Abstract
Background
The efficacy and safety of saline versus balanced crystalloid solutions in ICU-patients remains complicated by exceptionally heterogenous study population in past comparative studies. This study sought to compare saline and balanced crystalloids for fluid resuscitation in patients with cardiogenic shock with or without out-of-hospital cardiac arrest (OHCA).
Methods
We retrospectively analyzed 1032 propensity score matched patients with cardiogenic shock from the Munich University Hospital from 2010 to 2022. In 2018, default resuscitation fluid was changed from 0.9% saline to balanced crystalloids. The primary endpoint was defined as 30-day mortality rate.
Results
Patients in the saline group (n = 516) had a similar 30-day mortality rate as patients treated with balanced crystalloids (n = 516) (43.1% vs. 43.0%, p = 0.833), but a higher incidence of new onset renal replacement therapy (30.2% vs 22.7%, p = 0.007) and significantly higher doses of catecholamines. However, OHCA-patients with a lactate level higher than 7.4 mmol/L had a significantly lower 30-day mortality rate when treated with saline (58.6% vs. 79.3%, p = 0.013). In addition, use of balanced crystalloids was independently associated with a higher mortality in the multivariate cox regression analysis after OHCA (hazard ratio 1.43, confidence interval: 1.05–1.96, p = 0.024).
Conclusions
In patients with cardiogenic shock, use of balanced crystalloids was associated with a similar all-cause mortality at 30 days but a lower rate of new onset of renal replacement therapy. In the subgroup of patients after OHCA with severe shock, use of balanced crystalloids was associated with a higher mortality than saline.
Trial registration: LMUshock registry (WHO International Clinical Trials Registry Platform Number DRKS00015860).
Similar content being viewed by others
Background
Fluid resuscitation is one of the most frequently used treatment for critically ill patients in the intensive care unit. Even though practiced since the nineteenth century, larger trials comparing different fluids have been absent until two decades ago [1]. Since then, albumin has been shown to increase mortality among patients suffering from traumatic brain injury [2, 3]. Another colloid, hydroxyethyl starch, has been found to increase the risk of acute kidney injury and death, leaving intensive care physicians with crystalloid fluids to choose from [4, 5]. Saline (0.9% sodium chloride) is the most commonly used crystalloid, but its use was associated with a higher risk of hyperchloremic acidosis, renal failure and in some studies mortality compared to balanced solutions that have a chloride concentration closer to that of blood plasma [6,7,8,9,10]. As subsequent randomized controlled trials failed to reproduce these findings, there is ongoing debate on which crystalloid fluid to use with the latest meta-analysis reporting a high probability that balanced crystalloids reduce mortality compared to saline [1, 6, 11]. However, available evidence is limited to a heterogenic study population with a high prevalence of postoperative patients ranging up to 71% in some studies, whereas the amount of non-operative cardiovascular admissions is either not reported or as low as 5% [6, 9]. Additionally, balanced electrolytes were associated with a higher mortality than saline in patients after traumatic brain injury, but data for patients after non-traumatic brain injury is lacking.
Cardiogenic shock (CS) patients in particular are not only significantly underrepresented in these trials, but have a very high risk of death with a 30-day mortality rate of around 40–50% and a risk of acute kidney injury requiring renal replacement therapy of up to 21% despite latest advances in treatment such as mechanical circulatory support [12,13,14]. Furthermore, these patients commonly require large volumes of intravenous fluids in addition to high doses of catecholamines to maintain sufficient circulation, making them potentially more susceptible to even smaller treatment effects of different fluids. To date, no study has compared different fluid resuscitation strategies in CS patients and specific guideline recommendations are lacking. To the best of our knowledge this is the first study comparing saline and balanced electrolytes in patients with CS with or without out-of-hospital cardiac arrest (OHCA). The primary hypothesis was that the use of balanced electrolytes reduces 30-day all-cause mortality rate in patients with CS.
