Abstract
Acute respiratory distress syndrome (ARDS) is a fatal condition with insufficiently clarified etiology. Supportive care for severe hypoxemia remains the mainstay of essential interventions for ARDS. In recent years, adequate ventilation to prevent ventilator-induced lung injury (VILI) and patient self-inflicted lung injury (P-SILI) as well as lung-protective mechanical ventilation has an increasing attention in ARDS.
Ventilation-perfusion mismatch may augment severe hypoxemia and inspiratory drive and consequently induce P-SILI. Respiratory drive and effort must also be carefully monitored to prevent P-SILI. Airway occlusion pressure (P0.1) and airway pressure deflection during an end-expiratory airway occlusion (Pocc) could be easy indicators to evaluate the respiratory drive and effort. Patient-ventilator dyssynchrony is a time mismatching between patient’s effort and ventilator drive. Although it is frequently unrecognized, dyssynchrony can be associated with poor clinical outcomes. Dyssynchrony includes trigger asynchrony, cycling asynchrony, and flow delivery mismatch. Ventilator-induced diaphragm dysfunction (VIDD) is a form of iatrogenic injury from inadequate use of mechanical ventilation. Excessive spontaneous breathing can lead to P-SILI, while excessive rest can lead to VIDD. Optimal balance between these two manifestations is probably associated with the etiology and severity of the underlying pulmonary disease.
High-flow nasal cannula (HFNC) and non-invasive positive pressure ventilation (NPPV) are non-invasive techniques for supporting hypoxemia. While they are beneficial as respiratory supports in mild ARDS, there can be a risk of delaying needed intubation. Mechanical ventilation and ECMO are applied for more severe ARDS. However, as with HFNC/NPPV, inappropriate assessment of breathing workload potentially has a risk of delaying the timing of shifting from ventilator to ECMO. Various methods of oxygen administration in ARDS are important. However, it is also important to evaluate whether they adequately reduce the breathing workload and help to improve ARDS.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is a fatal condition with insufficiently clarified etiology. The Berlin Definition is the currently available clinical criteria for ARDS [1], which consists of acute onset, hypoxia with the partial pressure of arterial oxygen (PaO2)/fraction of inspiratory oxygen (FIO2) ratio of less than 300 mmHg, diffuse infiltrates on chest radiograph or computed tomography (CT), and respiratory failure not fully explained by the cardiac failure or fluid overload. The survival rate is improving from the first report of 50% [2] to around 70% [3, 4]. However, the precise survival rate remains uncertain, because the pathogenesis of ARDS is very heterogeneous and the survival rate may vary according to the pathogenesis of ARDS.
Supportive care for severe hypoxemia remains the mainstay of an effective intervention for ARDS. An adequate oxygen administration to prevent hypoxemia, as well as ventilator-induced lung injury (VILI) and patient self-inflicted lung injury (P-SILI), could potentially facilitate recovery of alveolar epithelial damage in ARDS.
In this review, I focused on the recent advances in the field of oxygen administration for patients with ARDS.
Unclarified issues
The Berlin definition is the most widely used severity classification for ARDS [5]. According to this definition, potential therapeutic options according to the severity of ARDS have been proposed [6]. In this proposal, it is stated that ARDS requires low tidal volume ventilation of 6 mL/kg predicted body weight and plateau pressure below 30 cm H2O regardless of severity. For mild to moderate ARDS, low to moderate positive end-expiratory pressure (PEEP) is suggested, and for more severe ARDS, higher PEEP is needed. Non-invasive ventilation is suggested for mild ARDS with a PaO2/FIO2 ratio of 200 or higher. In more severe ARDS with a PaO2/FIO2 ratio of less than 150, inhibition of excessive spontaneous breathing with muscle relaxants and supine positioning to improve ventilation-perfusion mismatch are recommended. These recommendations are very reasonable and acceptable. However, these recommendations are based only on the severity of ARDS (i.e., PaO2/FIO2 ratio) and do not take into account other factors, for example, P-SILI due to excessive spontaneous breathing, reduction of respiratory workload, patient-ventilator dyssynchrony that may potentially cause alveolar epithelial injury, and, conversely, ventilator-induced diaphragm dysfunction (VIDD) complicated by ventilator over/under-assistance, dyssynchrony, or excessive PEEP. For achieving adequate respiratory support in ARDS, factors other than the PaO2/FIO2 ratio may need to be considered.
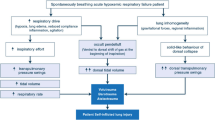
Figure 1 summarizes the suggested flowchart of respiratory management in patients with ARDS. Various physiological variables including respiratory drive and effort, dyssynchrony, and VIDD should be considered for the adequate management of hypoxemia in ARDS.
