Abstract
Background
Musculoskeletal injuries (MSkIs) are a leading cause of health care utilization, as well as limited duty and disability in the US military and other armed forces. MSkIs affect members of the military during initial training, operational training, and deployment and have a direct negative impact on overall troop readiness. Currently, a systematic overview of all risk factors for MSkIs in the military is not available.
Methods
A systematic literature search was carried out using the PubMed, Ovid/Medline, and Web of Science databases from January 1, 2000 to September 10, 2019. Additionally, a reference list scan was performed (using the “snowball method”). Thereafter, an international, multidisciplinary expert panel scored the level of evidence per risk factor, and a classification of modifiable/non-modifiable was made.
Results
In total, 176 original papers and 3 meta-analyses were included in the review. A list of 57 reported potential risk factors was formed. For 21 risk factors, the level of evidence was considered moderate or strong. Based on this literature review and an in-depth analysis, the expert panel developed a model to display the most relevant risk factors identified, introducing the idea of the “order of importance” and including concepts that are modifiable/non-modifiable, as well as extrinsic/intrinsic risk factors.
Conclusions
This is the qualitative systematic review of studies on risk factors for MSkIs in the military that has attempted to be all-inclusive. A total of 57 different potential risk factors were identified, and a new, prioritizing injury model was developed. This model may help us to understand risk factors that can be addressed, and in which order they should be prioritized when planning intervention strategies within military groups.
Similar content being viewed by others
Background
Musculoskeletal injuries (MSkIs) are a leading cause of health care utilization, as well as limited duty and disability in the US military [1] and other armed forces [2,3,4,5,6]. MSkIs affect members of the military during initial training [7], operational training [8], and deployment [9], and have a direct negative impact on overall troop readiness. MSkIs have been shown to make up 50% of disease and non-battle injury (DNBI) casualties, and 43% of DNBI casualties requiring evacuation. Additionally, many service members sustain MSkIs, which are treated conservatively in the theater during deployment, but eventually require surgery following a combat tour [10, 11]. The consequences of MSkIs are reduced individual fitness and health [12], and ultimately discharge from military duty [13, 14].
As such, the prevention of MSkIs is considered a main target area to increase the readiness, performance, and health of military personnel. Approaches include the identification of risk factors and purposeful intervention strategies to reduce MSkIs. In recent decades, hundreds of original studies have been published with the goal of identifying risk factors for MSkIs, including narrative and systematic reviews on specific risk factors [15,16,17,18,19,20,21,22,23,24,25,26]. However, an overall summary of the published data on risk factors for MSkIs in the military is not available. Further, for several risk factors, such as sex, there is an ongoing debate on whether there is a direct association with an increased risk of MSkIs, or whether the association is indirect via a confounding risk factor [27]. Finally, there is no model that clarifies the relative order of importance of the risk factors for MSkIs in the military.
Given the gaps in knowledge identified above and the fact that soldier readiness is of great importance to all allied militaries, the multidisciplinary NATO Science and Technology Organization (STO) Research Task Group (RTG) 283 on “Reducing musculoskeletal injuries” set out to perform a systematic review of risk factors for MSkIs in the military to address and discuss the facilitation of successful interventions.
Methods
A systematic literature search considering the PRISMA guidelines [28] was initiated using the PubMed, Ovid/Medline, and Web of Science databases with the search terms “(military) AND ((injury) OR (trauma)) AND ((basic training) OR (physical training))” with all MeSH terms (see details on Additional file 1) on September 10, 2019. The principal criterion for inclusion was that the study reported on risk factors for MSkIs in a military population. The exclusion criteria were as follows: a language other than English; studies without a risk factor evaluation; and studies published before January 1, 2000. Review articles (without a meta-analysis) were used to find the included original works (see below), but were not included as such in this review. Of the 1794 studies identified (after removing duplicates), 179 were selected for full-text analysis. After full-text analysis, 42 papers were excluded because they did not meet the inclusion criteria, and 19 studies were reviews and did not present new information. So far, a total of 118 original papers and 3 meta-analyses have been included.
Moreover, to present a complete overview, a reference list scan (using the “snowball method”) [29] was performed on each of the 179 fully analyzed texts, including each of the 19 review articles. With this approach, an additional 283 studies were identified, of which 87 were excluded due to the publication date being before January 1, 2000. The remaining 196 papers were also read in full to determine relevance. If two studies reported on exactly the same population, only the publication that provided the most details was included. As a result, an additional 58 studies were included in this review, bringing the total to 176 original papers and 3 meta-analyses (Fig. 1).
Once all the literature was identified, a list of all reported risk factors was created. Each original paper and meta-analysis was then assigned to a risk factor. If an original paper described multiple risk factors, it was assigned to every risk factor it reported.
In the results section, a general description of all the included publications is provided first, followed by specific descriptions per risk factor. Risk factors were sorted into different groups (in alphabetical order): lifestyle factors, medical factors, occupational factors, physiological factors, social factors, and training factors. For each risk factor, an accompanying table was included that summarizes each aspect of the supporting studies: lead author; year of publication; country of origin; characteristics of the population examined (branch and unit/type of military activity); study type (retrospective or prospective); sample size of the population studied; and whether or not the study concluded that the risk factor was correlated to MSkIs (yes or no). In a number of publications, more than one risk factor was evaluated.
Finally, the multidisciplinary expert panel (consisting of all coauthors of this review) classified the evidence supporting the association between a risk factor and MSkI into one of five categories: strong, moderate, weak, insufficient, or no evidence. For this classification, the expert panel took into account the results of the studies, as well as the number of participants and their professional experience in military MSkI injury prevention. In addition, the expert panel included a determination as to whether a risk factor would be considered modifiable or non-modifiable in the military context. A risk factor was defined as modifiable if a service member could influence it (e.g., to be a smoker) or if military authorities could influence it (e.g., by changing the training schedule or by providing other gear). Risk factors classified as non-modifiable are beyond personal control (e.g., the weather). Whether a risk factor is modifiable is a significant determinant for the application of intervention strategies. Based on the literature review and an in-depth analysis, the multidisciplinary expert panel developed a model to classify the different risk factors identified, introducing the concept of “order of importance” and including the notions of modifiable/non-modifiable and extrinsic/intrinsic risk factors.
Results
Of the 176 original papers, 101 came from investigations in the US Armed Forces. Additional investigations were conducted in the armed forces of the UK (19 studies), Israel (18 studies), and Finland (14 studies). Australia and Switzerland produced 4 studies each, China and Greece had 3 studies each, Germany had 2 studies, and Belgium, Denmark, India, Iran, Malta, Poland, Slovenia, and Sweden were represented by 1 study each. A majority of the studies examined risk factors in the army (113 studies), whereas there were considerably fewer studies conducted in the marines (16 studies), the air force (7 studies), the navy (5 studies), and the special operations forces (2 studies). Seven studies explored risk factors, including multiple armed services branches; 4 studies were conducted only among recruits or participants in academy training, and 22 studies did not include descriptions of the particular service branch. More than half of the studies (n = 101) chose a prospective study design, and the remaining 75 papers evaluated data retrospectively. The study populations ranged from 20 subjects [30] to 5,580,875 analyzed person-years [31]. In two studies [32, 33], no information about the underlying size of the population was reported. Less than half of the studies (n = 79) scrutinized populations of less than 1000 participants, while 27 studies had a population greater than 10,000 participants. A number of retrospective studies involved populations with over 100,000 participants [31, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]. A large minority of the studies included both male and female military personnel (n = 51). In 33 studies, only male members were included, whereas 17 studies focused exclusively on women in the military. In most of the studies (n = 75), no specific information was given about the sex of the included participants.
Lifestyle factors
Alcohol intake
Nine studies focused on higher alcohol intake as a risk factor for MSkIs (Table 1). Five studies were conducted in the US Army, 2 within the British Army, and 1 in Finland and in Greece. The sizes of the study populations ranged from 64 to 4139 participants. Three of the 9 studies identified alcohol intake as a risk factor for MSkIs, and 6 did not show a significant association between alcohol intake and MSkIs.
There is insufficient scientific evidence for alcohol intake as a modifiable risk factor.
Calcium intake (low)
Four studies focused on low (daily) calcium intake as a risk factor for MSkIs (Table 1). Three studies were conducted in the Israel Defense Force (IDF) and one in the Armed Forces of Greece. The sizes of the study populations ranged from 64 to 2306 participants. Only the study with one of the smallest populations identified low daily calcium intake as a risk factor for MSkIs. The other three studies, including one with more than 2000 participants, did not find a significant association.
There is insufficient scientific evidence for low (daily) calcium intake as a modifiable risk factor.
Milk consumption (low)
Three studies focused on milk consumption as a risk factor for MSkIs (Table 1). The research was conducted within the militaries of Israel, the USA, and the UK (1 study from each country). The sizes of the study populations ranged from 116 to 1082 participants. Only one study identified low milk consumption as a risk factor for MSkIs; the other two studies did not find a significant association.
There is insufficient scientific evidence for low milk consumption as a modifiable risk factor.
Vegetable consumption
Two studies focused on the amount of vegetables eaten (as measured via a self-report questionnaire) as a risk factor for MSkIs (Table 1). The research was conducted within different branches of the UK military. The sizes of the study populations ranged from 1082 to 1810 participants. Neither study found a significant association between the amount of vegetable consumption and MSkIs.
There is no scientific evidence for the amount of vegetable consumption as a modifiable risk factor for MSkIs.
Vegetarian diet
Only one study focused on a vegetarian diet as a risk factor for MSkIs (Table 1). This study was conducted within the Indian Army. In this study, with 8570 participants, a vegetarian diet was identified as a risk factor for stress fractures.
There is weak scientific evidence for a vegetarian diet as a modifiable risk factor.
(Reduced) sleep time
Two studies focused on little time for sleep as a risk factor for MSkIs (Table 1). These studies were conducted within the Army of Switzerland and the Army of Slovenia. The sizes of the study populations ranged from 129 to 1676 participants. A larger study identified little time for sleep as a risk factor for MSkIs; however, this was not observed within the smaller study.
There is weak scientific evidence for little time for sleep as a modifiable risk factor.
Smoking
Fifty-four studies focused on smoking as a risk factor for MSkIs (Table 1). Most of the research was conducted within different branches of the US Armed Forces (32 studies); additional studies were conducted within the militaries of the UK (8 studies), Finland (5 studies), China, Israel, Switzerland (2 studies from each) and Greece, Malta and Slovenia (1 study from each nation). The study populations ranged from 64 to 238,772 participants. Twenty-seven studies identified smoking as a risk factor for MSkIs, and 23 studies did not find a significant association between smoking and MSkI. One study found a significant increase in MSkIs related to a lower level of smoking, and one study found that former smoking habits were a significant risk factor for MSkIs. In one study, the association between smoking and increased risk for MSkIs was found only for males (not for females). A meta-analysis, which included 18 studies, found that smoking increases the risk for MSkIs, for males by 26% (a low level of smoking) up to 84% (a high level of smoking) and for females by 30% (low level of smoking) up to 56% (high level of smoking) [24]. For both sexes together, the increased risk ranges from 27 to 71%.
There is strong scientific evidence for smoking as a modifiable risk factor for MSkIs. Smoking is associated with a 27–71% increased risk of MSkIs.