Methods
Study population
All CS patients treated in the cardiac intensive care unit (ICU) of the Ludwig-Maximilians-University hospital between January 2010 and August 2022 were included in the LMUshock registry (WHO International Clinical Trials Registry Platform Number DRKS00015860). Data collection and analysis was in accordance with the Declaration of Helsinki and German data protection laws. The study was approved by the local ethics committee (IRB number: 18–001). CS was defined by ESC guidelines, the IABP-SHOCK II trial and CULPRIT SHOCK trial [13,14,15]. Telephone follow-up was performed for patients dismissed from the hospital before day 30.
Intravenous fluids
From 2018 on, the default maintenance and resuscitation fluid in our institution was switched from saline (0,9% sodium chloride, B. Braun SE, Melsungen, Germany) to a balanced resuscitation fluid (Jonosteril®, Fresenius Kabi, Bad Homburg, Germany). Jonosteril® is a balanced crystalloid buffered with acetate that has electrolyte concentrations closer to those of blood plasma than saline (Jonosteril®: Na + 137 mmol/l, Cl − 110 mmol/l, K + 4 mmol/l, Ca2 + 1.65 mmol/l, Mg2 + 1.25 mmol/l, acetate 36.8 mmol; Saline: Na + 154 mmol/l, Cl− 154 mmol/l). This decision was driven by the results of the SMART trial and was upheld since then [8]. However, a different choice of resuscitation fluid was allowed at the discretion of the attending intensive care physician. Patients receiving Jonosteril® at the day of admission to ICU were assigned to the balanced group, while patients receiving exclusively unbalanced fluid as resuscitation fluid were assigned to the saline group. Fluids required for dilution of parenteral medication were not analyzed due to missing data. Output data was available as total fluid output including urine, feces and iatrogenic output such as pleuracentesis or dialysis.
Study endpoints and parameters
The primary endpoint was defined as all-cause 30-day mortality rate. Secondary endpoints included time on ICU, serum creatinine, new onset of renal-replacement therapy, time-weighted catecholamine doses (using the formula: dobutamine (mg/h) + 100 × epinephrine (mg/h) + 100 × norepinephrine (mg/h) as previously described), blood pressure, arterial blood pH, bicarbonate, serum chloride concentration [16]. In patients after OHCA, peak neuron specific enolase (NSE) within 3 days after resuscitation was assessed as a predictor of neurologic outcome in resuscitated patients [17].
Statistical analysis
Statistical analysis was performed in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement using the software R (version 4.2.2, The R foundation, Vienna, Austria) [18]. Normally distributed continuous variables were depicted as mean with standard deviation and non-normally distributed continuous variables as median with interquartile ranges. Students t-test and Mann–Whitney-U test were used to compare groups as appropriate. Categorical variables were reported as absolute numbers and percentages and Chi-squared test was utilized for comparison. All tests were 2-tailed, and p-values < 0.05 were considered significant. Mortality rates were calculated using the Kaplan–Meier method and comparisons were made by log-rank tests. Missing data for body mass index and Simplified Acute Physiology Score 2 was imputed by R package “mice” (version 3.13.0) with predictive mean matching. Univariate and multivariate cox regression analysis was performed to identify predictors for the primary endpoint of 30-day all-cause mortality. Parameters for multivariate analysis were stepwise selected by Akaike information criterion (AIC) with backward direction and 1000 bootstrap iterations using the stepAIC function of the R-package MASS (version 7.3–58.1).
R-package MatchIt (version 4.5.0; Ho, Imai, King, and Stuart) was used for propensity score matching with a 1:1 nearest neighbour algorithm, no replacement, a 0.1 caliper and the following variables:[19]. age, sex, estimated glomerular filtration rate, OHCA, duration of out-of-hospital cardiopulmonary resuscitation, myocardial infarction (STEMI, NSTEMI) as well as mechanical ventilation, VA-ECMO, percutaneous transvalvular microaxial flow pump (Impella®), catecholamine doses and serum lactate at admission. Subgroup analyses were conducted for patients after OHCA as well as for patients receiving more than the median hourly volume of resuscitation fluids during the first day. The subgroup of OHCA patients was then divided into two groups based on the median serum lactate at admission to assess OHCA patients with severe shock.