Management flow of oxygen administration for patients with ARDS. According to the severity of ARDS, HFNC, NPPV, MV, and ECMO should be used as appropriate. The most important thing is to continuously monitor not only oxygenation, but also respiratory drive/ effort and other parameters. If any of these indicators are inadequate, the procedure of oxygen administration should be immediately changed for improving respiratory drive/ effort. ARDS, acute respiratory distress syndrome; HFNC, high-flow nasal cannula; NPPV, non-invasive positive pressure ventilation; MV, mechanical ventilation; ECMO, extracorporeal membrane oxygenation
Respiratory drive and effort
Excessive respiratory drive and effort may increase the severity of lung injury, which may prolong the duration of mechanical ventilation and affect patient outcomes. Therefore, adequate regulation of spontaneous breathing has been increasingly recognized as important in respiratory management in ARDS. It would be important to systematically measure the respiratory drive in ventilated patients making spontaneous breathing and to assess how high respiratory drive leads to subsequent deterioration of respiratory function during attempts to weaning from mechanical ventilation [7].
Airway occlusion pressure (P0.1) is a simple, non-invasive measure for estimating respiratory drive during mechanical ventilation, which can be used automatically in almost all mechanical ventilators [8, 9]. P0.1 is defined as the negative airway pressure occurring during the first 0.1 s of an occluded inspiration (Fig. 2). The absence of airflow rate makes P0.1 independent from respiratory compliance, resistance, and muscle weakness. Small P0.1 indicates the weak patient’s inspiratory effort, while large P0.1 indicates the strong patient’s inspiratory effort. Too weak inspiratory effort can be associated with weaning failure, while too strong inspiratory effort can be associated with P-SILI. Telias et al. [10] investigated the correlation of P0.1 with respiratory drive and effort by using various mechanical ventilators. P0.1 was well correlated with alternative measures of respiratory drive, including the electrical activity of the diaphragm, and with inspiratory effort measured by the esophageal pressure-time product. In addition, P0.1 could have detected excessive inspiratory effort with the cut-off value of 3.5 to 4.0 cm H2O (sensitivity, 0.67; specificity, 0.86–0.91; accuracy 0.82–0.86) and low inspiratory effort with the cut-off value of 1.0 cm H2O (sensitivity, 0.75; specificity, 0.95; accuracy 0.89), respectively. It is important to note that Servo ventilators estimate P0.1 by the airway pressure drop during the trigger phase without true occlusions, whereas others (Evita-XL and Puritan Bennett) measure P0.1 with true occlusions, suggesting that P0.1 can be underestimated in the use of Servo ventilators. In that case, the cut-off value for P0.1 should be lower (i.e., 2.0 cm H2O).
Procedure to measure P0.1. Ventilator screen displaying P0.1 calculated from the change in airway pressure associated with 0.1 s of airway occlusion. Gray arrow indicates the buttons used for P0.1 measurement. Gray square indicates the intervals of 0.1 s of airway occlusion. White arrow indicates the negative airway pressure occurring during 0.1 s of airway occlusion (P0.1), with the most recent data being − 1.5 cm H2O
Dyssynchrony
Patient-ventilator dyssynchrony is a time mismatching between patient’s effort and ventilator drive, often occurs during assisted ventilator modes. Although dyssynchrony can occur in around 25% of mechanically ventilated patients [11], it is frequently unrecognized and is associated with poor clinical outcomes. Esophageal pressure (transpulmonary pressure) can be used for better detection of dyssynchrony. Dyssynchrony can lead to increased work of breathing, auto-positive end-expiratory pressure (PEEP), poor gas exchange, prolonged use of mechanical ventilation, and barotrauma [11, 12]. The major groups of dyssynchrony include (A) trigger asynchrony, (B) cycling asynchrony, and (C) flow delivery mismatch [13]. Adjusting the ventilator settings can dramatically improve patient-ventilator dyssynchrony [14] (Fig. 3).