Medical factors
Current illness
The term “current illness” was used to describe the situation where an injured person was ill (e.g., with influenza at the time the MSkI occurred). There was only one study on current illness as a risk factor for MSkIs (Table 2). The study was conducted in 2010 in the US Armed Forces. With 24,177 male participants, this study found a significant association between current illness and an increased risk for MSkIs. It must be noted that the risk factor “current illness” may represent a bias. Soldiers with an identified current illness are generally removed from active duty and training. This means that current illness is a risk factor mostly based on retrospective self-report by the service member.
There is weak scientific evidence for current illness as a non-modifiable risk factor.
The prescription of contraceptives
Four studies focused on the prescription of contraceptives as a risk factor for MSkIs (Table 2). Most of the research was conducted within different branches of the US Armed Forces (3 studies). An additional study was conducted within the IDF. The sizes of the study populations ranged from 350 to 2962 participants. None of the four studies identified the prescription of contraceptives as a risk factor for MSkIs.
There is no scientific evidence for the prescription of contraceptives as a modifiable risk factor for MSkIs.
The prescription of non-steroidal anti-inflammatory drugs (NSAIDs)
Only one study focused on the prescription of a NSAID as a risk factor for MSkIs (Table 2). This study was conducted within the US Army. In this retrospective study, with 120,730 participants, the prescription of a NSAID was identified as a risk factor for MSkIs (specifically stress fractures). There may be a bias between NSAID use and increased risk for a stress fracture because with the medication, soldiers may have stayed in training longer and consequently were more likely to suffer a fracture. Therefore, this study also explored the relationship with a subset who were taking NSAIDs for non-pain or injury reasons and found a similar relationship with increased risk for MSkIs.
There is weak scientific evidence for prescription for a NSAID as a modifiable risk factor.
Previous MSkIs
Thirty studies focused on previous MSkIs as a risk factor for MSkIs (Table 2). Most of the research was conducted within different branches of the US Armed Forces (18 studies); the remaining research was conducted within the militaries of the UK (3 studies), Israel and China (2 studies from each), Australia, Finland, Slovenia, Sweden, and Switzerland (1 study from each nation). The sizes of the study populations ranged from 53 to 83,323 participants. Nineteen of the 30 studies identified an earlier MSkI as a risk factor for MSkIs; 7 studies did not find a significant association. Two studies found a significant association only for one sex but not the other. The remaining two studies found that an earlier MSkI reduced the risk for MSkIs.
There is strong scientific evidence for earlier MSkIs as a non-modifiable risk factor for MSkIs.
Prior pregnancy
Only one study focused on prior pregnancy as a risk factor for MSkIs (Table 2). This study was conducted within the US Army. In this study, with 920 female participants, prior pregnancy > 7 months prior was identified as a risk factor for MSkIs.
There is weak scientific evidence for prior pregnancy as a non-modifiable risk factor.
Serum iron/serum ferritin (lower)
Two studies focused on serum iron/serum ferritin as a risk factor for MSkIs (Table 2). Both studies were conducted within the IDF. The sizes of the study populations were 227 and 438 participants. Both studies identified low serum iron/serum ferritin as a risk factor for MSkIs.
There is weak scientific evidence for low serum iron/serum ferritin as a modifiable risk factor.
Vitamin D status [low level of 25(OH)D]
Four studies focused on vitamin D status as a risk factor for MSkIs (Table 2). The studies were conducted within the militaries of the UK (2 studies), Israel, and the US (1 study from each country). The sizes of the populations of both UK studies [65, 127] were the same. The study populations ranged from 1082 to 2306 participants. Three studies identified low vitamin D status as a risk factor for MSkIs, while another study did not find a significant association. The two studies from the UK reported different outcomes. Davey et al. [127] reported a significant difference in vitamin D level for participants who have suffered a stress fracture when compared to a group that did not [(64.2 ± 28.2) nmol/L for participants with stress fracture vs. (78.6 ± 35.9) nmol/L for participants without a stress fracture, P = 0.004]. Alternatively, Sanchez-Santos et al. [65] presented the results as odds ratios with a cutoff value for a low level of vitamin D at 50 nmol/L. They found no difference in the likelihood of stress fractures between the groups above and below the vitamin D level cutoff (P = 0.077).
In a meta-analysis by Dao et al. [23], it was reported that the mean serum 25(OH)D level was lower in stress fracture cases than in controls at the time of entry into basic training. The mean serum 25(OH)D level was also lower in the stress fracture cases at the time of stress fracture diagnosis.
There is moderate scientific evidence for a low level of vitamin D status as a modifiable risk factor.
Occupational factors
Branch
Three studies focused on membership in different branches as a risk factor for MSkIs (Table 3). Two studies were conducted within the US Armed Forces and 1 within the Army of Finland. The sizes of the study populations ranged from 982 to 423,581 participants. All 3 studies identified membership to different branches as a risk factor for MSkIs.
There is strong scientific evidence for branches as a non-modifiable risk factor for MSkI.
Length of service
Eight studies focused on the length of service as a risk factor for MSkIs (Table 3). Half of the research was conducted within different branches of the US Armed Forces (4 studies), and the remaining studies were conducted within the militaries of Finland (2 studies), Israel, and the UK (1 study from each country). The sizes of the study populations ranged from 195 to 152,095 participants. Five studies identified that military servicemen and servicewomen with a longer length of service have an increased risk for MSkIs; 3 studies did not find a significant association. Two of the largest studies only examined conscripts (Kuikka et al. [36] and Mattila et al. [38]), with a small range of lengths of service, and found conflicting results. Hill et al. [115] included a broad range of active duty personnel and showed a strong association for military servicemen and women with more than 10 years of service for an increased risk of MSkIs. Reynolds et al. [98] and Wilkinson et al. [60] detected no association, but had only a small range of lengths of service.
There is moderate scientific evidence for length of service as a non-modifiable risk factor.
Load carriage
Six studies focused on load carriage as a risk factor for MSkIs (Table 3). Most of the research was conducted in the US Armed Forces (5 studies); the remaining study was conducted within the IDF. The sizes of the study populations ranged from 263 to 1423 participants. Five studies identified body-borne load as a risk factor for MSkIs, with 3 of the 5 studies reporting load via self-report. One study found no association between load carriage and the risk for MSkIs.
There is strong scientific evidence for body-borne load as a modifiable risk factor for MSkI.
Military occupational specialty (MOS)
Seven studies focused on military occupational specialties (MOS) as a risk factor for MSkIs (Table 3). Most of the research was conducted within the US Armed Forces, 2 studies were from the IDF, and only 1 study was from the military of the UK. The sizes of the study populations ranged from 1788 to 19,791 participants. All but one study (with light infantry) identified membership in different MOSs as a risk factor for MSkIs.
There is strong scientific evidence for MOS as a non-modifiable risk factor for MSkI.
Previous deployment
Four studies focused on previous deployment as a risk factor for MSkIs (Table 3). All 4 studies were conducted within different branches of the US Armed Forces. The sizes of the study populations ranged from 625 to 83,323 participants. Three of the 4 studies identified previous deployment as a risk factor for MSkI, and 1 study did not find a significant association.
There is moderate scientific evidence for previous deployment as a non-modifiable risk factor.
Status (active vs. reserve)
Three studies focused on status (active vs. reserve) as a risk factor for MSkIs (Table 3). All 3 studies were conducted within the US Armed Forces. The sizes of the study populations ranged from 1902 to 3367 participants. All 3 studies identified status as a risk factor for MSkIs: 1 study only for women (when they are in the reserve instead of active duty), 1 for active personnel vs. reserve, and 1 for reserve vs. active personnel.
There is no scientific evidence for being part of the reserve (instead of active duty) as a non-modifiable risk factor for MSkIs.
Physiological factors
Age
Sixty-five studies focused on age as a risk factor for MSkIs (Table 4). Most of the research was conducted within different branches of the US Armed Forces, 8 within the military of the UK, and 7 within the military of Finland; the other studies were conducted within the militaries of China (3 studies), Israel (2 studies), Belgium, Greece, Iran, Poland, and Switzerland (1 study for each country). The study populations ranged from 44 to 5,580,875 participants. Thirty-three of the 65 studies identified older age as a risk factor for MSkIs (however, the definitions of older age differ across studies); 30 studies did not find a significant association between age and MSkIs, while 1 study found a significant rise in MSkIs for younger participants when compared to older participants. When only studies with a population of 1400 or more participants were taken into account (this represents 31 of the 65 studies), 23 studies revealed a significant association between age and an increased risk for MSkIs compared to only 8 studies that did not find a significant association. When only studies that had 5000 participants or more were considered, the relationship was 12 (significant association) vs. 1 (no association).
There is moderate scientific evidence for age as a non-modifiable risk factor.
Ankle dorsiflexion (limited)
Only 2 studies focused on limited ankle dorsiflexion as a risk factor for MSkIs (Table 4). One study was conducted within the IDF, and one in the armed forces of the UK. The sizes of the study populations were 20 and 70 participants, respectively. In both studies, limited ankle dorsiflexion was not significantly identified as a risk factor for MSkIs.
There is no scientific evidence for limited ankle dorsiflexion as a non-modifiable risk factor.
Balance (low)
Two studies focused on low balance as a risk factor for MSkIs (Table 4). These studies were conducted within the special operations forces of the US military. In the larger study, poor balance (measured as single-leg balance with the eyes open, and the eyes closed on a force plate) was identified as a risk factor for MSkIs, whereas in the other studies, no association was identified.
There is weak scientific evidence for low balance as a modifiable risk factor.
BMI: in general
Fifty-two studies focused on BMI (in general) as a risk factor for MSkIs (Table 5). BMI in general means that the studies have looked at BMI without categorization (such as obese, overweight, underweight categories). This makes it very difficult to compare different study outcomes. Most of the research was conducted within different branches of the US Armed Forces (24 studies); 9 studies within the military of the UK, 6 within the Finnish armed forces, and 5 within the IDF. The remaining studies were conducted in the militaries of Switzerland (3 studies), Greece (2 studies), Australia, Belgium, and Malta (1 study each). The sizes of the study populations ranged from 44 to 238,772 participants. Fourteen of the 52 studies identified BMI as a risk factor for MSkIs. Thirteen studies found that higher BMI was a risk factor; 1 study found that lower BMI was a risk factor. Thirty-five studies did not find a significant association between BMI and MSkIs, and 3 studies found that BMI is a risk factor for men, but not for women.
There is insufficient scientific evidence for BMI in general as a modifiable risk factor.
BMI: obesity (BMI ≥ 30 kg/m2)
Seventeen studies focused on obesity as a risk factor for MSkIs (Table 5). Most of the research was conducted within different branches of the US Armed Forces (12 studies). Additional studies were conducted within the militaries of Finland (3 studies), China, and Germany (1 study for each country). The sizes of the study populations ranged from 410 to 387,536 participants. Sixteen studies identified obesity as a risk factor for MSkIs; only one study, with 1568 participants, did not find a significant association.
There is strong scientific evidence for obesity (BMI ≥ 30 kg/m2) as a modifiable risk factor for MSkIs.
BMI: overweight (BMI ≥ 25 and < 30 kg/m2)
Sixteen studies focused on being overweight as a risk factor for MSkIs (Table 5). Most of the research was conducted within different branches of the US Armed Forces (10 studies); the remaining studies were conducted within the Finnish armed forces (4 studies) and within the militaries of China and Germany (1 study each). The sizes of the study populations ranged from 410 to 736,608 participants. Eleven studies identified being overweight as a risk factor for MSkIs; 4 studies did not find a significant association. One study found an association for men but not for women. It is important to acknowledge that these findings are based on BMI alone; none of the 16 studies analyzed the body composition of the included soldiers in detail (i.e., body fat or muscle mass).
