Abstract
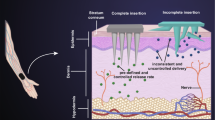
Topical treatment of fungal infections has several superiorities over oral treatment. However, the greatest challenge for dermal delivery is the stratum corneum which is considered an effective barrier for penetration of most antifungal drugs into deeper skin layers. Terconazole (Tr), which is the first marketed triazole antifungal, was reported to be one of the most active azoles against vaginal candidiasis. Nevertheless, our work group is the first to investigate the potential of Tr in the treatment of skin mycosis via integration into lecithin microemulsion-based lipogels (LMBGs). The microemulsion regions of the investigated systems were detected through ternary phase diagrams. The in vitro characterization studies revealed promising physicochemical merits for the selected LMBGs as well as satisfactory in vitro antifungal activity. The current research work was endeavored to investigate the potential of such novel Tr-loaded LMBGs in comparison with conventional gels. Ex vivo permeation and retention studies in addition to in vivo deposition study showed a significant improvement in the permeability of Tr through animal skin from LMBGs compared to other conventional gels. Furthermore, the optimized microemulsion lipogel proved to be safe and a nonirritant to experimental animals through the acute sensitivity study and histological skin examination. Overall, lecithin-based microemulsion lipogels of different composition confirmed their potential as interesting nanocarriers for skin delivery of terconazole compared to current therapy.













Similar content being viewed by others
References
Shao PL, Huang LM, Hsueh PR. Recent advances and challenges in the treatment of invasive fungal infections. Int J Antimicrob Agents. 2007;30(6):487–95. https://doi.org/10.1016/j.ijantimicag.2007.07.019.
Dabas PS. An approach to etiology, diagnosis and management of different types of candidiasis. J Yeast Fungal Res. 2013;4(6):63–74. https://doi.org/10.5897/JYFR2013.0113.
Calzavara-Pinton PG, Venturini M, Sala R. A comprehensive overview of photodynamic therapy in the treatment of superficial fungal infections of the skin. J Photochem Photobiol B Biol. 2005;78(1):1–6. https://doi.org/10.1016/j.jphotobiol.2004.06.006.
Zhang Z, Tsai P-C, Ramezanli T, Michniak-Kohn BB. Polymeric nanoparticles-based topical delivery systems for the treatment of dermatological diseases. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2013;5(3):205–18. https://doi.org/10.1002/wnan.1211.
Aggarwal N, Goindi S. Preparation and evaluation of antifungal efficacy of griseofulvin loaded deformable membrane vesicles in optimized guinea pig model of Microsporum canis-dermatophytosis. Int J Pharm. 2012;437(1–2):277–87. https://doi.org/10.1016/j.ijpharm.2012.08.015.
Kyle AA, Dahl MV. Topical therapy for fungal infections. Am J Clin Dermatol. 2004;5(6):443–51 http://www.ncbi.nlm.nih.gov/pubmed/15663341.
Gupta M, Goyal AK, Paliwal SR, Paliwal R, Mishra N, Vaidya B, et al. Development and characterization of effective topical liposomal system for localized treatment of cutaneous candidiasis. J Liposome Res. 2010;20(4):341–50. https://doi.org/10.3109/08982101003596125.
Zhang AY, Camp WL, Elewski BE. Advances in topical and systemic antifungals. Dermatol Clin. 2007;25(2):165–83. https://doi.org/10.1016/j.det.2007.01.002.
Sood G, Nyirjesy P, Weitz MV, Chatwani A. Terconazole cream for non-Candida albicans fungal vaginitis: results of a retrospective analysis. Infect Dis Obstet Gynecol. 2000;8(5–6):240–3. https://doi.org/10.1002/1098-0997(2000)8:5<240::AID-IDOG1026>3.0.CO;2-4.
El-naggar Y, Talaat SM, Bahey-el-din M, Abdallah OY. Novel lecithin-integrated liquid crystalline nanogels for enhanced cutaneous targeting of terconazole: development, in vitro and in vivo studies. Int J Nanomedicine. 2016;11:5531–47.
Elnaggar YS, Etman S, Abdelmonsif DA, Abdallah OY. Novel piperine-loaded Tween-integrated monoolein cubosomes as brain-targeted oral nanomedicine in Alzheimer’s disease: pharmaceutical , biological , and toxicological studies. Int J Nanomedicine. 2015;10:5459–73.