Variation of dyssynchrony. Combination of airway pressure and tidal volume curves showing various types of dyssynchrony. a Ineffective triggering (miss triggering): Small waveform changes during expiration indicate the presence of weak spontaneous breathings that was not triggered (white arrows). It can be associated with a weak patient respiratory drive. Ineffective triggering can occur in situations combined with underlying auto-PEEP and excessive ventilation. It can be adjusted by extended expiratory time and increased trigger sensitivity. b Double triggering: Prolonged spontaneous breathing is generating a second mechanical ventilation immediately after the completion of the first mechanical ventilation (white arrow). It can occur when second breathing starts before the first ventilation delivery has completed. Double triggering may be adjusted by extended inspiratory time. c Auto triggering: Excessive mechanical ventilation (black arrows) is occurring despite the lack of patient’s respiratory effort (white arrows), which might be associated with the water in the circuit or circuit leakage. This type of asynchrony can occur in cases of sputum in the circuit, condensation, circuit leakage, or heart oscillations. Auto triggering can be adjusted by lowering the triggering sensitivity of the mechanical ventilator or by removing sputum or condensation. d Reverse triggering: Spontaneous breathing is paradoxically triggered by mechanical ventilation, resulting in a generation of double triggering (white and black arrows). Reverse triggering is frequently observed in highly sedated patients. Reverse triggering can be adjusted by decreasing sedation. e Premature cycling: Since mechanical ventilation is completed earlier than the completion of spontaneous breathing, there remains spontaneous breathing in the expiratory phase. Waveform swinging is observed in the exhalation phase (white and black arrows). Premature cycling can be adjusted by extending inspiratory time. f Delayed cycling: Since spontaneous breathing is completed earlier than the completion of mechanical ventilation, the inspiratory phase is rapidly terminated (white and black arrows). Delayed cycling can be adjusted by reducing inspiratory time. Gray bars indicate the time periods of spontaneous breathing. P, airway pressure curve; V, tidal volume curve
Figure 4 shows a patient presenting with various dyssynchronies. The patient exhibited a great variety of dyssynchronies, including ineffective triggering, reverse triggering, double triggering, and auto triggering in a very short period of time. The target tidal volume was set as 320 mL (6 mL/kg), and the actual tidal volume was 271 mL (5.6 mL/kg). The observed dyssynchronies increased the tidal volume up to 432 mL (9.0 mL/kg), which was unacceptable for lung-protective ventilation.
Practical examples of various dyssynchrony. Ventilator screen displaying various dyssynchrony. a Reverse triggering: The airway pressure curve demonstrated the waveform during the expiratory phase swinging slightly toward negative pressure (white arrows). The waveforms of airway flow and tidal volume were also deformed (gray arrows), indicating a presence of reverse triggering. b Ineffective triggering (white arrow) and auto triggering (gray arrow): The baseline before the first inspiration fluctuated slightly (white arrows), indicating a presence of ineffective triggering. The second inspiration had a different waveform from the others (gray arrows) with the absence of the patient’s respiratory effort, indicating auto triggering. c The airway pressure/airway flow curve presented a jaggy baseline (white arrows), indicating a presence of droplets or secretion in the circuit. The ventilation volume curve did not return to the baseline (gray arrow), indicating a presence of auto-PEEP. d The first inspiration induced reverse triggering and deformed expiratory waveform (white arrow). Consequently, a reverse triggering induced a double triggering (gray arrow). e The airway pressure/airway flow curve demonstrated the first expiratory waveform was trembling (white arrow), indicating the presence of an ineffective triggering
Among these dyssynchronies, reverse triggering is the newly emerging type of dyssynchrony with a potential risk of alveolar injury. After the widespread use of low tidal volume ventilation in ARDS, double triggering in heavily sedated patients can be frequently observed in association with breath stacking [15]. Greater neural inspiratory time compared with ventilatory inflation time could be responsible for this phenomenon. Recent studies suggested that one-third of the breath stacking was associated with reverse triggering [16]. Reverse triggering is likely to be injurious if the ventilator delivers a second breath. Greater effort resulting from reverse triggering can be injurious as it can induce eccentric contractions when it occurs during the expiratory phase and can induce pendelluft and excessive local lung stress when it occurs during the inspiratory phase [17,18,19].
On the contrary, Rodriguez et al. [20] reported inconsistent findings in a prospective, multicenter, observational study. They investigated the frequency of reverse triggering and its impact on clinical outcomes during the early phase of non-paralyzed mechanically ventilated patients with ARDS. They collected a total of 100 patients and evaluated the ventilatory patterns obtained after a median of 24 h of intubation. Fifty percent of patients demonstrated reverse triggering without breath stacking. Increased occurrence of reverse triggering was associated with lower tidal volume (odds ratio [OR], 0.91 per 0.1 mL/kg; 95% confidence interval (CI), 0.84–0.98; p = 0.02) and less use of fentanyl (OR, 0.93 per 10 micrograms; 95%CI, 0.88–0.99; p = 0.02). We should note that the presence of reverse triggering was not associated with the duration of mechanical ventilation, but was associated with a reduced 90-day in-hospital mortality rate (hazard ratio [HR], 0.65; 95%CI, 0.57–0.73; p < 0.001). The authors concluded that the early detection of reverse triggering may be a good indicator of a favorable outcome in patients with mild to moderate ARDS. Further investigations are necessary for determining whether specific intervention should be applied for reverse triggering to improve patient outcomes.
