Abstract
Background
Overdiagnosis and overtreatment of ductal carcinoma in situ (DCIS) are concerns, especially for women with low-volume, screen-detected DCIS. This study aimed to evaluate the outcomes for such patients.
Methods
Women who had minimal-volume DCIS (mDCIS, defined as DCIS diagnosed by core biopsy but with no residual disease on the surgical excision) treated with breast-conserving surgery from 1990 to 2011 were identified. Ipsilateral and contralateral breast events (IBE and CBE) were compared by competing-risk (CR) analysis. Kaplan–Meier (KM) estimates and log-rank tests were used to evaluate covariates.
Results
The study identified 290 cases of mDCIS. The median age of the patients was 53 years. Radiation therapy (RT) was performed for 27.6% and endocrine therapy for 16.2% of the patients. The median follow-up period was 6.8 years. Overall, the IBE rates were 4.3% at 5 years and 12.3% at 10 years. Among the women not receiving RT, the 5- and 10-year IBE rates (5.4 and 14.5%) were higher than the CBE rates (1.8 and 2.7%). Among those receiving RT, the IBE rates (1.5 and 6.0%) were lower than the CBE rates (4.1 and 15.6%). The women receiving RT trended toward significantly lower IBE rates (p = 0.07). Age, grade, and endocrine therapy were not significantly associated with IBE risk.
Conclusions
Among the patients with mDCIS who did not receive RT, the IBE risk was substantially higher than the CBE risk, demonstrating that even DCIS of very low volume is associated with clinically relevant disease. The finding that the IBE risk was greater than the CBE risk supports current strategies that treat DCIS as a precursor rather than a risk marker. Women with mDCIS are not at negligible risk for IBE in the absence of adjuvant therapy.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30.
Wong JS, Chen YH, Gadd MA, Gelman R, Lester SC, Schnitt SJ, et al. Eight-year update of a prospective study of wide excision alone for small low- or intermediate-grade ductal carcinoma in situ (DCIS). Breast Cancer Res Treat. 2014;143:343–50.
Solin LJ, Gray R, Hughes LL, Wood WC, Lowen MA, Badve SS, et al. Surgical excision without radiation for ductal carcinoma in situ of the breast: 12-year results from the ECOG-ACRIN E5194 study. J Clin Oncol. 2015;33:3938–44.
McCormick B, Winter K, Hudis C, Kuerer HM, Rakovitch E, Smith BL, et al. RTOG 9804: a prospective randomized trial for good-risk ductal carcinoma in situ comparing radiotherapy with observation. J Clin Oncol. 2015;33:709–15.
Elshof LE, Tryfonidis K, Slaets L, van Leeuwen-Stok AE, Skinner VP, Dif N, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ: The LORD study. Eur J Cancer. 2015;51:1497–510.
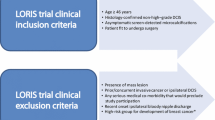
Francis A, Thomas J, Fallowfield L, Wallis M, Bartlett JM, Brookes C, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer. 2015;51:2296–303.
The Alliance for Clinical Trials In Oncology Foundation (principal investigator: Hwang S). Comparison of Operative Versus Medical Endocrine Therapy for Low-Risk DCIS: The COMET Trial. 2016. Retrieved 10 February 2017. http://www.pcori.org/research-results/2016/comparison-operative-versus-medical-endocrine-therapy-low-risk-dcis-comet.
Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–54.
Early Breast Cancer Trialists’ Collaborative G, Correa C, McGale P, Taylor C, Wang Y, Clarke M, et al. Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast. J Natl Cancer Inst Monogr. 2010;2010:162–77.
Wapnir IL, Dignam JJ, Fisher B, Mamounas EP, Anderson SJ, Julian TB, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103:478–88.
Cuzick J, Sestak I, Pinder SE, Ellis IO, Forsyth S, Bundred NJ, et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 2011;12:21–9.
Donker M, Litiere S, Werutsky G, Julien JP, Fentiman IS, Agresti R, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J Clin Oncol. 2013;31:4054–9.
Warnberg F, Garmo H, Emdin S, Hedberg V, Adwall L, Sandelin K, et al. Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol. 2014;32:3613–8.
Roychoudhuri R, Robinson D, Putcha V, Cuzick J, Darby S, Moller H. Increased cardiovascular mortality more than fifteen years after radiotherapy for breast cancer: a population-based study. BMC Cancer. 2007;7:9.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–98.
Henson KE, McGale P, Taylor C, Darby SC. Radiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancer. Br J Cancer. 2013;108:179–82.
Prochazka M, Hall P, Gagliardi G, Granath F, Nilsson BN, Shields PG, et al. Ionizing radiation and tobacco use increases the risk of a subsequent lung carcinoma in women with breast cancer: case-only design. J Clin Oncol. 2005;23:7467–74.