There is strong scientific evidence for being overweight (BMI ≥ 25 and < 30 kg/m2) as a modifiable risk factor for MSkI.
BMI: underweight (BMI < 18.5 kg/m2)
Fifteen studies focused on being underweight as a risk factor for MSkIs (Table 5). Most of the research was conducted within different branches of the US Armed Forces (10 studies); the remaining studies were conducted within the militaries of Finland (3 studies), China, and Israel (1 study each). The sizes of the study populations ranged from 135 to 736,608 participants. Twelve studies identified being underweight as a risk factor for MSkIs, and 3 studies did not find a significant association.
There is strong scientific evidence for being underweight (BMI < 18.5 kg/m2) as a modifiable risk factor for MSkIs.
Body fat (higher)
Eight studies focused on body fat as a risk factor for MSkIs (Table 6). The research was conducted within the armies of Greece (2 studies), Iran (1 study), Israel (2 studies), and the US (3 studies); the studies included different methods for measuring body fat (e.g., self-report, circumference, dual-energy X-ray absorptiometry, 4-site skinfold test). The sizes of the study populations ranged from 44 to 583,651 participants. Six of the 8 studies identified a higher percentage of body fat as a risk factor for MSkIs, and 2 studies did not find a significant association. A retrospective study by Knapik et al. [46], with more than a half million participants, showed a relationship between a greater percentage of body fat and a higher risk for MSkIs.
There is strong scientific evidence for higher body fat as a modifiable risk factor for MSkIs.
Body height (higher)
Forty-six studies focused on body height as a risk factor for MSkIs (Table 6). Most of the research was conducted within different branches of the US Armed Forces (18 studies); 8 within the military of the UK, 7 within the military of Finland, and 6 studies within the IDF; the other studies were conducted within the military of China (3 studies), Belgium, Iran, Poland, and Sweden (1 study each). The sizes of the study populations ranged from 44 to 583,651 participants. Eight of the 46 studies identified a taller stature as a risk factor for MSkIs, and 35 studies did not find a significant association. One study found a significant increase in MSkIs associated with a taller stature for men but not for women, and one study found that a shorter stature was a significant risk factor for MSkIs.
There is insufficient scientific evidence for body height as a non-modifiable risk factor for MSkIs.
Body weight (higher)
Forty-five studies focused on body weight as a risk factor for MSkIs (Table 6). Most of the research was conducted within different branches of the US Armed Forces (16 studies); 11 studies within the military of the UK, and 6 within the IDF. The remaining studies were conducted within the militaries of Finland (4 studies), China (2 studies), Australia, Belgium, Greece, Iran, Poland, and Sweden (1 study each). The sizes of the study populations ranged from 44 to 583,651 participants. Thirteen of the 45 studies identified a higher body weight as a risk factor for MSkIs, 27 did not find a significant association between body weight and MSkIs, and 3 studies found a significant increase in MSkIs for a lower body weight. Two studies found different outcomes regarding the participants’ sex.
There is insufficient scientific evidence for higher body weight as a modifiable risk factor.
Bone (mineral) density (low)
Three studies focused on low bone (mineral) density as a risk factor for MSkIs (Table 7). All 3 studies were conducted in the US Army. The sizes of the study populations ranged from 230 to 891 participants. Two studies identified low bone (mineral) density as a risk factor for MSkIs; one study did not find a significant association.
There is insufficient scientific evidence for low bone (mineral) density as a non-modifiable risk factor.
External rotation of the hip (higher)
Five studies focused on external rotation (range of motion) of the hip as a risk factor for MSkIs (Table 7). The research was conducted within the militaries of Australia (2 studies), Iran, Israel, and the US (each 1 study). The range of motion of the hip was measured in different ways across the identified studies. The sizes of the study populations ranged from 77 to 748 participants. Three studies (including the two with the most participants) identified that higher external rotation of the hip is a risk factor for MSkIs; two studies did not find a significant association.
There is insufficient scientific evidence for higher external rotation of the hip as a non-modifiable risk factor.
Flexibility (lower)
Five studies focused on flexibility at different anatomical locations as a risk factor for MSkIs (Table 7). Most of the research was conducted within different branches of the US Armed Forces (4 studies), and 1 study was conducted by armed forces from China. The sizes of the study populations ranged from 95 to 805 participants. Only 1 study identified low flexibility as a risk factor for MSkIs, and 5 studies did not find a significant association.
There is insufficient scientific evidence for lower flexibility as a modifiable risk factor.
Foot type
Eight studies focused on foot type (e.g., anatomic differences such as a pes planus, a wide malleolar or a forefoot varus) as a risk factor for MSkIs (Table 7). The studies were conducted within the militaries of the UK (3 studies), USA (2 studies), Australia, Israel, and Malta (1 study from each country). The sizes of the study populations ranged from 124 to 504 participants. Five studies identified different foot types as a risk factor for MSkI, while 3 studies did not.
There is moderate scientific evidence for different foot types as a non-modifiable risk factor.
Genetic factors
Two studies focused on genetic factors as risk factors for MSkIs (Table 8). One study was conducted within the military of China and 1 within the military of Finland. The study populations ranged from 192 to 1398 participants. Both studies identified an association between certain genetic factors and an increased risk for MSkIs. The analyzed genetic factors were different between the 2 studies, so a comparison was not possible. Korvala et al. [89] examined genes involved in bone metabolism and pathology, and Zhao et al. [108] looked at a specific growth differentiation factor 5 (GDF5) polymorphism between recruits with and without stress fractures.
There is weak scientific evidence for genetic factors as a non-modifiable risk factor.
Late menarche
Seven studies focused on late menarche as a risk factor for MSkIs (Table 8). All of the research was conducted within different branches of the US Armed Forces. The sizes of the study populations ranged from 136 to 3758 participants. Two studies identified late menarche as a risk factor for MSkIs, and 5 studies did not find a significant association.
There is no scientific evidence for late menarche as a non-modifiable risk factor for MSkIs.
Muscular strength (lower)
Eleven studies focused on muscular strength as a risk factor for MSkIs (Table 8), although it was measured in different ways depending on the study. Most of the research was conducted within the US Army (5 studies) or the military of Finland (4 studies). Additional studies were conducted within the militaries of Switzerland and the UK (1 study from each country). The sizes of the study populations ranged from 95 to 152,095 participants. Six studies identified low muscular strength as a risk factor for MSkIs, while 5 studies did not find a significant association. Notably, two studies with more than 100,000 participants found an inverse association between muscular strength and the risk for MSkIs, the other study found no association, but this study focused on traumatic patellar luxation.
There is moderate scientific evidence for lower muscular strength as a modifiable risk factor.
Physical fitness (low)
Seventy-four studies focused on physical fitness, based on results from physical fitness tests, as a risk factor for MSkIs (Table 8). Most of the research was conducted in different branches of the US Armed Forces (45 studies); 12 studies were conducted within the military of the UK, and 9 were conducted within the military of Finland. The remaining studies were conducted within the militaries of Israel and Switzerland (2 studies each) as well as China, Denmark, Germany, and Malta (1 study each). The size of the study population ranged from 44 to 238,772 participants. Fifty studies identified low physical fitness as a risk factor for MSkIs. Out of these 50 studies, 4 studies explored low physical endurance. Two studies found an association between low physical fitness and an increased risk for MSkI, but not for both sexes, and 20 studies did not find a significant association. In two studies, there was an inverse effect; high physical fitness was associated with an increased risk for MSkIs. A meta-analysis that included 27 publications found that the relative risk is 2.34 (95% CI 2.02—2.70) for injuries incurred during training, as well as for personnel who perform in the bottom quartile or quintile when compared to their peers in the top quartile or quintile of physical fitness [25].
There is strong scientific evidence for low physical fitness as a modifiable risk factor for MSkIs. Low physical fitness has an increased relative risk of 2.34 for MSkIs.
Secondary amenorrhea
Eight studies focused on having no menses in the last months (secondary amenorrhea) as a risk factor for MSkIs (Table 9). All of the research was conducted within different branches of the US Armed Forces. The sizes of the study populations ranged from 86 to 2962 participants. Three studies identified secondary amenorrhea as a risk factor for MSkIs, and 5 studies did not find a significant association.
There is insufficient scientific evidence for secondary amenorrhea as a modifiable risk factor.
Sex (female)
Thirty-eight studies focused on sex as a risk factor for MSkIs (Table 9). Most of the research was conducted within different branches of the US Armed Forces (24 studies). Additional studies were conducted within the militaries of Israel and the UK (4 studies each), Finland (3 studies), Australia (2 studies), and Greece (1 study). The sizes of the study populations ranged from 124 to 5,580,875 participants. Twenty-nine studies identified being female as a risk factor for MSkIs (when compared to males), 8 studies did not find a significant association between sex and MSkIs, and 1 study found a significant increase in MSkIs for males when compared to females.
There is strong scientific evidence that being female is a non-modifiable risk factor for MSkIs.
Plantar pressure assessment (of walking gait)
Five studies focused on plantar pressure assessment (of walking gait) as a risk factor for MSkIs (Table 9). Most of the research was conducted within different branches of the UK military (3 studies). Additional studies were conducted within the militaries of Belgium and Israel (1 study from each country). The study populations ranged from 69 to 468 participants. All studies included males only. Two studies identified a particular foot pressure pattern while walking as a risk factor for MSkIs, and two studies did not find a significant association. In one study, this association was only found for a pressure pattern involving the little toe (digitus V).
There is insufficient scientific evidence for specific plantar pressure patterns during walking as a modifiable risk factor.
Range of tibial rotation during running (lower)
Only one study focused on the range of tibial rotation (calculated as the difference between peak internal and external rotation) during running as a risk factor for MSkIs (Table 9). This study was conducted within the UK Marines. In this prospective study with 160 male participants, a lower range of tibial rotation during running (the difference between peak internal and external lower leg segment rotation) was identified as a risk factor for MSkIs.
There is weak scientific evidence for a lower range of tibial rotation during running as a modifiable risk factor.
Tibia length (shorter)
Four studies focused on tibia length as a risk factor for MSkIs (Table 9). The research was conducted within the IDF (2 studies) and within the US Marines (1 study) and within the army of China (1 study). The sizes of the study populations ranged from 44 to 1398 participants. Two studies identified a shorter tibia length as a risk factor for MSkIs, and the two studies did not find a significant association. Hence, one of these studies reported leg length, not tibia length.
There is insufficient scientific evidence for shorter tibia length as a modifiable risk factor.
Waist circumference (higher)
Five studies focused on high circumference as a risk factor for MSkIs (Table 9). Three studies were conducted within the military of Finland, and two were carried out within the US Air Force. The size of the study populations ranged from 141 to 67,525 participants. Two studies from Finland identified high circumference as a risk factor for MSkIs, while the other 3 studies did not find a significant association. Especially, the retrospective study by Nye et al. [151], with 67,525 participants, found no association between high waist circumference and an increased risk for MSkIs.
There is insufficient scientific evidence for a high waist circumference as a modifiable risk factor.
Social factors
Education (lower)
Thirteen studies focused on education as a risk factor for MSkIs (Table 10). Nearly half of the research was conducted within different branches of the US Armed Forces (6 studies); the others were conducted within the militaries of Finland (4 studies), the UK (2 studies), and Israel (1 study). The sizes of the study populations ranged from 205 to 4029 participants. Five of the 13 studies identified a lower level of education as a risk factor for MSkIs, and 8 studies did not find a significant association between lower education and MSkIs. The definitions of lower education are different among the studies examined.