Ventilator-induced diaphragm dysfunction (VIDD)
Ventilator-induced diaphragm dysfunction (VIDD) is a form of iatrogenic injury from inadequate use of mechanical ventilation [21, 22]. VIDD is not solely due to modes of mechanical ventilation but rather can be caused by inappropriate ventilator support through various mechanisms. While VIDD can be largely induced by disuse atrophy due to ventilator over-assistance, several other mechanisms including load-induced injury due to ventilator under-assistance, eccentric contractile injury due to dyssynchrony, and excessive shortening due to high PEEP can also be involved.
Diaphragm muscle weakness can rapidly occur in mechanically ventilated critically ill patients in the ICU [23,24,25,26], which can be associated with an increased mortality rate [27,28,29]. VIDD can occur twice as frequently as limb muscle weakness, which has a negative impact on successful weaning [30]. Disuse of diaphragm muscle can be a potential risk factor of VIDD. However, the best balance between the increased respiratory drive/ effort and the risk of VIDD can be difficult to be adequately defined. Diaphragm ultrasound can directly visualize diaphragm, which has been proposed to assess VIDD and a resultant inspiratory effort [26, 31,32,33]. Low excursion of the diaphragm or weak apposition thickening detected by diaphragm ultrasound was a strong predictor of weaning failure [30, 33,34,35,36].
The impact of spontaneous mechanical ventilation on VIDD has not been well known. Animal studies have demonstrated that spontaneous mechanical ventilation may be more protective than controlled mechanical ventilation [37, 38], whereas these data have not been well confirmed in human subjects. Marin-Corral et al. [39] investigated the effects of different modes of mechanical ventilation in respiratory and peripheral muscles in ventilated organ donors. They demonstrated that the cross-sectional area of the diaphragm was significantly reduced in patients who did not receive diaphragm stimuli compared with those who received diaphragm stimuli. These findings supported the hypothesis that spontaneous mechanical ventilation would be more favorable for preventing VIDD compared with controlled mechanical ventilation.
Lindqvist et al. [40] investigated the effect of PEEP on VIDD. Typically, mechanically ventilated patients with ARDS would be managed by using PEEP to avoid alveolar collapse. However, the use of PEEP can increase end-expiratory lung volume, resulting in the flattened diaphragm dome and structural modification in the diaphragm fibers. They demonstrated that PEEP induced a caudal movement of the diaphragm both in critically ill patients and in animal models, which resulted in the shortening of muscle fiber length. The shortened muscle fibers can generate less force, resulting in diaphragm dysfunction. Slow reduction in PEEP would be favorable to allow the reversal of longitudinal muscle atrophy.
Goligher et al. [41] investigated the clinical impact of VIDD on the duration of mechanical ventilation. They included a total of 191 patients requiring mechanical ventilation, and diaphragm thickness was measured daily by ultrasound. More than a 10% decrease in diaphragm thickness was observed in 41% of patients by median day 4. Development of decreased diaphragm thickness was associated with a lower probability of ventilator withdrawal (HR, 0.69 per 10% reduction; 95% CI, 0.54–0.87), prolonged ICU stays (adjusted duration ratio, 1.71; 95%CI, 1.29–2.27), and increased complications (OR, 3.00; 95%CI, 1.34–6.72). On the other hand, however, the development of increased diaphragm thickness was also associated with prolonged ventilation (adjusted duration ratio, 1.38; 95%CI, 1.00–1.90). Patients with a diaphragm thickening rate of 15 to 30% (similar to resting breathing) during the first 3 days presented the shortest duration of ventilation. This study suggested that targeting an inspiratory effort level similar to that of healthy subjects at rest might be most effective for reducing the duration of mechanical ventilation.
HFNC and NPPV
High-flow nasal cannula (HFNC) and non-invasive positive pressure ventilation (NPPV) are the non-invasive techniques for supporting hypoxemia and respiratory effort in patients with severe hypoxemic respiratory failure. The major advantages of HFNC could be the better tolerability compared with NPPV, provides high FIO2, and can unload the inspiratory muscles by washing out the dead space in the upper airway with low levels of positive pressure. On the other hand, the major advantages of NPPV could be the provision of higher FIO2, and more reliable unloading of the inspiratory muscles by providing higher positive airway pressure. HFNC and NPPV can be effective non-invasive ventilatory devices for ARDS, since the reduction of respiratory workload is an important factor as well as the improvement of hypoxemia [42, 43].
As a result of the increasing use of HFNC, there is a risk of delays in needed intubation. This is an important concern, as a number of previous studies demonstrated that patients who failed to manage NPPV with acute respiratory failure have worse outcomes. This has been shown in NPPV [29] and also in HFNC [44]. In addition, there are no prospectively validated criteria for intubation in patients with ARDS. This may result in considerable variation among clinicians and may affect patient outcomes.
