Abstract
Background
Biliary atresia in very low birth weight (VLBW) and extremely low birth weight (ELBW) infants is rarely reported, and the optimal timing of Kasai portoenterostomy (KPE) in these cases remains unclear.
Case presentation
We report a case of biliary atresia in a preterm female infant of 24 weeks of gestation who weighed 824 g. She underwent exploratory laparotomy and intraoperative cholangiography at 58 days of age (weight, 1336 g). Despite the diagnosis of biliary atresia with a type I cyst, we could only perform gallbladder drainage at that time due to the unstable intraoperative condition. While we waited for her body weight to increase, KPE was performed at 122 days of age (corrected age: 16 days), when the patient weighed 2296 g. Although she initially became jaundice-free, her liver function deteriorated due to cholangitis, and she developed decompensated cholestatic liver cirrhosis. Living donor liver transplantation was successfully performed at 117 days after KPE, and the postoperative course was uneventful. The timing of KPE is difficult to determine and a review of the relevant literature revealed that a poor prognosis in VLBW and ELBW infants with BA.
Conclusions
Early KPE and careful postoperative follow-up, including liver transplantation is important for the improvement of outcomes.
Similar content being viewed by others
Background
Biliary atresia (BA) is a destructive inflammatory obliterative cholangiopathy of neonates that affects the intra- and extrahepatic bile ducts [1]. While the etiology remains unclear, BA is the most common cause of end-stage liver disease and is also the most frequent indication for liver transplantation (LT) in children [2, 3]. Preterm birth has been reported to be a poor prognostic factor in patients with BA [4, 5]. Although some studies have demonstrated the incidence and outcomes of BA in preterm infants, few studies have focused on BA in very low birth weight (VLBW) and extremely low birth weight (ELBW) infants. We herein report a case of BA in an ELBW preterm infant born at 24 weeks of gestation.
Case presentation
A female preterm infant weighing 824 g was born to a 37-year-old woman at 24 6/7 weeks of gestational age (GA) by induced delivery due to chorioamnionitis. Because of bradycardia and unstable respiration, endotracheal intubation was performed immediately after birth, and surfactant was administered under the diagnosis of respiratory distress syndrome (RDS). The Apgar score was 3 at 1 min, 4 at 5 min. After admission to the NICU, the patient was put on mechanical ventilator support. At 4 days of age, a patent ductus arteriosus (PDA) was noted on echocardiography. Cardiac failure due to refractory PDA worsened in spite of the administration of catecholamine and diuretics. Therefore, PDA ligation was carried out at 24 days of age.
At 15 days of age, mild hyperbilirubinemia with total bilirubin level of 3.9 mg/dL and a direct bilirubin level of 2.8 mg/dL was noted. Ursodeoxycholic acid (UDCA) and Inchinkoto (traditional Japanese herbal medicine) were administered; however, the conjugated hyperbilirubinemia worsened, and acholic stool was noted at 30 days of age. Abdominal ultrasonography showed a cystic structure at the porta hepatis with a diameter of 6.8 mm (Fig. 1); we therefore suspected BA with a type I cyst or congenital biliary dilatation (CBD). Since exploratory laparotomy (EL) and intraoperative cholangiography (IC) were essential for making a definitive diagnosis as early as possible, the operation was performed at 58 days of age, when the patient weighed 1336 g. During the operation, the liver was soft (Fig. 2a), and IC showed a cystic common bile duct that had no communication with the duodenum, with the intrahepatic ductules showing a cloudy pattern (Fig. 2b). These findings indicated BA with a type I cyst. Although we had initially planned to perform KPE for BA sequentially, we could only perform gallbladder drainage because the patient’s vital signs worsened during the operation. Since there were no significant bleeding or other intraoperative complications, the patient’s immaturity was considered to be the cause of this unstable condition.