Elnaggar YSR, El-Massik MA, Abdallah OY. Fabrication, appraisal, and transdermal permeation of sildenafil citrate-loaded nanostructured lipid carriers versus solid lipid nanoparticles. Int J Nano. 2011;6:3195–205.
Zhai Y, Zhai G. Advances in lipid-based colloid systems as drug carrier for topic delivery. J Control Release. 2014;193:90–9. https://doi.org/10.1016/j.jconrel.2014.05.054.
Das S, Chaudhury A. Recent advances in lipid nanoparticle formulations with solid matrix for oral drug delivery. AAPS PharmSciTech. 2011;12(1):62–76. https://doi.org/10.1208/s12249-010-9563-0.
Attama AA, Momoh MA, Builders PF. Lipid nanoparticulate drug delivery systems: a revolution in dosage form design and development. In: Recent advances in novel drug carrier systems; 2012. p. 107–40. https://doi.org/10.5772/50486.
Elnaggar YSR, El-Refaie WM, El-Massik MA, Abdallah OY. Lecithin-based nanostructured gels for skin delivery: an update on state of art and recent applications. J Control Release. 2014;180:10–24. https://doi.org/10.1016/j.jconrel.2014.02.004.
Vintiloiu A, Leroux J-C. Organogels and their use in drug delivery—a review. J Control Release. 2008;125(3):179–92. https://doi.org/10.1016/j.jconrel.2007.09.014.
Kumar R, Katare OP. Lecithin organogels as a potential phospholipid-structured system for topical drug delivery: a review. AAPS PharmSciTech. 2005;6(2):298–310. https://doi.org/10.1208/pt060240.
Moulik SP, Paul BK. Structure, dynamics and transport properties of microemulsions. Adv Colloid Interf Sci. 1998;78(2):99–195. https://doi.org/10.1016/S0001-8686(98)00063-3.
Jatav MP, Ramteke S. Formulation and evaluation of lecithin organogel for treatment of arthritis. Int J Adv Sci Res. 2015;1(07):300–7. https://doi.org/10.7439/ijasr.
Luisi PL, Scartazzini R, Haering G, Schurtenberger P. Organogels from water-in-oil microemulsions. Colloid Polym Sci. 1990;268:356–74. https://doi.org/10.1007/BF01411679.
Raut S, Bhadoriya SS, Uplanchiwar V, Mishra V, Gahane A, Jain SK. Lecithin organogel: a unique micellar system for the delivery of bioactive agents in the treatment of skin aging. Acta Pharm Sin B. 2012;2(1):8–15. https://doi.org/10.1016/j.apsb.2011.12.005.
Zhao XY, Cao Q, Zheng LQ, Zhang GY. Rheological properties and microstructures of gelatin-containing microemulsion-based organogels. Colloids Surfaces A Physicochem Eng Asp. 2006;281(1–3):67–73. https://doi.org/10.1016/j.colsurfa.2006.02.051.
Jadhav KR, Shaikh IM, Ambade KW, Kadam VJ. Applications of microemulsion based drug delivery system. Curr Drug Deliv. 2006;3(3):267–73. https://doi.org/10.2174/156720106777731118.
Willimann H, Walde P, Luisi PL, Gazzaniga A, Stroppolo F. Lecithin organogel as matrix for transdermal transport of drugs. J Pharm Sci. 1992;81(9):871–4. https://doi.org/10.1016/0006-291X(91)90622-E.
Nasseri A, Aboofazeli R, Zia H, Needham T. Lecithin stabilized microemulsion based organogels for topical application of ketorlac tromethamine. II. In vitro release study. Iran J Pharm Res. 2003;2(2):117–23.
Murdan S. Organogels in drug delivery. Expert Opin Drug Deliv. 2005;2(3):489–505.
Surjyanarayan M, Sawant KK, Mandal S. Lecithin stabilized organogel: design and development for topical application of clobetasol propionate. Int J PharmTech Res. 2010;2(2):1133–8.
Thorat SP, Rane SI. Formulation and in vitro evaluation of lecithin (soya and egg) based aceclofenac organogels. J Pharm Res. 2010;3(6):1438–41.
Dreher F, Wehrli E. Interaction of a lecithin microemulsion gel with human stratum corneum and its effect on transdermal transport. J Control Release. 1997;45:131–40.