Roca et al. [45] investigated the diagnostic accuracy of the ROX index defined as the ratio of oxygen saturation (SpO2)/FIO2 to respiratory rate for predicting the need for intubation in patients with hypoxemic respiratory failure. They included a total of 191 patients, of whom 68 (36%) patients required intubation. The area under the ROC curve of ROX index at 2, 6, and 12 h after initiating HFNC for predicting intubation were 0.648 (95%CI, 0.561–0.734; p = 0.001), 0.672 (95%CI, 0.580–0.764; p < 0.001), and 0.695 (95%CI, 0.598–0.791; p < 0.001), respectively. A ROX index of < 2.85 at 2 h, < 3.47 at 6 h, and < 3.85 at 12 h of initiating HFNC, respectively, were predictors of HFNC failure. In addition, the serial changes of its value may help discriminate patients with HFNC success from those with HFNC failure.
Another important topic regarding HFNC is the identification of subgroups of acute respiratory failure for which HFNC is effective. Azoulay et al. [46] investigated whether HFNC decreases mortality among immunocompromised patients with ARDS compared with standard oxygen therapy. They included a total of 776 patients with a median partial pressure of arterial oxygen (PaO2)/FIO2 ratio of 136 (interquartile range [IQR], 96–187), and 128 (IQR, 92–164) in the intervention and control groups, respectively. The authors found no significant difference between the cohorts regarding 28-day mortality (36% vs 36%), intubation rate (39% vs 44%), ICU length of stay (8 vs 6 days), ICU-acquired infections (10% vs 11%), or hospital length of stay (24 vs 27 days). These results suggested that intensive attention for improving oxygenation may not beneficial for improving survival in immunocompromised patients with ARDS.
The HACOR (heart rate, acidosis, consciousness, oxygenation, and respiratory rate) score was an index for predicting NPPV failure in patients with ARDS. Duan et al. [47] included a total of 449 patients requiring NPPV and evaluated the predictive value of the HARCOR score. The failure rate of NPPV was 48% and 39% in the test and validation cohorts, respectively. The areas under the ROC curve of the HACOR score assessed at 1 h of NPPV for predicting HPPV failure were 0.88 (95%CI, 0.84–0.91) for the test cohort and 0.91 (95%CI, 0.88–0.94) for the validation cohort. With the cut-off value of > 5, sensitivity, specificity, and diagnostic accuracy were 73–76%, 90–93%, and 82–86%, respectively. In addition, the serial changes of its value could also discriminate patients with NPPV success from those with NPPV failure.
Innocenti et al. [48] further investigated the utility of the HACOR score in a patient with acute respiratory failure requiring NPPV. They retrospectively included a total of 644 hypoxemic patients with or without hypercapnia, of whom 147 (23%) patients have died during the observation period. The area under the ROC curve of the HACOR score for predicting in-hospital mortality were 0.64 (95%CI, 0.58–0.69; p < 0.001) at initiating NPPV, 0.68 (95%CI, 0.63–0.73; p < 0.001) at 1 h of NPPV, and 0.75 (95%CI, 0.70–0.80; p < 0.001) at 24 h of NPPV, respectively. The Cox survival analysis for in-hospital mortality demonstrated that the HACOR score of > 5 at 24 h of NPPV was associated with increased in-hospital mortality (RR, 2.39; 95%CI 1.60–3.56; p < 0.001).
Since HFNC or NPPV can be used outside the ICU and could be a good alternative for patients who are not candidates for invasive mechanical ventilation, these scoring tools would be useful for the adequate use of HFNC/ NPPV.
Mechanical ventilation
Because mechanical ventilation includes a potential risk of VILI, low tidal volume ventilation, synonymous with lung-protective ventilation, remains the most recommended ventilatory management in patients with ARDS. Previous studies and meta-analyses demonstrated the beneficial effect of low tidal volume ventilation in patients with ARDS. This ventilatory strategy typically consists of tidal volume of 4–8 mL/kg predicted body weight, plateau pressure (Pplat) of < 30 cm H2O, and sufficient PEEP, which can be roughly estimated as multiplying FIO2 by 20 (i.e., if FIO2 is 0.5, PEEP would be around 10 cm H2O; if FIO2 is 1.0, PEEP would be around 20 cm H2O), according to the PEEP/FIO2 table [49]. A randomized clinical trial (RCT) including 961 patients with ARDS, the PReVENT trial [50], investigated the benefit of low tidal volume ventilation (< 6 mL/kg of predicted body weight (PBW), with titration to a target of 4 mL/kg PBW) compared with intermediate tidal volume ventilation (10 mL/kg PBW). They demonstrated no significant benefit of low tidal volume ventilation in ventilator-free days, hospital length of stay, 28-day and 90-day mortalities, or the risk of adverse events. However, around 25% of the low tidal volume ventilation cohort received a tidal volume of > 6 mL/kg PBW by day 3. Similarly, around 25% of the intermediate tidal volume ventilation cohort received a tidal volume of > 10 mL/kg PBW by day 3. Therefore, insufficient differences observed in this study could have been associated with these actual tidal volumes.