Results
Baseline characteristics
All consecutive CS patients from 2010 to 2022 were included in the analysis (Additional file 1: Fig. S1). After propensity score matching groups were well balanced with a standard difference of mean below 0.15 for all matching parameters. (Additional file 1: Fig. S2). Distribution of treatment years after matching is displayed in Additional file 1: Table S1. Characteristics of the 1032 matched patients are shown in Table 1. Patients in the saline group had less often undergone coronary artery bypass grafting and were more frequently on intraaortic ballon pump. On admission to the ICU serum lactate, arterial blood pH, bicarbonate concentration, serum creatinine, chronic dialysis and serum chloride did not differ between groups. Most patients were admitted for CS complicating myocardial infarction (23.7% NSTEMI, 29.3% STEMI, Table 1). Patients were presenting with a high percentage of OHCA (25.4% vs. 24.8%, p = 0.886) and venoarterial extracorporeal membrane oxygenation (22.5% vs. 23.1%, p = 0.882).
Fluids and electrolytes
Volumes of saline and balanced crystalloids administered as resuscitation fluid within the first seven days on the ICU are shown in Fig. 1. Cumulative fluid volume within the first week was comparable between the saline and balanced crystalloid group (mean volume in milliliters ± standard deviation: 8436.7 ± 9227.8 vs. 9086.3 ± 10,690.7, p = 0.296). Patients treated with saline had significantly higher levels of serum chloride and lower levels of bicarbonate as well as arterial blood pH (Fig. 2). Serum creatinine was comparable during the first seven days except for a significantly higher value in the saline group at day 2 (Fig. 2). Total fluid output was similar between groups on the first 7 days on ICU.
Arterial blood pH, bicarbonate, chloride, creatinine concentration and catecholamine doses. Mean values (standard deviation) of arterial blood pH (A), bicarbonate (B), chloride concentration (C) and creatinine (D) as well as median catecholamine doses (E, using the formula: dobutamine (mg/h) + 100 × epinephrine (mg/h) + 100 × norepinephrine (mg/h)) and norepinephrine (F) in patients treated with saline (Saline, black) and balanced crystalloids (Balanced, red). n.s. not significant. *p < 0.05; **p < 0.01; ***p < 0.001
Outcomes
Cumulative catecholamine doses within the first week in ICU are shown in Fig. 2. Combined catecholamine doses were numerically higher in the saline group during the first days with a significant difference on day 3 (Fig. 2E). Noradrenaline doses were significantly higher in the saline group at day two to four (Fig. 2F) despite significantly lower blood pressure in the saline group (Additional file 1: Table S3). The 30-day mortality rate was 43.1% in the saline group vs. 43.0% in the balanced crystalloid group (p = 0.833, Fig. 3). In addition, use of balanced crystalloids was not significantly associated with mortality in a cox regression analysis that included CS patients before matching (Additional file 1: Table S2). Length of stay in ICU did not differ between groups (median days (interquartile range): 5.6 (1.9–12.5) vs 5.1 (1.9–10.1) days, p = 0.358). Patients in the saline group had a higher rate of new onset renal replacement therapy (30.2% vs 22.7%, p = 0.007) as well as a higher rate of in-hospital cardiopulmonary resuscitation (18.2% vs. 13.4%, p = 0.041).
Subgroup analyses
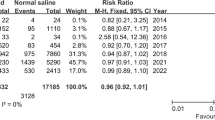
Patients after OHCA (Additional file 1: Table S4) showed a trend towards higher 30-day mortality rate when treated with balanced crystalloids group that did not reach statistical significance (53.2% vs 46.7%, p = 0.356, Fig. 4A). Patients with OHCA with lactate levels higher than 7.4 mmol/L (median of the former group) showed a higher mortality rate (79.3% vs 58.6%, p = 0.013, Fig. 4B) in the balanced group. In these patients, NSE was comparable at admission but significantly higher at 48–72 h after admission when treated with balanced crystalloids (104.6 (60.0–286.0) vs. 67.9 (34.6–148.2), p = 0.039). Furthermore, use of balanced crystalloids as resuscitation fluid as well as age, serum lactate, duration of CPR and mechanical ventilation were independently associated with a higher 30-day mortality rate in a multivariate analysis including all patients with OHCA before propensity-score matching (Table 2). Patients without OHCA showed a comparable 30-day all-cause mortality rate when treated with saline or balanced electrolytes (41.9% vs. 39.5%, p = 0.427).