Aboofazeli R, Zia H, Needham TE. Transdermal delivery of nicardipine: an approach to in vitro permeation enhancement. Drug Deliv. 2002;9(4):239–47. https://doi.org/10.1080/10717540260397855.
Scartazzini R, Luisi P. Organogels from lecithins. J Phys Chem. 1988;92(3):829–33. https://doi.org/10.1021/j100314a047.
Gosenca M, Bešter-Rogač M, Gašperlin M. Lecithin based lamellar liquid crystals as a physiologically acceptable dermal delivery system for ascorbyl palmitate. Eur J Pharm Sci. 2013;50(1):114–22. https://doi.org/10.1016/j.ejps.2013.04.029.
Lopes LB, Speretta FFF, Bentley MVLB. Enhancement of skin penetration of vitamin K using monoolein-based liquid crystalline systems. Eur J Pharm Sci. 2007;32(3):209–15. https://doi.org/10.1016/j.ejps.2007.07.006.
Chorilli M, Prestes PS, Rigon RB, Leonardi GR, Chiavacci LA, Sarmento VHV, et al. Structural characterization and in vivo evaluation of retinyl palmitate in non-ionic lamellar liquid crystalline system. Colloids Surfaces B Biointerfaces. 2011;85(2):182–8. https://doi.org/10.1016/j.colsurfb.2011.02.027.
El Laithy HM, El-Shaboury KMF. The development of Cutina lipogels and gel microemulsion for topical administration of fluconazole. AAPS PharmSciTech. 2002;3(4):77–85. https://doi.org/10.1208/pt030435.
Nesseem DI. Formulation and evaluation of itraconazole via liquid crystal for topical delivery system. J Pharm Biomed Anal. 2001;26(3):387–99. https://doi.org/10.1016/S0731-7085(01)00414-9.
Zakir F, Vaidya B, Goyal AK, Malik B, Vyas SP. Development and characterization of oleic acid vesicles for the topical delivery of fluconazole. Drug Deliv. 2010;17(4):238–48. https://doi.org/10.3109/10717541003680981.
Kumar J, Muralidharan S, Parasuraman S. Evaluation of antifungal activity of sustained release microsponge enriched fluconazole gel for penile candidiasis in male rats. Int J PharmTech Res. 2014;6(6):1888–97.
Ozcan I, Abaci O, Uztan AH, et al. Enhanced topical delivery of terbinafine hydrochloride with chitosan hydrogels. AAPS PharmSciTech. 2009;10(3):1024–31. https://doi.org/10.1208/s12249-009-9299-x.
Kumar L, Verma S, Jamwal S, Vaidya S, Vaidya B. Polymeric microparticles-based formulation for the eradication of cutaneous candidiasis: development and characterization. Pharm Dev Technol. 2014;19(3):318–25. https://doi.org/10.3109/10837450.2013.778874.
Elmoslemany RM, Abdallah OY, El-khordagui LK, Khalafallah NM. Propylene glycol liposomes as a topical delivery system for miconazole nitrate: comparison with conventional liposomes. AAPS PharmSciTech. 2012;13(2):723–31. https://doi.org/10.1208/s12249-012-9783-6.
Vaghasiya H, Kumar A, Sawant K. Development of solid lipid nanoparticles based controlled release system for topical delivery of terbinafine hydrochloride. Eur J Pharm Sci. 2013;49(2):311–22. https://doi.org/10.1016/j.ejps.2013.03.013.
IACUC Faculty and Staff. Guideline on anesthesia and analgesia in laboratory animals. Univ South Florida. 2015:1–20. https://doi.org/10.1016/B978-012373898-1.50016-4.
Butani D, Yewale C, Misra A. Amphotericin B topical microemulsion: formulation, characterization and evaluation. Colloids Surfaces B Biointerfaces. 2014;116:351–8. https://doi.org/10.1016/j.colsurfb.2014.01.014.
Shishu, Aggarwal N. Preparation of hydrogels of griseofulvin for dermal application. Int J Pharm. 2006;326(1–2):20–4. https://doi.org/10.1016/j.ijpharm.2006.07.001.
Sahoo S, Pani NR, Sahoo SK. Microemulsion based topical hydrogel of sertaconazole: formulation, characterization and evaluation. Colloids Surfaces B Biointerfaces. 2014;120:193–9. https://doi.org/10.1016/j.colsurfb.2014.05.022.