The LIVE study [51] was a multicenter, single-blind, stratified, parallel-group, RCT enrolling patients with moderate to severe ARDS in France. They investigated whether a mechanical ventilation strategy that was personalized to individual patients’ lung morphology would improve survival when compared with standard care. In the personalized cohort, patients with focal ARDS received a tidal volume of 8 mL/kg, low PEEP, and prone position. Patients with non-focal ARDS received a tidal volume of 6 mL/kg, along with recruitment maneuvers and high PEEP. In a multivariate analysis, there was no difference in 90-day mortality between the cohorts (HR, 1.01; 95%CI, 0.61–1.66; p = 0.98). However, a significant number of misclassifications of focal or non-focal ARDS was found in 21% of enrolled patients. In addition, misclassification of patients was associated with the increased 90-day mortality compared with the control cohort (HR, 2.8; 95%CI, 1.5–5.1; p = 0·012). This study suggested the potential difficulty and risk of personalized ventilatory management.
The difference between volume-limited assist-control mode and pressure-limited assist-control mode seems minimal. Previous studies demonstrated no significant differences in mortality, oxygenation, or respiratory effort [52,53,54]. Synchronized intermittent mandatory ventilation (SIMV) is one of the most frequently used ventilatory modes to facilitate patient-ventilator synchrony, to preserve respiratory muscle, and to minimize the risk of auto-PEEP. However, in terms of respiratory effort and constant tidal volume, the assist-control mode would be more reasonable for patients with ARDS compared with SIMV. Pressure support ventilation (PSV) could be an adequate option for weaning from mechanical ventilation, because respiratory effort can be proportionally supported by PSV. However, no studies supported the beneficial effect of PSV for weaning to date. In addition, the following characteristics of PSV could be disadvantages for patients with the acute phase of ARDS:
-
1.
Respiratory effort of patients with ARDS cannot be fully supported.
-
2.
Defined tidal volume and respiratory rate cannot be provided.
-
3.
Patient-ventilator asynchrony can occur.
-
4.
Higher levels of pressure support could be necessary to prevent alveolar collapse.
Regardless of whether the volume-limited or pressure-limited assist-control mode is selected, fully supported modes are generally favorable compared with partially supported modes in patients with ARDS.
Oxygen concentration and oxygen toxicity
Most patients with ARDS require a high concentration of oxygen to maintain sufficient oxygenation. However, we should be aware of the potential toxicity of a high concentration of oxygen. Previous studies using human cohort and animals demonstrated that the high concentration of inspired oxygen was associated with the occurrence of acute lung injury, ranging from mild to severe diffuse alveolar damage (DAD) [55]. In general, oxygen toxicity may be increased in patients receiving FIO2 of more than 0.6. A longer duration of exposure can induce severer lung injury.
Chu et al. [56] conducted a meta-analysis to investigate the impacts of liberal and conservative oxygen therapy on mortality and morbidity in acutely ill adult patients. They included a total of 25 RCTs with 16,037 patients and demonstrated that the liberal oxygen strategy (median FIO2, 0.52, IQR 0.28–1.0) increased in-hospital mortality and 30-day mortality compared with the conservative oxygen strategy (median FIO2, 0.21; IQR, 0.21–0.25). In addition, a meta-regression effect of SpO2 on in-hospital mortality showed an increased SpO2 was associated with an increased risk of mortality. Barbateskovic et al. [57] subsequently conducted another meta-analysis to evaluate the benefits and harms of higher versus lower FIO2 or target PaO2 in adult patients in ICU. They included a total of 10 RCTs with 1458 patients, and demonstrated that lower FIO2 or target PaO2 was associated with a marginal increase in the risk of mortality. In addition, higher FIO2 or target PaO2 was also associated with an increase in serious adverse events. However, the certainty in many of the included studies was very low, indicating that these results should be carefully interpreted.
By contrast, a subsequent RCT, the ICU-ROX study [58], investigated the benefit of conservative use of oxygen in adult patients who underwent mechanical ventilation. They enrolled a total of 1000 patients and demonstrated no significant benefit of conservative oxygen strategy (SpO2 90–97%) compared with liberal oxygen strategy (SpO2 > 90%) for ventilator-free days or 180-day mortality. Another RCT, the LOCO2 study [59], investigated whether targeting lower PaO2 would improve outcome in patients with ARDS. They enrolled a total of 205 patients with ARDS, and demonstrated no benefit of conservative oxygen strategy (target PaO2, 55–70 mmHg; target SpO2, 88–90%) compared with liberal oxygen strategy (target PaO2, 90–105 mmHg; target SpO2, > 96%) on 28-day mortality. However, this study was prematurely stopped for safety concerns and a low likelihood of a significant difference.