Intraoperative findings at 58 days of age (exploratory laparotomy and cholangiography). a The liver (arrowhead) was still soft. A drainage tube (arrow) was placed in the gallbladder. b Cholangiography revealed a cystic common bile duct (arrow) that had no communication with the duodenum and a cloudy pattern of intrahepatic ductules (circle)
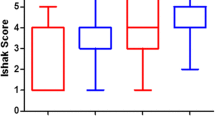
After surgery, the color of the fluid drained from the gall bladder was yellowish, and the serum bilirubin level had improved but was not normal, which indicated that cyst-jejunostomy would be ineffective and that Kasai portoenterostomy (KPE) was necessary. We decided to wait for the patient to gain weight and to maintain her general condition. She was extubated at 72 days of age. At 122 days of age (corrected age: 16 days), we performed KPE, with the patient weighing 2296 g. The liver had become firm and cirrhotic (Fig. 3), and portoenterostomy with Roux-en-Y reconstruction was completed without complications. The examination of a liver biopsy revealed bridging fibrosis and cholestasis. The postoperative course was good, and prednisolone was administered from postoperative day (POD) 7 to 31 in accordance with our institution’s routine practice [6]. The serum bilirubin level normalized at POD 27. The patient’s body weight successfully increased (Fig. 4).
Although a jaundice-free status was initially achieved, the serum bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) levels began to increase following the development of cholangitis at 157 days of age (POD 35). Secondary prednisolone therapy was performed; however, the liver function continued to worsen (Fig. 5). Cholestasis, increasing ascites, coagulopathy, and gastrointestinal bleeding were noted subsequently with a pediatric end-stage liver disease (PELD) score 26 and Child–Pugh class C. At 221 days of age (corrected age: 133 days, 117 days after KPE), we performed living donor liver transplantation, with the patient weighing 4106 g. The donor was the patient's mother, who was 38 years of age and whose blood type was identical. The graft was a segment 2 (S2) monosegment graft and the graft-to-recipient weight ratio was 3.23%. Post-transplantation management was conducted as described in our previous report [7]. The postoperative course was uneventful, and the serum bilirubin and liver function profiles normalized by the first postoperative month. Currently, at 14 months after LT, the patient is well and shows a normal liver function with relatively good growth in height (-1.7 SD) and weight (-0.9 SD).
Discussion
BA is a rare disease with an incidence of 1 in 8000–15,000 live births [1, 8]. According to the Japanese Biliary Atresia Registry (JBAR), 3,362 BA patients were identified in Japan from 1989 to 2017. Among them there were only 30 cases (0.89%) whose birth weight was less than 1500 g [9, 10]. Since these patients were rarely reported, the clinical course and therapeutic strategy remain unclear. We reported a case with a birth weight of 824 g, which is the lowest weight recorded for a BA patient in Japan.
In the present case, despite diagnosing the patient with BA by cholangiography at 58 days of age, we could not perform radical surgery at the time due to the unstable intraoperative condition. To determine the timing of KPE, we had to consider weight gain, the stabilization of the cardiac and respiratory condition, and the progress of treatment for PDA and RDS. We then performed KPE at 122 days of age (corrected age: 16 days). Eventually, the patient required LT due to the development of biliary cirrhosis at 3 months after KPE.
Preterm birth is reported to be a poor prognostic factor in BA; however, the exact mechanism remains unclear [4, 5, 11]. In general, the preoperative prognostic factors of KPE are the age at the operation, the presence of the biliary atresia splenic malformation (BASM) syndrome, liver histology, and the anatomic pattern of the bile ducts [12,13,14]. Most reports indicate that operating at an early age improves the prognosis [4, 12, 14]. Some studies have also investigated the ideal timing of KPE in preterm BA patients. Iwasaki et al. [15] recommended that surgery be performed by a corrected age of 60 days in preterm infants. Jiao et al. [4] also indicated, based on a retrospective study of 34 preterm BA patients, that KPE at a chronological age of ≤ 90 days and a corrected age of ≤ 60 days provided a good prognosis. On the other hand, a study of BA in preterm infants in Taiwan [11], which used the national registry system data, demonstrated that the mean corrected age at the time of KPE was 32.2 days (chronological age: 71.8 days) and that the native liver survival rate of preterm BA patients at 18 months of age was significantly lower than that of term infants (50% vs. 72.7%). This result suggests that the prognosis of preterm BA patients is poor, even if KPE is performed within a corrected age of 60 days.