There is weak scientific evidence for a lower level of education as a non-modifiable risk factor for MSkIs.
Marital status
Six studies focused on marital status as a risk factor for MSkIs (Table 10). All of the research was conducted within different branches of the US Armed Forces (mostly in the army). The sizes of the study populations ranged from 205 to 83,323 participants. Only one study (with the largest number of participants examined) identified being married as a risk factor for MSkI. Another study identified being divorced or widowed as a risk factor for MSkIs. The remaining 4 studies did not find a significant association between marital status and MSkIs.
There is insufficient scientific evidence for marital status as a non-modifiable risk factor.
Race/ethnicity
Twenty-seven studies focused on race/ethnicity as a risk factor for MSkIs (Table 10). Most of the research was conducted within different branches of the US Armed Forces (24 studies); 2 studies were conducted within the militaries of the UK, and 1 was conducted in Israel. The sizes of the study populations ranged from 86 to 5,580,875 participants. Seventeen studies identified race/ethnicity as a risk factor for MSkIs, while 10 studies did not find a significant association. When only studies with more than 10,000 participants were taken into account (9 studies, total: 8,640,581 participants), all studies found an association between race/ethnicity and the risk for MSkIs, but the findings were contradictory in that there was no clear association as to which race/ethnicity was at the highest risk.
There is strong scientific evidence for race/ethnicity as a non-modifiable risk factor for MSkIs.
Rank (lower)
Eleven studies focused on rank as a risk factor for MSkIs (Table 10). All except one of the studies were conducted within different branches of the US Armed Forces, and the exception was conducted within the British Army. The sizes of the study populations ranged from 230 to 242,949 participants or aircraft exits. Six studies identified as having a lower rank as a risk factor for MSkIs, and 5 studies did not find a significant association between rank and MSkIs (3 of the 5 had less than 1000 participants).
There is weak scientific evidence for lower rank as a non-modifiable risk factor.
Seasons of the year (summertime)
Four studies focused on the seasons of the year as a risk factor for MSkIs (Table 10). Two studies were conducted within the Finnish armed forces and two within the US Army. The study populations ranged from 955 to 2568 participants, and one study examined 213,500 person-years. All 4 studies identified the effect of the season of the year as a risk factor for MSkIs, with a higher risk in the summer months.
There is strong scientific evidence for the season of the year (summertime) as a non-modifiable risk factor for MSkIs.
UV index (higher)
Only one study focused on the UV index (a surrogate for vitamin D exposure) as a risk factor for MSkIs (Table 10). This study was conducted within the US Army. In this retrospective study, with 511,602 participants, a higher UV index at a recruit’s home before basic combat training (BCT) was identified as a risk factor for MSkIs during BCT. The relative risk reduction for a lower UV index was small (0.92 and 0.89 vs. 1.00, P < 0.01).
There is weak scientific evidence for a higher UV index as a non-modifiable risk factor.
Training factors
Equipment: running shoes
Only one study focused on running shoes as a risk factor for MSkIs (Table 11). This study was conducted within the US Armed Forces. In this prospective study, with 827 participants, no association between the kinds of running shoes and an increased risk for MSkIs could be identified.
There is no scientific evidence for the kinds of running shoes as a modifiable risk factor.
Participation in sports before military service (no or low)
Twenty-four studies focused on a history of participation in sports before military service as a risk factor for MSkIs (Table 11). Most of the research was conducted among recruits or those new to military service within different branches of the US Armed Forces (13 studies). The militaries of China, Finland, and Israel conducted 2 studies each; the remaining studies were conducted within the militaries of Australia, Denmark, India, Sweden, and the UK (1 study each). The sizes of the study populations ranged from 53 to 8570 participants. Fifteen studies identified no or low participation in sports before military service time as a risk factor for MSkIs, and 6 studies (all with fewer than 350 participants) did not find a significant association. In two studies, an association was found only for men, and in another study, an inverse association was found (higher participation in a sport before military service was a risk factor for MSkIs).
There is strong scientific evidence for no or low participation in sports before military service time as a non-modifiable risk factor for MSkIs.
Physical training: available participation time (low)
Two studies focused on the amount of time available to take part in physical training as a risk factor for MSkIs (Table 11). The research was conducted within the US Army (1 study) and the army of Switzerland (1 study). The sizes of the study populations were 1677 and 1676 participants. The study from Switzerland found an association between having little time for physical training and an increased risk for MSkIs, while the study from the US military did not show a significant association.
There is insufficient scientific evidence for having little time available for taking part in physical training as a modifiable risk factor.
Physical training: participation rate (low)
Six studies focused on participation in physical training as a risk factor for MSkIs (Table 11). Most of the research was conducted within different branches of the US Armed Forces (5 studies). An additional study was conducted within the military of the UK. The study populations ranged from 195 to 6865 participants. Three studies identified a low participation rate in physical training as a risk factor for MSkIs, and 3 studies did not find a significant association.
There is insufficient scientific evidence for the participation rate in physical training as a modifiable risk factor.
Physical training: personnel, non-military training (high amounts)
Eight studies focused on high amounts of training during free time (non-military training) as a risk factor for MSkIs (Table 11). Most of the research was conducted within the army and the Marines Corp of the US Armed Forces (5 studies in total). Additional studies were conducted within the militaries of Finland, Israel, and Switzerland (1 study from each country). The sizes of the study populations ranged from 116 to 4236 participants. Three studies identified a high amount of personal training during free time as a risk factor for MSkIs, and 3 studies did not find a significant association. Two studies found an inverse effect; a low amount of personal training was associated with an increased risk of MSkIs.
There is insufficient scientific evidence for high amounts of personnel training during free time as a modifiable risk factor.
Physical training: unit training (high amount)
Eleven studies focused on physical training during unit training as a risk factor for MSkIs (Table 11). Most of the research was conducted within different branches of the US Armed Forces (8 studies). Additional studies were conducted within the militaries of China, Israel, and Switzerland (1 study from each). The study populations ranged from 44 to 67,525 participants. Eight studies identified a high amount of training during unit training as a risk factor for MSkIs, whereas 3 studies did not find a significant association.
There is strong scientific evidence for high amounts of training during unit training as a modifiable risk factor for MSkIs.
Training program content
Four studies focused on different training program content as a risk factor for MSkIs (Table 11). Three studies were conducted within the US Armed Forces and 1 in the Army of Slovenia. The sizes of the study populations ranged from 129 to 1967 participants. One study included a total of 10,511 person-years. Three studies identified that different training program content could be a risk factor for MSkIs, and the smallest study found no association.
There is weak scientific evidence for training program content as a modifiable risk factor.
Training site
Six studies focused on the training site as a risk factor for MSkIs (Table 11). The studies were conducted within the militaries of the US Armed Forces (3 studies), the UK (2 studies), and Israel (1 study). The sizes of the study populations ranged from 660 to 24,177 participants. Three studies identified the training site as a risk factor for MSkIs (two of these studies had more than 10,000 participants), and 3 studies did not find a significant association between the training site and MSkIs. It should be taken into account that the training site is a combination of many different factors (e.g., training situation, climate, infrastructure, etc.), so it is very difficult to identify the true factor that influenced the MSkI risk.
There is weak scientific evidence for training sites as a possibly modifiable risk factor.
Risk factor classification
In sum, 57 potential risk factors for MSkIs in the military were identified. Twenty-one factors were classified as risk factors with a strong or moderate association with an increased risk for MSkIs. For 14 other potential risk factors, an association was possible, but the evidence in the scientific literature was considered weak. For the final 22 potential risk factors, the evaluation showed either insufficient evidence or no evidence. As such, they cannot be classified as risk factors for an increased risk for MSkIs at this time (Table 12).
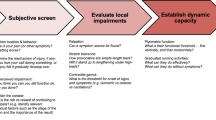
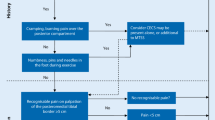
Based on this systematic literature review and an in-depth analysis, the NATO HFM-283 Research Task Group developed a model to classify the different risk factors identified. The classification model was based upon the rationale that some risk factors directly increase MSkI risk, whereas others merely increase the risk for MSkIs indirectly as a cofactor. As an example of a direct factor (1st order), high amounts of training during unit training increase the total volume of load placed upon the biological tissues of the soldier, directly resulting in injury. Alternatively, as an example of a cofactor, low vitamin D levels may lead to lower bone density, which may result in lower tissue resilience, which in turn may cause an MSkI due to the training load now exceeding the soldier’s reduced tissue capacity. The term “order” was used to classify how close each risk factor was to a direct cause of injury. A 1st-order risk factor was thought to be most closely related to injury, whereas a 3rd-order factor was thought to follow a path through multiple cofactors. Table 12 shows all risk factors categorized as 1st, 2nd, or 3rd order of importance. Additionally, the model includes the established concepts of modifiable/non-modifiable and extrinsic/intrinsic risk factors. This prioritizing classification model may guide the planning and implementation of intervention strategies, introducing the notion that a larger risk reduction can likely be achieved if risk factors in a higher order are targeted (Fig. 2).
Discussion
This review is the qualitative systematic review of studies on risk factors for MSkIs in the military that has attempted to be all-inclusive. With a total of 179 original papers and 3 meta-analyses from the past two decades, a very large number of studies on MSkIs in the military were included. A total of 57 different risk factors were identified and evaluated.
The approach used in this study identified more risk factors for MSkIs in the military than previously reported [15,16,17,18,19,20,21,22,23,24,25,26]. The aim was to have an overview of all risk factors in one place. Further, the project is one of the first to include the classification of risk factors for MSkIs in the military into modifiable or non-modifiable categories. This additional distinction (modifiable vs. non-modifiable) helps us to understand which risk factors can be addressed and which ones cannot be addressed when an intervention is planned.
In addition to listing all potential risk factors, the members of the multidisciplinary expert panel assessed the combined evidence presented for each risk factor on a five-grade scale (strong evidence to no evidence). The number of participants (e.g., > 10,000 subjects) significantly influenced the evaluation of available evidence. Some classifications of available evidence had to be made based on a small number of studies with a small number of participants. The final rating also included the subjective professional experience (opinion) of the experts on the panel.
This review introduces a new injury model for the military, incorporating the established principles of modifiable vs. non-modifiable and intrinsic vs. extrinsic risk factors. The model clearly illustrates differences between risk factors; some increase the risk for MSkIs directly (1st order), whereas others influence the injury risk only indirectly (2nd or 3rd order). The model may explain why many of the interventions that have been attempted over the past decades to reduce MSkIs were not successful. In fact, a systematic review of successful interventions in reducing MSkIs in the military [6] shows that the only successful interventions are those that target 1st- and 2nd-order modifiable risk factors (i.e., in the upper half of the model).
Hence, most of the scientific publications are from the US Armed Forces, with studies conducted by other countries much less frequently. As such, the findings may not be generalizable across all nations. In addition, most studies focused on one branch of the armed forces—the army—which might not be representative of all service branches. Transferring the information from one country to another or from one military branch to another must be done with great caution.
Even with the very broad systematic approach used in this review, no studies on psychological, cognitive, and/or behavioral risk factors for MSkIs in the military could be identified. In civilian sports, these risk factors have been reported for several years [202, 203]. It is possible that the search terms used in this review did not allow for psychological factors to be identified or the psychosocial aspects of injuries.
