Abstract
Background
Routine contrast esophagram is frequently performed after esophagectomy in order to detect occult anastomotic leak (AL). This modality has a low sensitivity, and its routine use has been called into question. Accordingly, we sought to demonstrate the clinical impact of routine contrast esophagography in the management of patients undergoing esophagectomy for malignant disease.
Methods
All patients undergoing esophagectomy from 2005 to 2011 for malignancy at a North American University hospital were identified from a prospectively collected database. Barium esophagram (BE) was performed within the first week postoperatively. Patients were dichotomized according to whether they had an AL, and the sensitivity and specificity of BE was determined. The clinical impact of the BE result, defined as cessation of enteral feeding, additional interventions, or delay in discharge, was determined.
Results
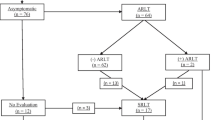
Overall, 221 patients underwent esophagectomy. Thirty (13.6 %) developed an AL, of which 10 (30 %) had a positive BE, 12 (40 %) had a negative BE, and 8 (26.7 %) had no BE and were diagnosed clinically (1/8), by computed tomography (CT) (3/8), endoscopically (3/8), or at reoperation (1/7). AL in patients with a negative BE was confirmed clinically (4/12), by CT (6/12), endoscopically (1/12), or at reoperation (1/12). The sensitivity and specificity of BE was 45.5 and 97.8 %, respectively. BE altered postoperative management in 8/221 (3.6 %) patients, with 5/221 (2.3 %) undergoing therapeutic intervention. Conversely, 3/221 (1.4 %) patients demonstrated clinically insignificant AL, delaying discharge and feeding without intervention.
Conclusion
Contrast esophagram is not an effective screening modality for AL when employed routinely following esophagectomy.


Similar content being viewed by others
References
Page RD, Shackcloth MJ, Russell GN, Pennefather SH. Surgical treatment of anastomotic leaks after oesophagectomy. Eur J Cardiothorac Surg. 2005;27(2):337–343.
Agha FP, Orringer MB, Amendola MA. Gastric interposition following transhiatal esophagectomy: radiographic evaluation. Gastrointest Radiol. 1985;10(1):17–24.
Griffin SM, Lamb PJ, Dresner SM, Richardson DL, Hayes N. Diagnosis and management of a mediastinal leak following radical oesophagectomy. Br J Surg. 2001;88(10):1346–1351.
Boone J, Rinkes IB, van Leeuwen M, van Hillegersberg R. Diagnostic value of routine aqueous contrast swallow examination after oesophagectomy for detecting leakage of the cervical oesophagogastric anastomosis. ANZ J Surg. 2008;78(9):784–790.
Honing J, Pultrum BB, van der Jagt EJ, Groen H, Plukker JT. Routine or on demand radiological contrast examination in the diagnosis of anastomotic leakage after esophagectomy. J Surg Oncol. 2009;100(8):699–702.
Pierie JP, de Graaf PW, van Vroonhoven TJ, Obertop H. Healing of the cervical esophagogastrostomy. J Am Coll Surg. 1999;188(4):448–454.
Solomon DG, Sasaki CT, Salem RR. An evaluation of the routine use of contrast radiography as a screening test for cervical anastomotic integrity after esophagectomy. Am J Surg. 2012;203(4):467–471.
Swanson JO, Levine MS, Redfern RO, Rubesin SE. Usefulness of high-density barium for detection of leaks after esophagogastrectomy, total gastrectomy, and total laryngectomy. AJR Am J Roentgenol. 2003;181(2):415–420.
Tirnaksiz MB, Deschamps C, Allen MS, Johnson DC, Pairolero PC. Effectiveness of screening aqueous contrast swallow in detecting clinically significant anastomotic leaks after esophagectomy. Eur Surg Res. 2005;37(2):123–128.
Gollub MJ, Bains MS. Barium sulfate: a new (old) contrast agent for diagnosis of postoperative esophageal leaks. Radiology. 1997;202(2):360–362.
Munitiz V, Martinez-de-Haro LF, Ortiz A, Ruiz-de-Angulo D, Pastor P, Parrilla P. Effectiveness of a written clinical pathway for enhanced recovery after transthoracic (Ivor Lewis) oesophagectomy. Br J Surg. 2010;97(5):714–718.
Ramírez JM, Blasco JA, Roig JV, et al. Enhanced recovery in colorectal surgery: a multicentre study. BMC Surg. 2011;11:9.
Lv L, Shao YF, Zhou YB. The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Colorectal Dis. 2012;27(12):1549–1554.
Lovely JK, Maxson PM, Jacob AK, et al. Case-matched series of enhanced versus standard recovery pathway in minimally invasive colorectal surgery. Br J Surg. 2012;99(1):120–126.
Cerfolio RJ, Bryant AS, Bass CS, Alexander JR, Bartolucci AA. Fast tracking after Ivor Lewis esophagogastrectomy. Chest. 2004;126(4):1187–1194.
Jiang K, Cheng L, Wang JJ, Li JS, Nie J. Fast track clinical pathway implications in esophagogastrectomy. World J Gastroenterol. 2009;15(4):496–501.
Li C, Ferri LE, Mulder DS, et al. An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery. 2012;152(4):606–614;discussion 614–606.
Gerritsen A, Besselink MG, Cieslak KP, et al. Efficacy and complications of nasojejunal, jejunostomy and parenteral feeding after pancreaticoduodenectomy. J Gastrointest Surg. 2012;16(6):1144–1151.
Llaguna OH, Kim HJ, Deal AM, Calvo BF, Stitzenberg KB, Meyers MO. Utilization and morbidity associated with placement of a feeding jejunostomy at the time of gastroesophageal resection. J Gastrointest Surg. 2011;15(10):1663–1669.
Levy RM, Trivedi D, Luketich JD. Minimally invasive esophagectomy. Surg Clin North Am. 2012;92(5):1265–1285.
Kato H, Miyazaki T, Sakai M, et al. Videofluoroscopic evaluation in oropharyngeal swallowing after radical esophagectomy with lymphadenectomy for esophageal cancer. Anticancer Res. 2007;27(6C):4249–4254.
Lanuti M, de Delva PE, Wright CD, et al. Post-esophagectomy gastric outlet obstruction: role of pyloromyotomy and management with endoscopic pyloric dilatation. Eur J Cardiothorac Surg. 2007;31(2):149–153.
Boyle MJ, Franceschi D, Livingstone AS. Transhiatal versus transthoracic esophagectomy: complication and survival rates. Am Surg. 1999;65(12):1137–1141;discussion 1141–1132.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cools-Lartigue, J., Andalib, A., Abo-Alsaud, A. et al. Routine Contrast Esophagram has Minimal Impact on the Postoperative Management of Patients Undergoing Esophagectomy for Esophageal Cancer. Ann Surg Oncol 21, 2573–2579 (2014). https://doi.org/10.1245/s10434-014-3654-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3654-1