30-day all-cause mortality rate of patients after out-of-hospital cardiac arrest. Kaplan–Meier curves showing 30-day all-cause mortality for patients after out-of-hospital cardiac arrest treated with saline (black) and balanced crystalloids (Balanced, red) (A) and for patients after out-of-hospital cardiac arrest with lactate at admission > 7.4 mmol/L (median) (B)
In another subgroup analysis the study cohort was divided into two subgroups each based on the median hourly volume of resuscitation fluid during the first day as well as the median serum lactate at admission. Among patients receiving more than median fluid volume (Additional file 1: Table S5), mortality rate at 30 days did not differ significantly between patients treated with saline and balanced crystalloids (51.2% vs 54.5%, p = 0.602). Among patients with higher than median serum lactate at admission, mortality rate at 30 days did not differ between groups (59.0% vs. 59.2%, p = 0.844).
Discussion
In this retrospective single center study comparing saline and balanced crystalloids as resuscitation fluid for CS patients, we did not find a significantly different mortality at 30 days, but a higher rate of new onset renal replacement therapy and higher doses of catecholamines among patients treated with saline.
Studies comparing the efficacy and safety of saline versus balanced resuscitation fluids produced conflicting results [1, 6, 8, 9, 11, 20]. While some studies found significantly higher rates of mortality and kidney failure among ICU patients treated with saline, newer randomized trials failed to reproduce the observed advantages of balanced crystalloids. Our trial is in concordance with published results showing no impact of saline versus crystalloid solution on overall 30-day mortality. However, our study is very distinct from the available evidence. While most of the preceding studies focused on unselected ICU patients with a high percentage of (elective) postoperative and sepsis patients, our study analysis the specific patient population with CS admitted to a tertiary center cardiac ICU. Compared to a heterogenous “all-comer” ICU collective, CS patients are severely ill with a very high risk of mortality and multiorgan failure including acute kidney failure. As such, baseline levels of serum lactate were much higher in our study cohort compared to patients in the PLUS trial, the only randomized trial even reporting baseline lactate [11]. CS patients typically need large amounts of resuscitation fluids to maintain sufficient circulation and when mechanical circulatory devices are implanted. Thus, cumulative volume of intravenous fluid in our study exceeded that of most preceding studies. Additionally, more than one third of patients required mechanical circulatory support, increasing the need for intravenous fluids even further, and rates of cardiac arrest were much higher in our patient population.
In previous studies, saline has been shown to cause hyperchloremic acidosis due to its high concentration of chloride [20]. Consistently, we found significantly higher levels of serum chloride and a significantly lower pH in the saline group. This hyperchloremic acidosis might explain the need for higher catecholamine doses that we found in the saline group through a direct effect on blood pressure and attenuation of catecholamines as well as the higher rate of new onset renal replacement therapy in the saline group [21, 22].
In our study, the primary endpoint of mortality rate at 30 days did not differ between groups and results remained unchanged when limiting the analysis to patients receiving large amounts of resuscitation fluids. This could be explained with the poor prognosis of CS patients. Even if balanced crystalloids might decrease acidosis and catecholamine demand in the early stages of CS, potential treatment effects are masked by the high mortality and unfavorable neurological outcome after cardiac arrest leading to palliative care.