Because few studies focused on BA in VLBW and ELBW infants, a review of the relevant literature was performed using PubMed and Ichushi-Web (a search engine for Japanese literature) to identify the characteristics and prognosis of these cases. Our search yielded 8 cases in the relevant English and Japanese literature; these cases and the present case are summarized in Table 1 [16,17,18,19,20]. All cases involved preterm birth, and the mean birth weight was 1123.8 g. Three cases were ELBW infants; our case had the lowest birth weight and was the only surviving ELBW infant among these reports. One case underwent primary LT, and the other seven underwent KPE. The mean body weight at KPE was 2385.2 g, probably because—in many of the cases—the operation was deferred empirically until a weight gain of 2000–2500 g was achieved. Although six cases underwent KPE within the corrected age of 60 days, five (83.3%) required subsequent LT in this review. The native liver survival rate of VLBW and ELBW infants with BA was found to be much poorer in comparison to general preterm BA patients, even though the KPE was performed within the corrected age of 60 days. Careful follow-up and avoiding delays in LT are necessary to improve the outcome.
The poor prognosis of KPE may imply the insufficiency of the criterion of the corrected age of 60 days. Given that recent studies have suggested that BA only manifests after loss of the protective physiology of the mother and placenta [2], the chronological age at KPE may reflect the prognosis more accurately rather than the corrected age. Actually, in our case, despite the liver being relatively soft at the first surgery (EL and IC) at 58 days of age, it became cirrhotic by the time of the second surgery (KPE) at 122 days of age. On the other hand, however, when KPE is performed too early, before sufficient weight gain can be achieved is associated with an increased risk of intraoperative and postoperative complications. Further studies with a larger sample size, which focus on BA in VLBW and ELBW infants should be performed to clarify the optimal timing of KPE in these cases.
Conclusions
We described the clinical course and prognosis of BA in VLBW and ELBW infants. It is preferable to perform KPE earlier; however, the optimal timing is difficult to determine due to their complicated clinical condition. Because of the poor prognosis of KPE, careful postoperative follow-up, including LT, are important for improving patient outcomes.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Abbreviations
- BA:
-
Biliary atresia
- LT:
-
Liver transplantation
- VLBW:
-
Very low birth weight
- ELBW:
-
Extremely low birth weight
- GA:
-
Gestational age
- RDS:
-
Respiratory distress syndrome
- PDA:
-
Patent ductus arteriosus
- UDCA:
-
Ursodeoxycholic acid
- CBD:
-
Congenital biliary dilatation
- EL:
-
Exploratory laparotomy
- IC:
-
Intraoperative cholangiography
- KPE:
-
Kasai portoenterostomy
- POD:
-
Postoperative day
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- PT:
-
Prothrombin time
- PELD:
-
Pediatric end-stage liver disease
- JBAR:
-
Japanese Biliary Atresia Registry
- BASM:
-
Biliary atresia splenic malformation
References
Davenport M. Biliary atresia. Lancet. 2009;374:1704–13.
Bezerra JA, Wells RG, Mack CL, Karpen SJ, Hoofnagle JH, Doo E, et al. Biliary atresia: clinical and research challenges for the twenty-first century. Hepatology. 2018;68(3):1163–73.
Scheenstra R, Peeters PMGJ, Verkade HJ, Gouw ASH. Graft fibrosis after pediatric liver transplantation: ten years of follow-up. Hepatology. 2009;49(3):880–6.
Jiao C, Yu K, Li D, Fu K, Wang P, He Y, et al. A retrospective study of the ideal operation time for preterm biliary atresia patients. Pediatr Surg Int. 2019;35(6):679–84.
Van Wessel DBE, Boere T, Hulzebos CV, De Kleine RHJ, Verkade HJ, Hulscher JBF, et al. Preterm infants with biliary atresia: a nationwide cohort analysis from the Netherlands. J Pediatr Gastroenterol Nutr. 2017;65(4):370–4.
