Abstract
Background
Regionalization of complex visceral surgery across the United States has followed identification of a volume-outcome association. However, improvements in postoperative mortality overall during the last decade may have weakened the strength of this association.
Methods
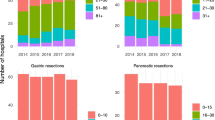
The National Cancer Database was used to identify patients undergoing colon, esophageal, liver, and pancreatic surgery from 2003 to 2011. Hospitals were divided into low-volume (< 33rd %tile), medium-volume (34–66th %tile), and high-volume (> 67th %tile) groups. Annual cancer-specific adjusted observed versus expected (O/E) ratios for 30- and 90-day mortality for each volume strata were calculated and plotted over time.
Results
In the year 2003, the O/E ratios decreased from low- to medium- to high-volume hospitals for all cancer surgeries for both 30- and 90-day mortality, indicating a strong volume-outcome relationship. For all volume strata, the O/E ratios trended downward from 2003 to 2011 for both 30- and 90-day mortality for all cancer surgeries. This trend was more pronounced for low- and medium-volume than for high-volume hospitals. Consequently, by 2011 the confidence intervals of the O/E ratios for the low-volume groups, and particularly for the medium-volume groups, overlapped those for the high-volume groups for most of the cancer surgeries studied.
Conclusions
The volume-outcome association for major cancer surgery is dynamic and has attenuated over time primarily due to improvements in postoperative mortality at low- and medium-volume hospitals.



Similar content being viewed by others
References
Urbach DR. Pledging to eliminate low-volume surgery. N Engl J Med. 2015;373:1388–90.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37.
Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–51.
Available at www.leapfroggroup.org/ratings-reports/surgical-volume. Accessed Nov 2018.
Fong ZV, Loehrer AP, Fernandez-Del Castillo C, et al. Potential impact of a volume pledge on spatial access: a population-level analysis of patients undergoing pancreatectomy. Surgery. 2017;162:203–10.
Schwartz DM, Fong ZV, Warshaw AL, et al. The hidden consequences of the volume pledge: “no patient left behind”? Ann Surg. 2017;265:273–4.
Wasif N, Etzioni D, Habermann EB, Mathur A, Pockaj BA, Gray RJ, Chang YH. Racial and socioeconomic differences in the use of high-volume commission on cancer-accredited hospitals for cancer surgery in the United States. Ann Surg Oncol. 2018;25:1116–25.
Zafar SN, Shah AA, Channa H, Raoof M, Wilson L, Wasif N. Comparison of rates and outcomes of readmission to index vs nonindex hospitals after major cancer surgery. JAMA Surg. 2018;153:719–27.
Learn PA, Bach PB. A decade of mortality reductions in major oncologic surgery: the impact of centralization and quality improvement. Med Care. 2010;48:1041–9.
Birkmeyer JD. Progress and challenges in improving surgical outcomes. Br J Surg. 2012;99:1467–9.
Wasif N, Etzioni DA, Habermann EB, et al. Does improved mortality at low- and medium-volume hospitals lead to attenuation of the volume-to-outcomes relationship for major visceral surgery? J Am Coll Surg. 2018;227:85–93.
Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37.
Cohen ME, Liu Y, Ko CY, et al. Improved surgical outcomes for ACS NSQIP hospitals over time: evaluation of hospital cohorts with up to 8 years of participation. Ann Surg. 2016;263:267–73.
Statistical Inference Pacific Grove, California: Duxbury/Thomson Learning. 2002.
Ingraham AM, Richards KE, Hall BL, et al. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251–67.
Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9.
Etzioni DA, Wasif N, Dueck AC, et al. Association of hospital participation in a surgical outcomes monitoring program with inpatient complications and mortality. JAMA. 2015;313:505–11.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81.
Sheetz KH, Dimick JB, Ghaferi AA. Impact of hospital characteristics on failure to rescue following major surgery. Ann Surg. 2016;263:692–7.
Funk LM, Gawande AA, Semel ME, et al. Esophagectomy outcomes at low-volume hospitals: the association between systems characteristics and mortality. Ann Surg. 2011;253:912–7.
Acknowledgment
This study was supported in part by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
No financial disclosures or conflicts of interest for any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wasif, N., Etzioni, D., Habermann, E.B. et al. Contemporary Improvements in Postoperative Mortality After Major Cancer Surgery are Associated with Weakening of the Volume-Outcome Association. Ann Surg Oncol 26, 2348–2356 (2019). https://doi.org/10.1245/s10434-019-07413-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07413-9