El-Refaie WM, Elnaggar YSR, El-Massik MA, Abdallah OY. Novel curcumin-loaded gel-core hyaluosomes with promising burn-wound healing potential: development, in-vitro appraisal and in-vivo studies. Int J Pharm. 2015;486(1–2):88–98. https://doi.org/10.1016/j.ijpharm.2015.03.052.
Verma S, Bhardwaj A, Vij M, Bajpai P, Goutam N, Kumar L. Oleic acid vesicles: a new approach for topical delivery of antifungal agent. Artif Cells Nanomed Biotechnol. 2014;42(2):95–101. https://doi.org/10.3109/21691401.2013.794351.
Song SH, Lee KM, Kang JB, Lee SG, Kang MJ, Choi YW. Improved skin delivery of voriconazole with a nanostructured lipid carrier-based hydrogel formulation. Chem Pharm Bull. 2014;62(8):793–8. https://doi.org/10.1248/cpb.c14-00202.
Song CK, Balakrishnan P, Shim CK, Chung SJ, Chong S, Kim DD. A novel vesicular carrier, transethosome, for enhanced skin delivery of voriconazole: characterization and in vitro/in vivo evaluation. Colloids Surfaces B Biointerfaces. 2012;92:299–304. https://doi.org/10.1016/j.colsurfb.2011.12.004.
Ge S, Lin Y, Lu H, Li Q, He J, Chen B, et al. Percutaneous delivery of econazole using microemulsion as vehicle: formulation, evaluation and vesicle-skin interaction. Int J Pharm. 2014;465:120–31. https://doi.org/10.1016/j.ijpharm.2014.02.012.
Aggarwal N, Goindi S. Dermatopharmacokinetic and pharmacodynamic evaluation of ethosomes of griseofulvin designed for dermal delivery. J Nanopart Res. 2013;15(10):1983. https://doi.org/10.1007/s11051-013-1983-9.
IACUC Staff. Recommended methods of anesthesia, analgesia, and euthanasia for laboratory animal species. Albert Einstein Coll Med:1–12.
Gupta M, Vyas SP. Development, characterization and in vivo assessment of effective lipidic nanoparticles for dermal delivery of fluconazole against cutaneous candidiasis. Chem Phys Lipids. 2012;165(4):454–61. https://doi.org/10.1016/j.chemphyslip.2012.01.006.
Wavikar P, Vavia P. Nanolipidgel for enhanced skin deposition and improved antifungal activity. AAPS PharmSciTech. 2013;14(1):222–33. https://doi.org/10.1208/s12249-012-9908-y.
Azeem A, Talegaonkar S, Negi LM, Ahmad FJ, Khar RK, Iqbal Z. Oil based nanocarrier system for transdermal delivery of ropinirole: a mechanistic, pharmacokinetic and biochemical investigation. Int J Pharm. 2012;422(1–2):436–44. https://doi.org/10.1016/j.ijpharm.2011.10.039.
Sahoo S, Kumar N, Bhattacharya C, Sagiri SS, Jain K, Pal K, et al. Organogels: properties and applications in drug delivery. Des Monomers Polym. 2011;14(2):95–108. https://doi.org/10.1163/138577211X555721.
Janssen Inc. TERAZOL® 7 terconazole vaginal cream 0.4% w/w, product monograph. 2014:1–23. http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Product+monograph#2.
Shchipunov YA. Lecithin organogel: a micellar system with unique properties. Colloids Surfaces A Physicochem Eng Asp. 2001;185:541–54. https://doi.org/10.1016/S0927-7757(01)00511-8.
Parsaee S, Sarbolouki MN, Parnianpour M. In-vitro release of diclofenac diethylammonium from lipid-based formulations. Int J Pharm. 2002;241(1):185–90. https://doi.org/10.1016/S0378-5173(02)00238-7.
Shaikh IM, Jadhav KR, Gide PS, Kadam VJ, Pisal SS. Topical delivery of aceclofenac from lecithin organogels: preformulation study. Curr Drug Deliv. 2006;3(4):417–27.
Rane SS, Anderson BD. What determines drug solubility in lipid vehicles: is it predictable? Adv Drug Deliv Rev. 2008;60(6):638–56. https://doi.org/10.1016/j.addr.2007.10.015.
Sahle FF, Metz H, Wohlrab J, Neubert RHH. Lecithin-based microemulsions for targeted delivery of ceramide AP into the stratum corneum: formulation, characterizations, and in vitro release and penetration studies. Pharm Res. 2013;30:538–51. https://doi.org/10.1007/s11095-012-0899-x.