Nio M, Muraji T. Multicenter randomized trial of postoperative corticosteroid therapy for biliary atresia. Pediatr Surg Int. 2013;29(11):1091–5.
Yoshimaru K, Matsuura T, Hayashida M, Kinoshita Y, Takahashi Y, Yanagi Y, et al. Transient hyperphosphatasemia after pediatric liver transplantation. Pediatr Int. 2016;58(8):726–31.
Nio M. Japanese Biliary Atresia Registry. Pediatr Surg Int. 2017;33(12):1319–25.
Japanese Biliary Atresia Society. Japanese biliary atresia registry 2017. J Jpn Soc Pediatr Surg. 2019;55(2):291–7 ((in Japanese)).
10Japanese Biliary Atresia Society. Japanese Biliary Atresia Registry 2017. https://jbas.net/registration. Accessed 1 May 2020.
Chiu CY, Chen PH, Chan CF, Chang MH, Wu TC. Biliary atresia in preterm infants in Taiwan: a nationwide survey. J Pediatr. 2013;163(1):100–3.
Song Z, Dong R, Shen Z, Chen G, Yang Y, Zheng S. Surgical outcome and etiologic heterogeneity of infants with biliary atresia who received Kasai operation less than 60 days after birth: a retrospective study. Medicine. 2017;96(26):1–5.
Wong KKY, Chung PHY, Chan IHY, Lan LCL, Tam PKH. Performing Kasai portoenterostomy beyond 60 days of life is not necessarily associated with a worse outcome. J Pediatr Gastroenterol Nutr. 2010;51(5):631–4.
Townsend MR, Jaber A, Abi Nader H, Eid SM, Schwarz K. Factors associated with timing and adverse outcomes in patients with biliary atresia undergoing Kasai hepatoportoenterostomy. J Pediat. 2018;199:237–42.
Iwasaki M, Hashimoto K, Kamimura R, Ikeda Y, Kobayashi H, Hanafusa T, et al. Clinical diagnosis and surgical management for cholestasis in premature infant. J Jpn Soc Pediatr Surg. 2006;42:470–9 ((in Japanese)).
Chen HW, Hsu WM, Chang MH, Chen CY, Chou HC, Tsao PN, et al. Embryonic biliary atresia in a very-low-birth-weight premature infant. J Formos Med Assoc. 2007;106(1):78–81.
Hashimoto K, Nakamura K, Ikeda Y, Sokoda T, Furukawa O. Shindan chiryō ni kuryoshita tandōheisashō no chōteishussei taijūji no ichirei [A case of biliary atresia in an extremely low birth weight infant with difficult diagnosis and treatment]. Perinatal Medicine. 2007;37:149–53 ((in Japanese)).
Fallon SC, Chang S, Finegold MJ, Karpen SJ, Brandt ML. Discordant presentation of biliary atresia in premature monozygotic twins. J Pediatr Gastroenterol Nutr. 2013;57(4):e22–3.
Sanmoto Y, Masumoto K, Sakamoto N, Aoyama T, Fujii S, Chiba F, et al. A case of a very low birth weight infant diagnosed as having biliary atresia. Jpn Soc Pediatr Surg. 2017;53:958–61 ((in Japanese)).
Miyatake H, Sakamoto R, Nakamura K. Five cases of preterm infant with biliary atresia. J Jpn Pediatr Soc. 2018;122:1474–80 ((in Japanese)).
Acknowledgements
We thank Brian Quinn (editor-in-chief, Japan Medical Communication, Inc., Fukuoka, Japan) for his assistance with the reading and editing of the manuscript.
Funding
The authors received no funding related to the manuscript.
Author information
Authors and Affiliations
Contributions
YK and KY contributed to the writing. TM contributed to the critical review and revision. YK, KY, YU, KK, YT, TS, YT, and TM performed the surgery and postoperative management. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kawano, Y., Yoshimaru, K., Uchida, Y. et al. Biliary atresia in a preterm and extremely low birth weight infant: a case report and literature review. surg case rep 6, 321 (2020). https://doi.org/10.1186/s40792-020-01092-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-020-01092-5