This review has several limitations. First, the method used is a variation of the strict PRISMA protocol for systematic reviews. The group of coauthors decided that the topic at hand deserved a broad approach, including all possible risk factors and all military studies, even those with a potentially poor scientific design. In addition, it was decided to include the multidisciplinary, professional experience of the group as a subjective element in assessing the level of evidence per risk factor reported. Second, all studies before 2000 were excluded. This was decided because training schedules and conditions in the militaries have changed significantly over the past two decades and anticipated that including studies from before 2000 would not yield additional, currently relevant insights. Third, this review did not include studies on risk factors for MSkIs in civilian sports activities. Although some of the risk factors for civilian sports injuries are the same, the military training environment has many unique aspects that make risk factors for MSkIs not comparable to civilian sports. Fourth, differences in how the risk factors were measured (e.g., self-report vs. direct measurements) or the potential interrelationships between risk factors (e.g., that the strong evidence for sex as a risk factor may be related to differences in the percentage of body fat or previous physical activity before service between the sexes) were not considered when assigning the level of evidence for each risk factor. However, these issues were taken into account when depicting the 1st-, 2nd-, or 3rd-order level of the risk factors in the model. Fifth, this review did not include calculated effect sizes or a meta-analysis of every risk factor. Of course, this could further enhance the scientific value of the current work. The authors propose that future scientific evaluations can now be done, concentrating on the risk factors that have been identified as high order and modifiable in this work.
Conclusions
This systematic review presents an all-inclusive, graded overview of risk factors for MSkIs in the military. Experts with a multidisciplinary background, from a total of seven nations as part of the NATO Research Task Group, introduced a new prioritizing injury model for the military. The model provides a foundation for understanding which risk factors would be most important to address and in which order when an intervention is planned.
Availability of data and materials
All data generated or analyzed in this review are included in the published article.
Abbreviations
- BCT:
-
Basis combat training
- DNBI:
-
Disease and nonbattle injury
- IET:
-
Initial entry training
- MSkIs:
-
Musculoskeletal injuries
- MOS:
-
Military occupational specialties
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- RTG:
-
Research Task Group
- STO:
-
Science and Technology Organization
References
No authors listed. Absolute and relative morbidity burdens attributable to various illnesses and injuries, active component, U.S. Armed Forces, 2018. MSMR. 2019;26(5):2–10.
Dijksma I, Bekkers M, Spek B, Lucas C, Stuiver M. Epidemiology and financial burden of musculoskeletal injuries as the leading health problem in the military. Mil Med. 2020;185(3–4):e480–6.
Orr RM, Johnston V, Coyle J, Pope R. Reported load carriage injuries of the Australian army soldier. J Occup Rehabil. 2015;25(2):316–22.
Sammito S. Direct and indirect costs caused by accidents at workplace sport activities. Präv Gesundheitsf. 2011;6(4):245–8.
Strowbridge NF, Burgess KR. Sports and training injuries in British soldiers: the Colchester Garrison Sports Injury and Rehabilitation Centre. J R Army Med Corps. 2002;148(3):236–43.
Wardle SL, Greeves JP. Mitigating the risk of musculoskeletal injury: A systematic review of the most effective injury prevention strategies for military personnel. J Sci Med Sport. 2017;20(Suppl 4):S3–10.
Reis JP, Trone DW, Macera CA, Rauh MJ. Factors associated with discharge during marine corps basic training. Mil Med. 2007;172(9):936–41.
Darakjy S, Marin RE, Knapik JJ, Jones BH. Injuries and illnesses among armor brigade soldiers during operational training. Mil Med. 2006;171(11):1051–6.
Patel AA, Hauret KG, Taylor BJ, Jones BH. Non-battle injuries among U.S. Army soldiers deployed to Afghanistan and Iraq, 2001–2013. J Safety Res. 2017;60:29–34.
Belmont PJ Jr, Goodman GP, Waterman B, DeZee K, Burks R, Owens BD. Disease and nonbattle injuries sustained by a U.S. Army Brigade Combat Team during Operation Iraqi Freedom. Mil Med. 2010;175(7):469–76.
Goodman GP, Schoenfeld AJ, Owens BD, Dutton JR, Burks R, Belmont PJ. Non-emergent orthopaedic injuries sustained by soldiers in Operation Iraqi Freedom. J Bone Joint Surg Am. 2012;94(8):728–35.
Lincoln AE, Smith GS, Amoroso PJ, Bell NS. The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work. 2002;18(2):99–113.
Bergman BP, Miller SA. Equal opportunities, equal risks? Overuse injuries in female military recruits. J Public Health Med. 2001;23(1):35–9.
Taanila H, Hemminki AJM, Suni JH, Pihlajamäki H, Parkkari J. Low physical fitness is a strong predictor of health problems among young men: a follow-up study of 1411 male conscripts. BMC Public Health. 2011;11:590.
de la Motte SJ, Lisman P, Gribbin TC, Murphy K, Deuster PA. Systematic review of the association between physical fitness and musculoskeletal injury risk: part 3—flexibility, power, speed, balance, and agility. J Strength Cond Res. 2017;33(6):1723–35.
Lisman PJ, de la Motte SJ, Gribbin TC, Jaffin DP, Murphy K, Deuster PA. A systematic review of the association between physical fitness and musculoskeletal injury risk: part 1—cardiorespiratory endurance. J Strength Cond Res. 2017;31(6):1744–57.
Knapik J, Steelman R. Risk factors for injuries during military static-line airborne operations: a systematic review and meta-analysis. J Athl Train. 2016;51(11):962–80.
Molloy JM. Factors influencing running-related musculoskeletal injury risk among U.S. Military Recruits. Mil Med. 2016;181(6):512–23.
Knapik JJ. The importance of physical fitness for injury prevention: part 1. J Spec Oper Med. 2015;15(1):123–7.
Knapik JJ. The importance of physical fitness for injury prevention: part 2. J Spec Oper Med. 2015;15(2):112–5.
Bulzacchelli MT, Sulsky SI, Rodriguez-Monguio R, Karlsson LH, Hill MOT. Injury during U.S. Army basic combat training: a systematic review of risk factor studies. Am J Prev Med. 2014;47(6):813–22.
Wentz L, Liu PY, Haymes E, Ilich JZ. Females have a greater incidence of stress fractures than males in both military and athletic populations: a systemic review. Mil Med. 2011;176(4):420–30.
Dao D, Sodhi S, Tabasinejad R, Peterson D, Ayeni OR, Bhandari M, et al. Serum 25-hydroxyvitamin D levels and stress fractures in military personnel: a systematic review and meta-analysis. Am J Sports Med. 2015;43(8):2064–72.
Bedno SA, Jackson R, Feng X, Walton IL, Boivin MR, Cowan DN. Meta-analysis of cigarette smoking and musculoskeletal injuries in military training. Med Sci Sports Exerc. 2017;49(11):2191–7.
Tomes CD, Sawyer S, Orr R, Schram B. Ability of fitness testing to predict injury risk during initial tactical training: a systematic review and meta-analysis. Inj Prev. 2020;26(1):67–81.
Knapik JJ, Steelman R. Risk factors for injuries during airborne static line operations. J Spec Oper Med. 2014;14(3):95–7.
Bell NS, Mangione TW, Hemenway D, Amoroso PJ, Jones BH. High injury rates among female army trainees: a function of gender? Am J Prev Med. 2000;18(3 Suppl):141–6.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331(7524):1064–5.
Dixon SJ, Creaby MW, Allsopp AJ. Comparison of static and dynamic biomechanical measures in military recruits with and without a history of third metatarsal stress fracture. Clin Biomech (Bristol, Avon). 2006;21(4):412–9.
Waterman BR, Gun B, Bader JO, Orr JD, Belmont PJ. Epidemiology of lower extremity stress fractures in the United States Military. Mil Med. 2016;181(10):1308–13.
Itskoviz D, Marom T, Ostfeld I. Trends of stress fracture prevalence among Israel Defense Forces basic trainees. Mil Med. 2011;176(1):56–9.
Jones SB, Knapik JJ, Jones BH. Seasonal variations in injury rates in U.S. Army ordnance training. Mil Med. 2008;173(4):362–8.
Jones BH, Hauret KG, Dye SK, Hauschild VD, Rossi SP, Richardson MD, Friedl KE. Impact of physical fitness and body composition on injury risk among active young adults: a study of army trainees. J Sci Med Sport. 2017;20(Suppl 4):S17–22.
Bedno SA, Nelson DA, Kurina LM, Choi YS. Gender differences in the associations of body mass index, physical fitness and tobacco use with lower extremity musculoskeletal injuries among new US Army soldiers. Inj Prev. 2019;25(4):295–300.
Kuikka PI, Pihlajamäki HK, Mattila VM. Knee injuries related to sports in young adult males during military service—incidence and risk factors. Scand J Med Sci Sports. 2013;23(3):281–7.
Mattila VM, Kuronen P, Pihlajamäki H. Nature and risk factors of injury hospitalization in young adults: a follow-up of 135,987 military conscripts. Scand J Public Health. 2007;35(4):418–23.
Mattila VM, Niva M, Kiuru M, Pihlajamäki H. Risk factors for bone stress injuries: a follow-up study of 102,515 person-years. Med Sci Sports Exerc. 2007;39(7):1061–6.
Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamäki HK. Stress injuries of the calcaneus detected with magnetic resonance imaging in military recruits. J Bone Joint Surg Am. 2006;88(10):2237–42.
Craig SC, Lee T. Attention to detail: injuries at altitude among U.S. army military static line parachutists. Mil Med. 2000;165(4):268–71.
Packnett ER, Niebuhr DW, Bedno SA, Cowan DN. Body mass index, medical qualification status, and discharge during the first year of US Army service. Am J Clin Nutr. 2011;93(3):608–14.
Sulsky SI, Bulzacchelli MT, Zhu L, Karlsson L, McKinnon CJ, Hill OT, Kardouni JR. Risk factors for training-related injuries during U.S. Army Basic Combat Training. Mil Med. 2018;183(suppl_1):55–65.
Activity AMS. Relationship between body mass index and musculoskeletal system and connective tissue disorders, US Army, 1990–1999. Med Surveill Mon Rep. 2000;6:2–10.
Cameron KL, Owens BD, DeBerardino TM. Incidence of ankle sprains among active-duty members of the United States Armed Services from 1998 through 2006. J Athl Train. 2010;45(1):29–38.
Montain SJ, McGraw SM, Ely MR, Grier TL, Knapik JJ. A retrospective cohort study on the influence of UV index and race/ethnicity on risk of stress and lower limb fractures. BMC Musculoskelet Disord. 2013;14:135.
Knapik JJ, Sharp MA, Montain SJ. Association between stress fracture incidence and predicted body fat in United States Army Basic Combat Training recruits. BMC Musculoskelet Disord. 2018;19(1):161.
Knapik J, Montain SJ, McGraw S, Grier T, Ely M, Jones BH. Stress fracture risk factors in basic combat training. Int J Sports Med. 2012;33(11):940–6.
Hruby A, Bulathsinhala L, McKinnon CJ, Hill OT, Montain SJ, Young AJ, et al. BMI and lower extremity injury in U.S. army soldiers, 2001–2011. Am J Prev Med. 2016;50(6):e163–71.
Bulathsinhala L, Hughes JM, McKinnon CJ, Kardouni JR, Guerriere KI, Popp KL, et al. Risk of stress fracture varies by race/ethnic origin in a cohort study of 1.3 million US Army soldiers. J Bone Miner Res. 2017;32(7):1546–53.