Zielinska-Jurek A, Reszczynska J, Grabowska E, Zaleska A. Nanoparticles preparation using microemulsion systems. In: Najjar R, editor. Microemulsions—an introduction to properties and applications. Rijeka: InTech Publisher; 2012. p. 229–50.
Aboofazeli R, Barlow D, Lawrence MJ. Particle size analysis of concentrated phospholipid microemulsions II. Photon correlation spectroscopy. AAPS PharmSci. 2000;2(2):1–10. https://doi.org/10.1208/ps020319.
Serajuddin ATM. Enhanced microemulsion formation in lipid-based drug delivery systems by combining mono-esters of medium-chain fatty acids with di- or tri-esters. J Excipients Food Chem. 2012;3(2):29–44 https://ojs.abo.fi/index.php/jefc/article/view/138.
Belitz H-D, Grosch W, Schieberle P. Food additives. In: Food chemistry; 2009. p. 429–66.
Malkin A, Isayev AI. Rheology: concepts, methods & applications. In: Rheology: concepts, methods & applications. 2nd edition; 2012. p. 127–221.
Shchipunov YA, Shumilina EV. Lecithin bridging by hydrogen bonds in the organogel. Mater Sci Eng C. 1995;3(1):43–50. https://doi.org/10.1016/0928-4931(95)00102-6.
Shchipunov YA, Mezzasalma SA, Koper GJM, Hoffmann H. Lecithin organogel with new rheological and scaling behavior. J Phys Chem B. 2001;105(43):10484–8. https://doi.org/10.1021/jp010874n.
Coneac G, Vlaia V, Olariu I, Muţ AM, Anghel DF, Ilie C, et al. Development and evaluation of new microemulsion-based hydrogel formulations for topical delivery of fluconazole. AAPS PharmSciTech. 2015;16(4):889–904. https://doi.org/10.1208/s12249-014-0275-8.
Olariu I, Coneac G, Vlaia L, et al. Development and evaluation of microemulsion-based hydrogel formulations for topical delivery of propranolol hydrochloride. Dig J Nanomater Biostructures. 2014;9(1):395–412.
Moser K, Kriwet K, Naik A, Kalia YN, Guy RH. Passive skin penetration enhancement and its quantification in vitro. Eur J Pharm Biopharm. 2001;52(2):103–12. https://doi.org/10.1016/S0939-6411(01)00166-7.
Elsheikh MA, Elnaggar YSR, Gohar EY, Abdallah OY. Nanoemulsion liquid preconcentrates for raloxifene hydrochloride: optimization and in vivo appraisal. Int J Nanomedicine. 2012;7:3787–802. https://doi.org/10.2147/IJN.S33186.
Deveda P, Jain A, Vyas N, Khambete H, Jain S. Gellified emulsion for sustain delivery of itraconazole for topical fungal diseases. Int J Pharm Pharm Sci. 2010;2(1):104–12.
Higuchi T. Physical chemical analysis of percutaneous absorption process from creams and ointments. J Soc Cosmet Chem. 1960;11(2):85–97 http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:PHYSICAL+CHEMICAL+ANALYSIS+OF+PERCUTANEOUS+ABSORPTION+PROCESS+FROM+CREAMS+AND+OINTMENTS#0.
Morrow DIJ, Mccarron PA, Woolfson AD, Donnelly RF. Innovative strategies for enhancing topical and transdermal drug delivery. Open Drug Deliv J. 2007;1:36–59. https://doi.org/10.2174/187412660701013606.
Lopes L. Overcoming the cutaneous barrier with microemulsions. Pharmaceutics. 2014;6(1):52–77. https://doi.org/10.3390/pharmaceutics6010052.
Ustündağ Okur N, Apaydın S, Karabay Yavaşoğlu NÜ, Yavaşoğlu A, Karasulu HY. Evaluation of skin permeation and anti-inflammatory and analgesic effects of new naproxen microemulsion formulations. Int J Pharm. 2011;416(1):136–44. https://doi.org/10.1016/j.ijpharm.2011.06.026.
Takahashi K, Tamagawa S, Katagi T, et al. In vitro transport of sodium diclofenac across rat abdominal skin: effect of selection of oleaginous component and the addition of alcohols to the vehicle. ChemPharm Bull. 1991;39(1):154–8.