In the BaSICS study, balanced crystalloids were associated with an increased 90-day mortality in patients after traumatic brain injury [9]. As these patients often develop intracranial hypertension, use of iso- or even hypertonic saline is often preferred over balanced electrolytes which are relatively hypotonic. In our study, 25% of patients experienced OHCA with a median duration of cardiopulmonary resuscitation of 12 min, indicating significant hypoxic brain injury. For patients after OHCA with a more severe shock state (lactate > median of OHCA cohort) we could demonstrate a significantly higher 30-day mortality rate in the balanced electrolytes group and a multivariate regression analysis revealed balanced electrolytes as an independent risk factor for mortality. Additionally, NSE was higher in the OHCA group with severe shock when treated with balanced crystalloids. These findings raise concerns that balanced fluids might be harmful in patients after non-traumatic brain injury. In accordance with results from patients with traumatic brain injury saline might be used as preferred resuscitation fluid in patients after OHCA with a more severe shock state until further evidence is provided from randomized controlled trials [9].
Limitations
This study is a retrospective single center analysis of patients from the LMUshock registry with its inherent limitations. Fluids administered before hospital admission and in the emergency department before admission to ICU as well as fluids for dilution of parenteral medications are not included in the analysis due to missing data. In our study, one specific balanced crystalloid solution was used and results might differ with other solutions, e.g. ringer’s lactate. Time of inclusion differed between the two groups by a few years and there might be differences in treatments, such as intraaortic balloon pump or indications for renal replacement therapy, not accounted for by the propensity score matching. Lastly, CS patients represent a unique patient population and findings should not be generalized. Subgroup analyses are hypothesis generating only and should be interpreted as such.
Conclusions
In this retrospective study of cardiogenic shock patients, treatment with balanced crystalloids as resuscitation fluid was associated with a similar all-cause mortality at 30 days but a lower incidence of renal replacement therapy than treatment with unbalanced crystalloids. In the subgroup of patients after out-of-hospital cardiac arrest with severe shock, use of balanced crystalloids was associated with a higher 30-day mortality rate.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to ethical committee regulations but might be available from the corresponding author on reasonable request and provided that ethical committee approves data sharing.
Abbreviations
- CS:
-
Cardiogenic shock
- ICU:
-
Intensive care unit
- NSTEMO:
-
Non-ST-elevation myocardial infarction
- OHCA:
-
Out-of-hospital cardiac arrest
- STEMI:
-
ST-elevation myocardial infarction
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- VA-ECMO:
-
Venoarterial extracorporeal membrane oxygenation
References
Hammond NE, Zampieri FG, Tanna GLD, Garside T, Adigbli D, Cavalcanti AB, et al. Balanced crystalloids versus saline in critically Ill adults—a systematic review with meta-analysis. NEJM Evid. 2022;1(2):EVIDoa2100010.
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350(22):2247–56.
Investigators SS, Australian, New Zealand Intensive Care Society Clinical Trials G, Australian Red Cross Blood S, George Institute for International H, Myburgh J, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874–84.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367(20):1901–11.
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367(2):124–34.
Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, et al. Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: The SPLIT randomized clinical trial. JAMA. 2015;314(16):1701–10.
Kellum JA. Abnormal saline and the history of intravenous fluids. Nat Rev Nephrol. 2018;14(6):358–60.
Semler MW, Self WH, Wanderer JP, Ehrenfeld JM, Wang L, Byrne DW, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med. 2018;378(9):829–39.
Zampieri FG, Machado FR, Biondi RS, Freitas FGR, Veiga VC, Figueiredo RC, et al. Effect of intravenous fluid treatment with a balanced solution vs 0.9% saline solution on mortality in critically ill patients: the BaSICS randomized clinical trial. JAMA. 2021;326(9):1–12.
Yunos NM, Kim IB, Bellomo R, Bailey M, Ho L, Story D, et al. The biochemical effects of restricting chloride-rich fluids in intensive care. Crit Care Med. 2011;39(11):2419–24.
Finfer S, Micallef S, Hammond N, Navarra L, Bellomo R, Billot L, et al. Balanced multielectrolyte solution versus saline in critically ill adults. N Engl J Med. 2022;386(9):815–26.
Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012;367(14):1287–96.
Thiele H, Akin I, Sandri M, de Waha-Thiele S, Meyer-Saraei R, Fuernau G, et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018;379(18):1699–710.