Hughes JM, McKinnon CJ, Taylor KM, Kardouni JR, Bulathsinhala L, Guerriere KI, et al. Nonsteroidal anti-inflammatory drug prescriptions are associated with increased stress fracture diagnosis in the US Army population. J Bone Miner Res. 2019;34(3):429–36.
Sillanpää P, Mattila VM, Iivonen T, Visuri T, Pihlajamäki H. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–11.
Canham-Chervak M. The Association of Health Risk Behaviors and Training-related Injury Among U.S. Army Basic Trainees. 2006. http://www.dtic.mil/get-tr-doc/pdf?AD=ADA568679. Accessed 14 Feb 2019.
Chatzipapas CN, Drosos GI, Kazakos KI, Tripsianis G, Iatrou C, Verettas DAJ. Stress fractures in military men and bone quality related factors. Int J Sports Med. 2008;29(11):922–6.
Cosio-Lima L, Brown K, Reynolds KL, Gregg R, Perry RA Jr. Injury and illness incidence in a Sergeants Major Academy class. Mil Med. 2013;178(7):735–41.
Lappe J, Davies K, Recker R, Heaney R. Quantitative ultrasound: use in screening for susceptibility to stress fractures in female army recruits. J Bone Miner Res. 2005;20(4):571–8.
Lappe JM, Stegman MR, Recker RR. The impact of lifestyle factors on stress fractures in female Army recruits. Osteoporos Int. 2001;12(1):35–42.
Robinson M, Siddall A, Bilzon J, Thompson D, Greeves J, Izard R, et al. Low fitness, low body mass and prior injury predict injury risk during military recruit training: a prospective cohort study in the British Army. BMJ Open Sport Exerc Med. 2016;2(1):e000100.
Schneider GA, Bigelow C, Amoroso PJ. Evaluating risk of re-injury among 1214 army airborne soldiers using a stratified survival model. Am J Prev Med. 2000;18(3 Suppl):156–63.
Taanila HP, Suni JH, Pihlajamaki HK, Mattila VM, Ohrankammen O, Vuorinen P, Parkkari JP. Predictors of low back pain in physically active conscripts with special emphasis on muscular fitness. Spine J. 2012;12(9):737–48.
Wilkinson DM, Blacker SD, Richmond VL, Horner FE, Rayson MP, Spiess A, Knapik JJ. Injury rates and injury risk factors among British army infantry soldiers: final report. Med Sci Sports Exer. 2009;42:283–4.
Givon U, Friedman E, Reiner A, Vered I, Finestone A, Shemer J. Stress fractures in the Israeli Defense Forces from 1995 to 1996. Clin Orthop Relat Res. 2000;373:227–32.
Moran DS, Finestone AS, Arbel Y, Shabshin N, Laor A. A simplified model to predict stress fracture in young elite combat recruits. J Strength Cond Res. 2012;26(9):2585–92.
Moran DS, Heled Y, Arbel Y, Israeli E, Finestone AS, Evans RK, et al. Dietary intake and stress fractures among elite male combat recruits. J Int Soc Sports Nutr. 2012;9(1):6.
Cosman F, Ruffing J, Zion M, Uhorchak J, Ralston S, Tendy S, et al. Determinants of stress fracture risk in United States Military Academy cadets. Bone. 2013;55(2):359–66.
Sanchez-Santos MT, Davey T, Leyland KM, Allsopp AJ, Lanham-New SA, Judge A, et al. Development of a prediction model for stress fracture during an intensive Physical Training Program: The Royal Marines Commandos. Orthop J Sports Med. 2017;5(7):2325967117716381.
Dash N, Kushwaha A. Stress fractures—a prospective study amongst recruits. Med J Armed Forces India. 2012;68(2):118–22.
Kovcan B, Vodicar J, Šimenko J, Videmšek M, Pori P, Vedran H. Retrospective and cross-sectional analysis of physical training-related musculoskeletal injuries in Slovenian Armed Forces. Mil Med. 2019;184(1–2):e195–9.
Wyss T, Roos L, Hofstetter MC, Frey F, Mäder U. Impact of training patterns on injury incidences in 12 Swiss Army basic military training schools. Mil Med. 2014;179(1):49–55.
Altarac M, Gardner JW, Popovich RM, Potter R, Knapik JJ, Jones BH. Cigarette smoking and exercise-related injuries among young men and women. Am J Prev Med. 2000;18(3 Suppl):96–102.
Anderson MK, Grier T, Canham-Chervak M, Bushman TT, Jones BH. Occupation and other risk factors for injury among enlisted U.S. army soldiers. Public Health. 2015;129(5):531–8.
Anderson MK, Grier T, Dada EO, Canham-Chervak M, Jones BH. The role of gender and physical performance on injuries: an army study. Am J Prev Med. 2017;52(5):e131–8.
Bedno SA, Cowan DN, Urban N, Niebuhr DW. Effect of pre-accession physical fitness on training injuries among US Army recruits. Work. 2013;44(4):509–15.
Brooks RD, Grier T, Dada EO, Jones BH. The combined effect of cigarette smoking and fitness on injury risk in men and women. Nicotine Tob Res. 2019;21(12):1621–8.
Cowan DN, Bedno SA, Urban N, Lee DS, Niebuhr DW. Step test performance and risk of stress fractures among female army trainees. Am J Prev Med. 2012;42(6):620–4.
Cowan DN, Bedno SA, Urban N, Yi B, Niebuhr DW. Musculoskeletal injuries among overweight army trainees: incidence and health care utilization. Occup Med (Lond). 2011;61(4):247–52.
Davey T, Lanham-New SA, Shaw AM, Cobley R, Allsopp AJ, Hajjawi MOR, et al. Fundamental differences in axial and appendicular bone density in stress fractured and uninjured royal marine recruits—a matched case-control study. Bone. 2015;73:120–6.
Fallowfield JL, Leiper RG, Shaw AM, Whittamore DR, Lanham-New SA, Allsopp AJ, et al. Risk of injury in Royal Air Force Training: does sex really matter? Mil Med. 2018. https://doi.org/10.1093/milmed/usy177.
Grier TL, Canham-Chervak M, Anderson MK, Bushman TT, Jones BH. Effects of physical training and fitness on running injuries in physically active young men. J Strength Cond Res. 2017;31(1):207–16.
Grier TL, Knapik JJ, Canada S, Canham-Chervak M, Jones BH. Risk factors associated with self-reported training-related injury before arrival at the US Army ordnance school. Public Health. 2010;124(7):417–23.
Kelly EW, Jonson SR, Cohen ME, Shaffer R. Stress fractures of the pelvis in female navy recruits: an analysis of possible mechanisms of injury. Mil Med. 2000;165(2):142–6.
Knapik JJ, Brosch LC, Venuto M, Swedler DI, Bullock SH, Gaines LS, et al. Effect on injuries of assigning shoes based on foot shape in air force basic training. Am J Prev Med. 2010;38(1 Suppl):S197-211.
Knapik JJ, Graham B, Cobbs J, Thompson D, Steelman R, Jones BH. A prospective investigation of injury incidence and injury risk factors among Army recruits in military police training. BMC Musculoskelet Disord. 2013;14:32.
Knapik JJ, Graham BS, Rieger J, Steelman R, Pendergrass T. Activities associated with injuries in initial entry training. Mil Med. 2013;178(5):500–6.
Knapik JJ, Jones SB, Darakjy S, Hauret KG, Nevin R, Grier T, Jones BH. Injuries and injury risk factors among members of the United States Army Band. Am J Ind Med. 2007;50(12):951–61.
Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. Risk factors for training-related injuries among men and women in basic combat training. Med Sci Sports Exerc. 2001;33(6):946–54.
Knapik JJ, Spiess A, Swedler D, Grier T, Darakjy S, Amoroso P, et al. Injury risk factors in parachuting and acceptability of the parachute ankle brace. Aviat Space Environ Med. 2008;79(7):689–94.
Knapik JJ, Swedler D, Grier T, Hauret KG, Bullock S, Williams K, et al. Injury reduction effectiveness of prescribing running shoes based on foot shape in basic combat training: Technical Report No. 12-MA-05SB-08. Aberdeen Proving Ground, MD; 2008.
Knapik JJ, Trone D, Swedler DI, Villasenor A, Schmied E, Bullock S, Jones BH. Injury reduction effectiveness of assigning running shoes based on foot shape in Marine Corps basic training: No. 12-MA-05SBA-08B. Aberdeen Proving Ground, MD; 2009.
Korvala J, Hartikka H, Pihlajamäki H, Solovieva S, Ruohola JP, Sahi T, et al. Genetic predisposition for femoral neck stress fractures in military conscripts. BMC Genet. 2010;11:95.
Lauder TD, Dixit S, Pezzin LE, Williams MV, Campbell CS, Davis GD. The relation between stress fractures and bone mineral density: evidence from active-duty Army women. Arch Phys Med Rehabil. 2000;81(1):73–9.
Munnoch K, Bridger RS. Smoking and injury in Royal Marines’ training. Occup Med (Lond). 2007;57(3):214–6.
Nagai T, Lovalekar M, Wohleber MF, Perlsweig KA, Wirt MD, Beals K. Poor anaerobic power/capability and static balance predicted prospective musculoskeletal injuries among Soldiers of the 101st Airborne (Air Assault) Division. J Sci Med Sport. 2017;20(Suppl 4):S11–6.
Pihlajamäki H, Parviainen M, Kyröläinen H, Kautiainen H, Kiviranta I. Regular physical exercise before entering military service may protect young adult men from fatigue fractures. BMC Musculoskelet Disord. 2019;20(1):126.
Psaila M, Ranson C. Risk factors for lower leg, ankle and foot injuries during basic military training in the Maltese Armed Forces. Phys Ther Sport. 2017;24:7–12.
Rappole C, Grier T, Anderson MK, Hauschild V, Jones BH. Associations of age, aerobic fitness, and body mass index with injury in an operational Army brigade. J Sci Med Sport. 2017;20(Suppl 4):S45-50.
Reynolds K, Cosio-Lima L, Bovill M, Tharion W, Williams J, Hodges T. A comparison of injuries, limited-duty days, and injury risk factors in infantry, artillery, construction engineers, and special forces soldiers. Mil Med. 2009;174(7):702–8.
Reynolds K, Cosio-Lima L, Creedon J, Gregg R, Zigmont T. Injury occurrence and risk factors in construction engineers and combat artillery soldiers. Mil Med. 2002;167(12):971–7.
Reynolds K, Williams J, Miller C, Mathis A, Dettori J. Injuries and risk factors in an 18-day marine winter mountain training exercise. Mil Med. 2000;165(12):905–10.
Roos L, Boesch M, Sefidan S, Frey F, Mäder U, Annen H, et al. Adapted marching distances and physical training decrease recruits’ injuries and attrition. Mil Med. 2015;180(3):329–36.
Ruohola JP, Laaksi I, Ylikomi T, Haataja R, Mattila VM, Sahi T, et al. Association between serum 25(OH)D concentrations and bone stress fractures in Finnish young men. J Bone Miner Res. 2006;21(9):1483–8.
Scheinowitz M, Yanovich R, Sharvit N, Arnon M, Moran DS. Effect of cardiovascular and muscular endurance is not associated with stress fracture incidence in female military recruits: a 12-month follow up study. J Basic Clin Physiol Pharmacol. 2017;28(3):219–24.