Accordingly, the optimal strategy for supplemental oxygen is still controversial. In addition, these studies were predominantly conducted in the critically ill patient cohort. Therefore, the optimal strategy of supplemental oxygen for patients with ARDS remains unknown.
ECMO
Although mechanical ventilation is the most common procedure to maintain oxygenation in patients with ARDS, the use of mechanical ventilation can potentially be associated with the occurrence of VILI, VIDD, or ventilator-associated pneumonia (VAP). ECMO, typically the venovenous (V-V) ECMO, would be the useful candidate for providing better oxygenation as well as minimizing the risk of VILI or VIDD. However, ECMO can also be associated with the potential risks including bleeding, thrombosis, and infection, an adequate selection of patients who can be favored from ECMO would be important.
Patient selection
The generally accepted criteria for patient selection would be the guidelines published by the Extracorporeal Life Support Organization (ELSO) [60, 61]. ECMO should be considered for patients with the risk of mortality of > 50%, and is indicated for patients with the risk of mortality of > 80%. The risk of mortality of > 50% can be estimated by a PaO2/FIO2 ratio of < 150 on FIO2 > 0.9, and/or Murray score of 2–3. The risk of mortality of > 80% can be estimated by a PaO2/FIO2 ratio of < 100 on FIO2 > 0.9, and/or Murray score of 3–4. Intolerable hypercapnia and severe air leak syndromes would also be good indication for V-V ECMO. Contraindications include mechanical ventilation at high settings (i.e., FIO2 > 0.9, plateau pressure of > 30 cm H2O) for > 7 days, older age (with no specific cut-off value), and severe complications (i.e., irreversible organ damage).
Indications of V-V ECMO for patients with COVID-19 are generally consistent with the guidelines published by ELSO [62]. However, specific considerations for patient selection would be different, according to the presence or absence of pandemic situation. In a limited capacity, the resource-intensive support will be more preferential than the common recommendations [62]. Increased age seemed associated with increased mortality. Therefore, age of > 65, obesity (body mass index of > 40), duration of mechanical ventilation of > 10 days, Clinical Frailty Scale category of ≥3, and severe complications (i.e., chronic heart, liver, renal, neurological dysfunctions) would be relative or absolute contraindications.
Initiation of ECMO
There are various forms of ECMO configuration (Fig. 5). One of the most important things to consider when starting ECMO is the cannula diameter. The use of a sufficiently large cannula minimizes blood cell destruction and limits the volume of blood transfusions. As the FACTT trial [63] has shown, the conservative fluid management strategy can improve lung function and shorten the duration of mechanical ventilation and ICU stay. The risk of inserting an additional drainage cannula at a later stage to further improve oxygenation should be minimized. Drainage cannulae are recommended to use a minimum of 23 Fr for adults. Return cannulae are recommended 19–23 Fr for adults.
Various forms of V-V ECMO configurations and their characteristics. Various forms of V-V ECMO configurations can be used, according to their merits and demerits. a Femo-jugular approach: It is probably the most widely used configuration and has the advantage of being generalized and easy to use. However, since the neck and inguinal area are fixed, the physical liberality is low. In addition, recirculation is obvious. b Femo-femoral approach: Both two cannulas are placed in the vena cava inferior or the right atrium, approached from the left and right inguinal areas. Adequate diameter of vena cava inferior is essential. Side holes of return cannula must be centralized at the tip. c Double lumen cannula: It is usually approached through the right jugular vein, passing through the right atrium and locating the tip in the vena cava inferior. It has the advantage of complete freedom of both lower limbs. However, it is also associated with the disadvantages including the risk of malpuncture of the heart, inadequate positioning of the side hole of the return cannula not facing to the tricuspid valve, and the limited ECMO blood flow. RA, right atrium; RV, right ventricle; Ao, aorta; DC, drainage cannula; RC, return cannula
The side holes of the cannula should be concentrated at the tip as much as possible. This is because the blood flow in the drainage cannula is larger at the proximal holes. This means that even if the tip of the drainage cannula is sufficiently located in the right atrium, the blood will be primarily drained from the superior or inferior vena cava through a drainage cannula with the side holes being widely distributed. Predominant drainage of blood from the superior or inferior vena cava can lead to inadequate blood flow.
In general, it is preferable to make no skin incision during cannulation. This is because even the smallest skin incision is at risk of inducing persistent bleeding and disrupting the systemic coagulation system due to the effects of heparin during ECMO management.
