tumor recurrence of non-functional pancreatic neuroendocrine tumors after curative resection. HPB Oxf. 2019. https://doi.org/10.1016/j.hpb.2019.11.009.
Dong DH, Zhang XF, Poultsides G, et al. Impact of tumor size and nodal status on recurrence of nonfunctional pancreatic neuroendocrine tumors ≤2 cm after curative resection: a multi-institutional study of 392 cases. J Surg Oncol. 2019;120:1071–9.
Davis CJ, Ilstrup DM, Pemberton JH. Influence of splenectomy on survival rate of patients with colorectal cancer. Am J Surg. 1988;155:173–9.
Griffith JP, Sue-Ling HM, Martin I, et al. Preservation of the spleen improves survival after radical surgery for gastric cancer. Gut. 1995;36:684–90.
Schwarz RE, Harrison LE, Conlon KC, Klimstra DS, Brennan MF. The impact of splenectomy on outcomes after resection of pancreatic adenocarcinoma. J Am Coll Surg. 1999;188:516–21.
Shiratori Y, Kawase T, Nakata R, et al. Effect of splenectomy on hepatic metastasis of colon carcinoma and natural killer activity in the liver. Dig Dis Sci. 1995;40:2398–406.
Higashijima J, Shimada M, Chikakiyo M, et al. Effect of splenectomy on antitumor immune system in mice. Anticancer Res. 2009;29:385–93.
Hwang HK, Murakami T, Kiyuna T, et al. Splenectomy is associated with an aggressive tumor growth pattern and altered host immunity in an orthotopic syngeneic murine pancreatic cancer model. Oncotarget. 2017;8:88827–34.
Acknowledgments
The authors thank the members of Korean Pancreas Surgery Club for their active contribution to this study: In Seok Choi (Department of Surgery, Konyang University College of Medicine, Daejeon, Korea), Sun-Whe Kim (Department of Surgery, National Cancer Center, Goyang, Korea), Woo Jung Lee (Department of Hepatobiliary and Pancreatic Surgery, Yonsei University College of Medicine, Seoul, Korea), In Woong Han (Division of Hepatobiliary-Pancreatic Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea), Dong Sup Yoon (Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea), Koo Jeong Kang (Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Keimyung University Dongsan Hospital, Daegu, Korea), Seog Ki Min (Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea), Hyeon Kook Lee (Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea), Soon Chan Hong (Department of Surgery, Gyeongsang National University College of Medicine, Jinju, Korea).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hwang, H.K., Song, K.B., Park, M. et al. Minimally Invasive Versus Open Pancreatectomy for Right-Sided and Left-Sided G1/G2 Nonfunctioning Pancreatic Neuroendocrine Tumors: A Multicenter Matched Analysis with an Inverse Probability of Treatment-Weighting Method. Ann Surg Oncol 28, 7742–7758 (2021). https://doi.org/10.1245/s10434-021-10092-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10092-0