Grantzau T, Mellemkjaer L, Overgaard J. Second primary cancers after adjuvant radiotherapy in early breast cancer patients: a national population-based study under the Danish Breast Cancer Cooperative Group (DBCG). Radiother Oncol. 2013;106:42–9.
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005;97:1652–62.
Ganz PA, Cecchini RS, Julian TB, Margolese RG, Costantino JP, Vallow LA, et al. Patient-reported outcomes with anastrozole versus tamoxifen for postmenopausal patients with ductal carcinoma in situ treated with lumpectomy plus radiotherapy (NSABP B-35): a randomised, double-blind, phase 3 clinical trial. Lancet. 2016;387:857–65.
Masood S, Rosa M. Borderline breast lesions: diagnostic challenges and clinical implications. Adv Anat Pathol. 2011;18:190–8.
Pilewskie M, Stempel M, Rosenfeld H, Eaton A, Van Zee KJ. Do LORIS trial eligibility criteria identify a ductal carcinoma in situ patient population at low risk of upgrade to invasive carcinoma? Ann Surg Oncol. 2016;23:3487–93.
Pilewskie M, Olcese C, Patil S, Van Zee KJ. Women with low-risk DCIS eligible for the LORIS trial after complete surgical excision: how low is their risk after standard therapy? Ann Surg Oncol. 2016;23:4253–61.
Rosai J. Borderline epithelial lesions of the breast. Am J Surg Pathol. 1991;15:209–21.
Schnitt SJ, Connolly JL, Tavassoli FA, Fechner RE, Kempson RL, Gelman R, Page DL. Interobserver reproducibility in the diagnosis of ductal proliferative breast lesions using standardized criteria. Am J Surg Pathol. 1992;16:1133–43.
Tozbikian G, Brogi E, Vallejo CE, Giri D, Murray M, Catalano J, et al. Atypical ductal hyperplasia bordering on ductal carcinoma in situ. Int J Surg Pathol. 2017;25:100–7.
Choi DX, Eaton AA, Olcese C, Patil S, Morrow M, Van Zee KJ. Blurry boundaries: do epithelial borderline lesions of the breast and ductal carcinoma in situ have similar rates of subsequent invasive cancer? Ann Surg Oncol. 2013;20:1302–10.
Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, Van Zee KJ. Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol. 2010;28:3762–9.
Sweldens C, Peeters S, van Limbergen E, Janssen H, Laenen A, Patil S, et al. Local relapse after breast-conserving therapy for ductal carcinoma in situ: a European single-center experience and external validation of the Memorial Sloan-Kettering Cancer Center DCIS nomogram. Cancer J. 2014;20:1–7.
Collins LC, Achacoso N, Haque R, Nekhlyudov L, Quesenberry CP Jr, Schnitt SJ, et al. Risk prediction for local breast cancer recurrence among women with DCIS treated in a community practice: a nested, case-control study. Ann Surg Oncol. 2015;22(Suppl 3):S502–8.
Wang F, Li H, Tan PH, Chua ET, Yeo RM, Lim FL, et al. Validation of a nomogram in the prediction of local recurrence risks after conserving surgery for Asian women with ductal carcinoma in situ of the breast. Clin Oncol R Coll Radiol. 2014;26:684–91.
Sedloev T, Vasileva M, Kundurzhiev T, Hadjieva T. Validation of the Memorial Sloan-Kettering Cancer Center nomogram in the prediction of local recurrence risks after conserving surgery for Bulgarian women with DCIS of the breast. Conference Paper, presented at the 2nd World Congress on Controversies in Breast Cancer (CoBrCa), Barcelona, Spain, September 2016. Retrieved 22 March 2017 at https://www.researchgate.net/publication/312232507_Validation_of_the_Memorial_Sloan-Kettering_Cancer_Center_nomogram_in_the_prediction_of_local_recurrence_risks_after_conserving_surgery_for_Bulgarian_women_with_DCIS_of_the_breast.
Yi M, Meric-Bernstam F, Kuerer HM, Mittendorf EA, Bedrosian I, Lucci A, et al. Evaluation of a breast cancer nomogram for predicting risk of ipsilateral breast tumor recurrences in patients with ductal carcinoma in situ after local excision. J Clin Oncol. 2012;30:600–7.
Acknowledgements
The preparation of this manuscript was supported by NIH/NCI Cancer Center Support Grant no. P30 CA008748.
Disclosure
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muhsen, S., Barrio, A.V., Miller, M. et al. Outcomes for Women with Minimal-Volume Ductal Carcinoma In Situ Completely Excised at Core Biopsy. Ann Surg Oncol 24, 3888–3895 (2017). https://doi.org/10.1245/s10434-017-6043-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6043-8