Thiele H, Ohman EM, de Waha-Thiele S, Zeymer U, Desch S. Management of cardiogenic shock complicating myocardial infarction: an update 2019. Eur Heart J. 2019;40(32):2671–83.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Pappalardo F, Schulte C, Pieri M, Schrage B, Contri R, Soeffker G, et al. Concomitant implantation of Impella((R)) on top of veno-arterial extracorporeal membrane oxygenation may improve survival of patients with cardiogenic shock. Eur J Heart Fail. 2017;19(3):404–12.
Schrage B, Rubsamen N, Becher PM, Roedl K, Soffker G, Schwarzl M, et al. Neuron-specific-enolase as a predictor of the neurologic outcome after cardiopulmonary resuscitation in patients on ECMO. Resuscitation. 2019;136:14–20.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
Ho DE, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28. https://doi.org/10.18637/jss.v042.i08.
Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308(15):1566–72.
Kellum JA, Song M, Venkataraman R. Effects of hyperchloremic acidosis on arterial pressure and circulating inflammatory molecules in experimental sepsis. Chest. 2004;125(1):243–8.
Pfortmueller CA, Funk GC, Reiterer C, Schrott A, Zotti O, Kabon B, et al. Normal saline versus a balanced crystalloid for goal-directed perioperative fluid therapy in major abdominal surgery: a double-blind randomised controlled study. Br J Anaesth. 2018;120(2):274–83.
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
JG: drafting of manuscript, statistical analysis, final approval. BB: Substantial contribution to data acquisition. EL: Substantial contribution to data acquisition. LB: Substantial contribution to data acquisition. DK: Substantial contribution to data acquisition, revision of manuscript. TS: Substantial contribution to data acquisition. KL: Substantial contribution to data acquisition, revision of manuscript. LW: Substantial contribution to data acquisition. SR: data acquisition, revision of manuscript. TP: data interpretation, revision of manuscript. SK: data interpretation, revision of manuscript. JH: data interpretation, revision of manuscript. CH: data interpretation, revision of manuscript. SM: data interpretation, revision of manuscript. MO: data interpretation, revision nof manuscript. CS: data acquisition, statistical analysis, drafting of manuscript, final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethics committee of the Ludwig-Maximilians University Munich (IRB number: 18–001).
Consent for publication
Not applicable.
Competing interests
Martin Orban: Speaker honoraria from Abbott Medical, AstraZeneca, Abiomed, Bayer vital, BIOTRONIK, Bristol-Myers Squibb, CytoSorbents, Daiichi Sankyo Deutschland, Edwards Lifesciences Services, Sedana Medical, support for attending meetings from AstraZeneca, Stocks from Abbott Laboratories, Abbvie, AstraZeneca, Bayer, Biontech, Bristol-Meyer- Squibb, Curevac, Draegerwerk, Fresenius Medical Care, Gilead sciences, Inari Medical, Johnson&Johnson, Linde, Merck US, Moderna, NovoNordisk, Nuance Communications, Pfizer, Proctor&Gamble, Roche, SAP, Siemens healthiniers, Zoom. Jörg Hausleiter: Speaker honoraria from and serves as consultant for Abbott Vascular and Edwards Lifesciences. Clemens Scherer: Speaker honoraria from AstraZeneca. Ludwig Weckbach: Speaker honoraria from AstraZeneca and Bayer. Remaining authors: no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Study flowchart. Figure S2. Standardized mean differences before and after propensity score matching. Love plot depicting standardized mean differences before (unadjusted) and after propensity score matching (adjusted). Table S1. Year of inclusion. Table S2. Cox regression analysis. Table S3. Blood pressure. Table S4. Subgroup characteristics for patients after out-of-hospital cardiac arrest. Table S5. Subgroup characteristics for patients that received high amounts of resuscitation fluid.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gmeiner, J., Bulach, B., Lüsebrink, E. et al. Comparison of balanced and unbalanced crystalloids as resuscitation fluid in patients treated for cardiogenic shock. j intensive care 11, 38 (2023). https://doi.org/10.1186/s40560-023-00687-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-023-00687-y