Sharma J, Heagerty R, Dalal S, Banerjee B, Booker T. Risk factors associated with musculoskeletal injury: a prospective study of British infantry recruits. Curr Rheumatol Rev. 2019;15(1):50–8.
Sharma J, Golby J, Greeves J, Spears IR. Biomechanical and lifestyle risk factors for medial tibia stress syndrome in army recruits: a prospective study. Gait Posture. 2011;33(3):361–5.
Taanila H, Suni JH, Kannus P, Pihlajamaki H, Ruohola JP, Viskari J, et al. Risk factors of acute and overuse musculoskeletal injuries among young conscripts: a population-based cohort study. BMC Musculoskelet Disord. 2015;16:104.
Trone DW, Cipriani DJ, Raman R, Wingard DL, Shaffer RA, Macera CA. Self-reported smoking and musculoskeletal overuse injury among male and female U.S. marine corps recruits. Mil Med. 2014;179(7):735–43.
Wang X, Wang P, Zhou W. Risk factors of military training-related injuries in recruits of Chinese People’s Armed Police Forces. Chin J Traumatol. 2003;6(1):12–7.
Wunderlin S, Roos L, Roth R, Faude O, Frey F, Wyss T. Trunk muscle strength tests to predict injuries, attrition and military ability in soldiers. J Sports Med Phys Fitness. 2015;55(5):535–43.
Zhao L, Chang Q, Huang T, Huang C. Prospective cohort study of the risk factors for stress fractures in Chinese male infantry recruits. J Int Med Res. 2016;44(4):787–95.
Shaffer RA, Rauh MJ, Brodine SK, Trone DW, Macera CA. Predictors of stress fracture susceptibility in young female recruits. Am J Sports Med. 2006;34(1):108–15.
Cameron KL, Mountcastle SB, Nelson BJ, DeBerardino TM, Duffey ML, Svoboda SJ, et al. History of shoulder instability and subsequent injury during four years of follow-up: a survival analysis. J Bone Joint Surg Am. 2013;95(5):439–45.
Evans R, Reynolds K, Creedon J, Murphy M. Incidence of acute injury related to fitness testing of U.S. Army personnel. Mil Med. 2005;170(12):1005–11.
Finestone A, Milgrom C, Wolf O, Petrov K, Evans R, Moran D. Epidemiology of metatarsal stress fractures versus tibial and femoral stress fractures during elite training. Foot Ankle Int. 2011;32(1):16–20.
Garnock C, Witchalls J, Newman P. Predicting individual risk for medial tibial stress syndrome in navy recruits. J Sci Med Sport. 2018;21(6):586–90.
George SZ, Childs JD, Teyhen DS, Wu SS, Wright AC, Dugan JL, et al. Predictors of occurrence and severity of first time low back pain episodes: findings from a military inception cohort. PLoS ONE. 2012;7(2):e30597.
Hill OT, Bulathsinhala L, Scofield DE, Haley TF, Bernasek TL. Risk factors for soft tissue knee injuries in active duty U.S. army soldiers, 2000–2005. Mil Med. 2013;178(6):676–82.
Knapik JJ, Graham B, Cobbs J, Thompson D, Steelman R, Jones BH. A prospective investigation of injury incidence and risk factors among army recruits in combat engineer training. J Occup Med Toxicol. 2013;8(1):5.
Kucera KL, Marshall SW, Wolf SH, Padua DA, Cameron KL, Beutler AI. Association of injury history and incident injury in Cadet Basic Military Training. Med Sci Sports Exerc. 2016;48(6):1053–61.
Lisman P, O’Connor FG, Deuster PA, Knapik JJ. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013;45(4):636–43.
Monnier A, Larsson H, Nero H, Djupsjöbacka M, Äng BO. A longitudinal observational study of back pain incidence, risk factors and occupational physical activity in Swedish marine trainees. BMJ Open. 2019;9(5):e025150.
Rice H, Nunns M, House C, Fallowfield J, Allsopp A, Dixon S. A narrow bimalleolar width is a risk factor for ankle inversion injury in male military recruits: a prospective study. Clin Biomech (Bristol, Avon). 2017;41:14–9.
Roy TC, Songer T, Ye F, LaPorte R, Grier T, Anderson M, et al. Physical training risk factors for musculoskeletal injury in female soldiers. Mil Med. 2014;179(12):1432–8.
Scott SA, Simon JE, Van Der Pol B, Docherty CL. Risk factors for sustaining a lower extremity injury in an Army Reserve Officer Training Corps Cadet Population. Mil Med. 2015;180(8):910–6.
Taanila H, Suni J, Pihlajamäki H, Mattila VM, Ohrankämmen O, Vuorinen P, et al. Aetiology and risk factors of musculoskeletal disorders in physically active conscripts: a follow-up study in the Finnish defence forces. BMC Musculoskelet Disord. 2010;11:146.
Merkel D, Moran DS, Yanovich R, Evans RK, Finestone AS, Constantini N, et al. The association between hematological and inflammatory factors and stress fractures among female military recruits. Med Sci Sports Exerc. 2008;40(11 Suppl):S691–7.
Moran DS, Israeli E, Evans RK, Yanovich R, Constantini N, Shabshin N, et al. Prediction model for stress fracture in young female recruits during basic training. Med Sci Sports Exerc. 2008;40(11 Suppl):S636–44.
Burgi AA, Gorham ED, Garland CF, Mohr SB, Garland FC, Zeng K, et al. High serum 25-hydroxyvitamin D is associated with a low incidence of stress fractures. J Bone Miner Res. 2011;26(10):2371–7.
Davey T, Lanham-New SA, Shaw AM, Hale B, Cobley R, Berry JL, et al. Low serum 25-hydroxyvitamin D is associated with increased risk of stress fracture during royal marine recruit training. Osteoporos Int. 2016;27(1):171–9.
Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791–6.
Schermann H, Karakis I, Ankory R, Kadar A, Yoffe V, Shlaifer A, et al. Musculoskeletal injuries among female soldiers working with dogs. Mil Med. 2018;183(9–10):e343–8.
Constantini N, Finestone AS, Hod N, Shub I, Heinemann S, Foldes AJ, et al. Equipment modification is associated with fewer stress fractures in female Israel border police recruits. Mil Med. 2010;175(10):799–804.
Konitzer LN, Fargo MV, Brininger TL, Lim RM. Association between back, neck, and upper extremity musculoskeletal pain and the individual body armor. J Hand Ther. 2008;21(2):143–8 (quiz 149).
Rappole C, Chervak MC, Grier T, Anderson MK, Jones BH. Factors associated with lower extremity training-related injuries among Enlisted Women in U.S. army operational units. J Mil Veterans Healt. 2018;26(1):18–28.
Roy TC, Ritland BM, Knapik JJ, Sharp MA. Lifting tasks are associated with injuries during the early portion of a deployment to Afghanistan. Mil Med. 2012;177(6):716–22.
Roy TC, Ritland BM, Sharp MA. A description of injuries in men and women while serving in Afghanistan. Mil Med. 2015;180(2):126–31.
Roy TC. Diagnoses and mechanisms of musculoskeletal injuries in an infantry brigade combat team deployed to Afghanistan evaluated by the brigade physical therapist. Mil Med. 2011;176(8):903–8.
Schwartz O, Malka I, Olsen CH, Dudkiewicz I, Bader T. Overuse injuries in the IDF’s Combat Training Units: rates, types, and mechanisms of injury. Mil Med. 2018;183(3–4):e196-200.
Sefton JM, Lohse KR, McAdam JS. Prediction of injuries and injury types in Army Basic Training, Infantry, Armor, and Cavalry Trainees using a common fitness screen. J Athl Train. 2016;51(11):849–57.
Sharma J, Dixon J, Dalal S, Heagerty R, Spears I. Musculoskeletal injuries in British army recruits: a prospective study of incidence in different Infantry Regiments. J R Army Med Corps. 2017;163(6):406–11.
Skeehan CD, Tribble DR, Sanders JW, Putnam SD, Armstrong AW, Riddle MS. Nonbattle injury among deployed troops: an epidemiologic study. Mil Med. 2009;174(12):1256–62.
Beck TJ, Ruff CB, Shaffer RA, Betsinger K, Trone DW, Brodine SK. Stress fracture in military recruits: gender differences in muscle and bone susceptibility factors. Bone. 2000;27(3):437–44.
Canham-Chervak M, Knapik JJ, Hauret K, Cuthie J, Craig S. Determining physical fitness criteria for entry into Army Basic Combat Training: can these criteria be based on injury risk? 2000. http://www.dtic.mil/dtic/tr/fulltext/u2/a374717.pdf. Accessed 1 Mar 2014.
Dixon S, Nunns M, House C, Rice H, Mostazir M, Stiles V, et al. Prospective study of biomechanical risk factors for second and third metatarsal stress fractures in military recruits. J Sci Med Sport. 2019;22(2):135–9.
Havenetidis K, Paxinos T. Risk factors for musculoskeletal injuries among Greek Army officer cadets undergoing Basic Combat Training. Mil Med. 2011;176(10):1111–6.
Henderson NE, Knapik JJ, Shaffer SW, McKenzie TH, Schneider GM. Injuries and injury risk factors among men and women in U.S. army combat medic advanced individual training. Mil Med. 2000;165(9):647–52.
Knapik JJ, Darakjy S, Hauret KG, Canada S, Scott S, Rieger W, et al. Increasing the physical fitness of low-fit recruits before basic combat training: an evaluation of fitness, injuries, and training outcomes. Mil Med. 2006;171(1):45–54.
Knapik JJ, Jones SB, Darakjy S, Hauret KG, Bullock SH, Sharp MA, et al. Injury rates and injury risk factors among U.S. army wheel vehicle mechanics. Mil Med. 2007;172(9):988–96.
Ma JZ, Cui SF, Hu F, Lu QJ, Li W. Incidence and characteristics of meniscal injuries in cadets at a military school, 2013–2015. J Athl Train. 2016;51(11):876–9.
Mahieu NN, Witvrouw E, Stevens V, Van Tiggelen D, Roget P. Intrinsic risk factors for the development of achilles tendon overuse injury: a prospective study. Am J Sports Med. 2006;34(2):226–35.
Moran DS, Evans R, Arbel Y, Luria O, Hadid A, Yanovich R, et al. Physical and psychological stressors linked with stress fractures in recruit training. Scand J Med Sci Sports. 2013;23(4):443–50.
Nunns M, House C, Rice H, Mostazir M, Davey T, Stiles V, et al. Four biomechanical and anthropometric measures predict tibial stress fracture: a prospective study of 1065 Royal Marines. Br J Sports Med. 2016;50(19):1206–10.
Nye NS, Pawlak MT, Webber BJ, Tchandja JN, Milner MR. Description and rate of musculoskeletal injuries in air force basic military trainees, 2012–2014. J Athl Train. 2016;51(11):858–65.
Owens B, Mountcastle S, White D. Racial differences in tendon rupture incidence. Int J Sports Med. 2007;28(7):617–20.
Parr JJ, Clark NC, Abt JP, Kresta JY, Keenan KA, Kane SF, et al. Residual impact of previous injury on musculoskeletal characteristics in special forces operators. Orthop J Sports Med. 2015;3(11):2325967115616581.
Rabin A, Kozol Z, Finestone AS. Limited ankle dorsiflexion increases the risk for mid-portion Achilles tendinopathy in infantry recruits: a prospective cohort study. J Foot Ankle Res. 2014;7(1):48.