Valenta C, Wanka M, Heidlas J. Evaluation of novel soya-lecithin formulations for dermal use containing ketoprofen as a model drug. J Control Release. 2000;63(1–2):165–73. https://doi.org/10.1016/S0168-3659(99)00199-6.
Tan Q, Liu W, Guo C, Zhai G. Preparation and evaluation of quercetin-loaded lecithin-chitosan nanoparticles for topical delivery. Int J Nanomedicine. 2011;6:1621–30. https://doi.org/10.2147/IJN.S22411.
Morrow DIJ, McCarron PA, Woolfson AD, et al. Influence of penetration enhancers on topical delivery of 5-aminolevulinic acid from bioadhesive patches. J Pharm Pharmacol. 2010;62(6):685–95. https://doi.org/10.1211/jpp.62.06.0004.
Madheswaran T, Baskaran R, Yong CS, Yoo BK. Enhanced topical delivery of finasteride using glyceryl monooleate-based liquid crystalline nanoparticles stabilized by cremophor surfactants. AAPS PharmSciTech. 2013;15(1):44–51. https://doi.org/10.1208/s12249-013-0034-2.
da Silva ER, de Freitas ZMF, Gitirana LDB, Ricci-Júnior E. Improving the topical delivery of zinc phthalocyanine using oleic acid as a penetration enhancer: in vitro permeation and retention. Drug Dev Ind Pharm. 2011;37(5):569–75. https://doi.org/10.3109/03639045.2010.529144.
El Maghraby GM, Barry BW, Williams AC. Liposomes and skin: from drug delivery to model membranes. Eur J Pharm Sci. 2008;34(4–5):203–22. https://doi.org/10.1016/j.ejps.2008.05.002.
Rhee YS, Choi JG, Park ES, Chi SC. Transdermal delivery of ketoprofen using microemulsions. Int J Pharm. 2001;228(1–2):161–70. https://doi.org/10.1016/S0378-5173(01)00827-4.
Pathan IB, Setty CM. Chemical penetration enhancers for transdermal drug delivery systems. Trop J Pharm Res. 2009;8(2):173–9. https://doi.org/10.1081/DDC-100100984.
Kanikkannan N, Kandimalla K, Lamba SS, Singh M. Structure-activity relationship of chemical penetration enhancers in transdermal drug delivery. Curr Med Chem. 2000;7(6):593–608 http://www.ncbi.nlm.nih.gov/pubmed/10702628.
Benson HA. Transdermal drug delivery: penetration enhancement techniques. Curr Drug Deliv. 2005;2(1):23–33 http://www.ncbi.nlm.nih.gov/pubmed/16305405.
Dhamecha D, Rathi AA, Saifee M, Lahoti SR, Dehghan MHG. Drug vehicle based approaches of penetration enhancement. Int J Pharm Pharm Sci. 2009;1(1):24–46.
Vicentini FTMC, Simi TRM, Del Ciampo JO, et al. Quercetin in w/o microemulsion: in vitro and in vivo skin penetration and efficacy against UVB-induced skin damages evaluated in vivo. Eur J Pharm Biopharm. 2008;69(3):948–57. https://doi.org/10.1016/j.ejpb.2008.01.012.
Zhao X, Liu JP, Zhang X, Li Y. Enhancement of transdermal delivery of theophylline using microemulsion vehicle. Int J Pharm. 2006;327(1–2):58–64. https://doi.org/10.1016/j.ijpharm.2006.07.027.
Paolino D, Ventura CA, Nisticò S, Puglisi G, Fresta M. Lecithin microemulsions for the topical administration of ketoprofen: percutaneous adsorption through human skin and in vivo human skin tolerability. Int J Pharm. 2002;244(1–2):21–31. https://doi.org/10.1016/S0378-5173(02)00295-8.
Lv Q, Yu A, Xi Y, Li H, Song Z, Cui J, et al. Development and evaluation of penciclovir-loaded solid lipid nanoparticles for topical delivery. Int J Pharm. 2009;372(1–2):191–8. https://doi.org/10.1016/j.ijpharm.2009.01.014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talaat, S.M., Elnaggar, Y.S.R. & Abdalla, O.Y. Lecithin Microemulsion Lipogels Versus Conventional Gels for Skin Targeting of Terconazole: In Vitro, Ex Vivo, and In Vivo Investigation. AAPS PharmSciTech 20, 161 (2019). https://doi.org/10.1208/s12249-019-1374-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-019-1374-3