Sobhani V, Shakibaee A, Khatibi Aghda A, Emami Meybodi MK, Delavari A, Jahandideh D. Studying the relation between medial tibial stress syndrome and anatomic and anthropometric characteristics of military male personnel. Asian J Sports Med. 2015;6(2):e23811.
Trybulec B, Majchrzak E. Injuries and factors determining their occurrence in paratroopers of airborne forces. Balt J Health Phys A. 2016;8(2):78–86.
Heebner NR, Abt JP, Lovalekar M, Beals K, Sell TC, Morgan J, et al. Physical and performance characteristics related to unintentional musculoskeletal injury in special forces operators: a prospective analysis. J Athl Train. 2017;52(12):1153–60.
Sell TC, Clark NC, Wood D, Abt JP, Lovalekar M, Lephart SM. Single-leg balance impairments persist in fully operational military special forces operators with a previous history of low back pain. Orthop J Sports Med. 2014;2(5):2325967114532780.
Allsopp AJ, Scarpello EG, Andrews S, Pethybridge RJ. Survival of the fittest? The scientific basis for the Royal Navy pre-joining fitness test. J R Nav Med Serv. 2003;89(1):11–8.
Billings CE. Epidemiology of injuries and illnesses during the United States Air Force Academy 2002 Basic Cadet Training program: documenting the need for prevention. Mil Med. 2004;169(8):664–70.
Blacker SD, Wilkinson DM, Bilzon JLJ, Rayson MP. Risk factors for training injuries among British Army recruits. Mil Med. 2008;173(3):278–86.
Havenetidis K, Paxinos T, Kardaris D, Bissas A. Prognostic potential of body composition indices in detecting risk of musculoskeletal injury in army officer cadet profiles. Phys Sports Med. 2017;45(2):114–9.
Kodesh E, Shargal E, Kislev-Cohen R, Funk S, Dorfman L, Samuelly G, et al. Examination of the effectiveness of predictors for musculoskeletal injuries in female soldiers. J Sports Sci Med. 2015;14(3):515–21.
Kupferer KR, Bush DM, Cornell JE, Lawrence VA, Alexander JL, Ramos RG, et al. Femoral neck stress fracture in Air Force basic trainees. Mil Med. 2014;179(1):56–61.
Waterman BR, Belmont PJ Jr, Cameron KL, DeBerardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38(4):797–803.
Gundlach N, Sammito S, Böckelmann I. Risk factors for accidents during sports while serving in German armed forces. Sportverletz Sportschaden. 2012;26(1):45–8 ((in German)).
Finestone A, Milgrom C, Evans R, Yanovich R, Constantini N, Moran DS. Overuse injuries in female infantry recruits during low-intensity basic training. Med Sci Sports Exerc. 2008;40(11 Suppl):S630–5.
Krauss MR, Garvin NU, Boivin MR, Cowan DN. Excess stress fractures, musculoskeletal injuries, and health care utilization among unfit and overweight female army trainees. Am J Sports Med. 2017;45(2):311–6.
Hughes CD, Weinrauch PCL. Military static line parachute injuries in an Australian commando battalion. ANZ J Surg. 2008;78(10):848–52.
Burne SG, Khan KM, Boudville PB, Mallet RJ, Newman PM, Steinman LJ, et al. Risk factors associated with exertional medial tibial pain: a 12 month prospective clinical study. Br J Sports Med. 2004;38(4):441–5.
Rauh MJ, Macera CA, Trone DW, Reis JP, Shaffer RA. Selected static anatomic measures predict overuse injuries in female recruits. Mil Med. 2010;175(5):329–35.
Keenan KA, Wohleber MF, Perlsweig KA, Baldwin TM, Caviston M, Lovalekar M, et al. Association of prospective lower extremity musculoskeletal injury and musculoskeletal, balance, and physiological characteristics in Special Operations Forces. J Sci Med Sport. 2017;20(Suppl 4):S34–9.
Esterman A, Pilotto L. Foot shape and its effect on functioning in Royal Australian Air Force recruits. Part 1: prospective cohort study. Mil Med. 2005;170(7):623–8.
Hetsroni I, Finestone A, Milgrom C, Ben Sira D, Nyska M, Radeva-Petrova D, et al. Prospective biomechanical study of the association between foot pronation and the incidence of anterior knee pain among military recruits. J Bone Joint Surg Br. 2006;88(7):905–8.
Levy JC, Mizel MS, Wilson LS, Fox W, McHale K, Taylor DC, et al. Incidence of foot and ankle injuries in West Point cadets with pes planus compared to the general cadet population. Foot Ankle Int. 2006;27(12):1060–4.
Yates B, White S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am J Sports Med. 2004;32(3):772–80.
Roy TC, Knapik JJ, Ritland BM, Murphy N, Sharp MA. Risk factors for musculoskeletal injuries for soldiers deployed to Afghanistan. Aviat Space Environ Med. 2012;83(11):1060–6.
Grier TL, Morrison S, Knapik JJ, Canham-Chervak M, Jones BH. Risk factors for injuries in the U.S. Army Ordnance School. Mil Med. 2011;176(11):1292–9.
Hall LJ. Relationship between 1.5-mile run time, injury risk and training outcome in British army recruits. J R Army Med Corps. 2017;163(6):376–82.
Hauret KG, Steelman RA, Pierce JR, Alemany JA, Sharp MA, Foulis SA, et al. Association of Performance on the Occupational Physical Assessment Test with Injuries and Attrition During Initial Entry Training – OPAT Phase I: PHR # S.0047229–18b. Aberdeen Proving Ground, MD: U.S. Army Public Health Center. DTIC: AD1061860; 2018.
Heller R, Stammers H. Running to breaking point? The relationship between 1.5-mile run time and injury risk in female recruits during British army basic training. J R Army Med Corps. 2020;166(E):e3–7.
Knapik JJ, Hauret KG, Arnold S, Canham-Chervak M, Mansfield AJ, Hoedebecke EL, et al. Injury and fitness outcomes during implementation of physical readiness training. Int J Sports Med. 2003;24(5):372–81.
Knapik JJ, Swedler DI, Grier TL, Hauret KG, Bullock SH, Williams KW, et al. Injury reduction effectiveness of selecting running shoes based on plantar shape. J Strength Cond Res. 2009;23(3):685–97.
Martin RC, Grier T, Canham-Chervak M, Bushman TT, Anderson MK, Dada EO, et al. Risk factors for sprains and strains among physically active young men: a US Army study. US Army Med Dep J. 2018;2–18:14–21.
Müller-Schilling L, Gundlach N, Böckelmann I, Sammito S. Physical fitness as a risk factor for injuries and excessive stress symptoms during basic military training. Int Arch Occup Environ Health. 2019;92(6):837–41.
Rauh MJ, Macera CA, Trone DW, Shaffer RA, Brodine SK. Epidemiology of stress fracture and lower-extremity overuse injury in female recruits. Med Sci Sports Exerc. 2006;38(9):1571–7.
Rosendal L, Langberg H, Skov-Jensen A, Kjaer M. Incidence of injury and physical performance adaptations during military training. Clin J Sport Med. 2003;13(3):157–63.
Välimäki VV, Alfthan H, Lehmuskallio E, Löyttyniemi E, Sahi T, Suominen H, et al. Risk factors for clinical stress fractures in male military recruits: a prospective cohort study. Bone. 2005;37(2):267–73.
Wyss T, Von Vigier RO, Frey F, Mäder U. The Swiss army physical fitness test battery predicts risk of overuse injuries among recruits. J Sports Med Phys Fitness. 2012;52(5):513–21.
Finestone AS, Milgrom C, Yanovich R, Evans R, Constantini N, Moran DS. Evaluation of the performance of females as light infantry soldiers. Biomed Res Int. 2014;2014:572953.
Gam A, Goldstein L, Karmon Y, Mintser I, Grotto I, Guri A, et al. Comparison of stress fractures of male and female recruits during basic training in the Israeli anti-aircraft forces. Mil Med. 2005;170(8):710–2.
Gemmell IMM. Injuries among female army recruits: a conflict of legislation. J R Soc Med. 2002;95:23–7.
Snedecor MR, Boudreau CF, Ellis BE, Schulman J, Hite M, Chambers BUS. Air force recruit injury and health study. Am J Prev Med. 2000;18(3 Suppl):129–40.
Goss DL, Moore JH, Slivka EM, Hatler BS. Comparison of injury rates between cadets with limb length inequalities and matched control subjects over 1 year of military training and athletic participation. Mil Med. 2006;171(6):522–5.
Knapik JJ, Canham-Chervak M, Hauret K, Laurin MJ, Hoedebecke E, Craig S, et al. Seasonal variations in injury rates during US Army Basic Combat Training. Ann Occup Hyg. 2002;46(1):15–23.
Mattila VM, Parkkari J, Korpela H, Pihlajamäki H. Hospitalisation for injuries among Finnish conscripts in 1990–1999. Accid Anal Prev. 2006;38(1):99–104.
Taanila H, Suni J, Pihlajamäki H, Mattila VM, Ohrankämmen O, Vuorinen P, et al. Musculoskeletal disorders in physically active conscripts: a one-year follow-up study in the Finnish Defence Forces. BMC Musculoskelet Disord. 2009;10:89.
Helton GL, Cameron KL, Zifchock RA, Miller E, Goss DL, Song J, et al. Association between running shoe characteristics and lower extremity injuries in United States military academy cadets. Am J Sports Med. 2019;47(12):2853–62.
Knapik JJ, Hauret KG, Canada S, Marin R, Jones B. Association between ambulatory physical activity and injuries during United States Army Basic Combat Training. J Phys Act Health. 2011;8(4):496–502.
Schuh A, Grier T, Canham-Chervak M, Hauschild V, Roy T, Jones BJ. Risk factors for injury associated with low, moderate, and high mileage road marching in a U.S. Army infantry brigade. J Sci Med Sport. 2017;20:S28–33.
Knapik J, Darakjy S, Scott SJ, Hauret KG, Canada S, Marin R, et al. Evaluation of a standardized physical training program for basic combat training. J Strength Cond Res. 2005;19(2):246–53.
Ivarsson A, Johnson U, Andersen MB, Tranaeus U, Stenling A, Lindwall M. Psychosocial factors and sport injuries: meta-analyses for prediction and prevention. Sports Med. 2017;47(2):353–65.
Junge A. The influence of psychological factors on sports injuries. Review of the literature. Am J Sports Med. 2000;28(5 Suppl):S10–5.
Acknowledgements
The authors would like to thank LTC Dr. Damien Van Tiggelen (Belgium) and Ms. Beatriz Sanz-Bustillo Aguirre (Spain) for their participation and input in the discussion during the HFM-283 meeting in Cologne (Germany) in January 2020.
Funding
No funding was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
SS was responsible for the review and the screening of the articles. KRK, SPR, and WOZ also screened articles. SS was the major contributor in writing the manuscript. All authors discussed the article during a personal meeting in January 2020. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
For this systematic review of the literature, approval from the ethics committee and informed consent by participants was not necessary.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. The views expressed herein are solely those of the authors and do not reflect an endorsement by, or the official policy or position of, the NATO nations represented, including the US Department of Defense.
Supplementary Information
Additional file 1
. MESH search term.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sammito, S., Hadzic, V., Karakolis, T. et al. Risk factors for musculoskeletal injuries in the military: a qualitative systematic review of the literature from the past two decades and a new prioritizing injury model. Military Med Res 8, 66 (2021). https://doi.org/10.1186/s40779-021-00357-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40779-021-00357-w