The material at the tip of the drainage cannula should contain metal wire, because V-V ECMO often requires high blood flow. The use of a drainage cannula made of soft material, which is often used in V-A ECMO, can cause the cannula to be collapsed and obstructed.
Balance between oxygen supply and consumption
Various formulas are necessary to assess the balance between oxygen supply and consumption in organs during ECMO management. The oxygen content (CaO2), oxygen supply (DO2), and oxygen consumption (VO2) can be calculated by the following equations:
-
CaO2 (mL/dL) = (1.34 × Hb × SaO2/100) + (0.003 × PaO2)
-
DO2 (mL/min) = CaO2 (mL/dL) × cardiac output (L/min) × 10 (unit correction)
-
VO2 (mL/min) = body surface area (m2) × 120
= 3 mL/kg/min (adults), 4–5 mL/kg/min (pediatrics), 6 mL/kg/min (neonates)
Normally, anaerobic metabolism does not occur and sufficient tissue oxygenation can be obtained if DO2 is more than three times that of VO2. These equations indicate that it is important to maintain not only SaO2, but also sufficient hemoglobin and cardiac output to supply sufficient oxygen to the peripheral tissues. The ECMO blood flow should be set so that the ECMO can supply all the required oxygen demand. Since oxygen demand can be calculated from the difference in oxygen supply between before and after the artificial lung, the required ECMO blood flow can be calculated using the following equation. If SpostO2 is 100% and SpreO2 is 70%, the required ECMO flow rate can be calculated to be about 4.1 L/min.
-
VO2 (mL/min) = DpostO2 − DpreO2
= (1.34 × 12 × (SpostO2 − SpreO2)) × ECMO blood flow × 10
-
DpostO2: Oxygen supply after the artificial lung
-
DpreO2: Oxygen supply before the artificial lung
-
SpostO2: Oxygen saturation after the artificial lung
-
SpreO2: Oxygen saturation before the artificial lung
-
ECMO blood flow (approximation)
= 60–80 mL/kg/min (adults), 80–100 mL/kg/min (pediatrics), 120 mL/kg/min (neonates)
Adjustment
FIO2 of V-V ECMO is always used at 1.0. A decrease in patient PaO2 is adjusted by increasing ECMO flow, and the target SpO2 is usually set to 85% or higher. The ratio of ECMO blood flow to sweep gas is approximately 1:1, and an increase in patient partial pressure of carbon dioxide (PaCO2) is adjusted by increasing the sweep gas flow. However, because rapid PaCO2 correction can induce cerebral vasoconstriction and cerebral hemorrhage, PaCO2 should be slowly adjusted.
The ventilator is usually set to the lung-protective ventilation setting (i.e., controlled ventilation mode, FIO2 of 0.21–0.40, plateau pressure of 20 cm H2O, PEEP of 10 cm H2O, respiratory rate of 5–10 breaths/min, respectively). The improvement of atelectasis by applying high PEEP is not important.
If SpO2 is decreased, it should be precisely evaluated whether it is caused by patient or ECMO factors. Patient factors include pneumothorax, increased oxygen consumption (e.g., sepsis), hemorrhage, decreased cardiac function, and pulmonary hypertension, while ECMO factors include poor performance of the artificial lungs and recirculation. Recirculation is a phenomenon in which oxygenated blood from the return cannula is drained from the drainage cannula without being used in the peripheral tissues. The recirculation rate can be calculated by the following formula (normal range, 0.3–0.5).
-
Recirculation rate (R) = (SpreO2 − SvO2)/(SpostO2 − SvO2)
-
SvO2: Oxygen saturation in central vein
-
Serial increase in SpreO2 or serial decrease in SaO2 is a sign of resuscitation. If the recirculation rate is high, the ECMO flow should be lowered or the tip distance between the drainage and the return cannulae should be increased.
Complications
Major complications in the management of ECMO include bleeding, thrombosis, infection, and mechanical problems. Since hemorrhage can induce systemic coagulation failure, complete hemostasis is important if it is detected. Suturing and ablation, as well as blood transfusion, are necessary.
The prolonged ECMO management can be associated with the increased risk of infection. Pathogenic microorganisms include gram-positive cocci, gram-negative bacilli, and fungi. However, prophylactic administration of antibiotics is usually unnecessary, because no evidences supported that they reduce the risk of developing infection. Because several drugs, such as beta-lactams, carbapenems, and antifungals, can be adsorbed on the ECMO circuit, it is necessary to investigate the characteristics of each drug before administration.
Replacement of ECMO circuit is necessary when white or black thrombus becomes prominent in the artificial lung or cannula and the oxygenation capacity of the artificial lung starts to decline. Decreased platelets, elevated D-dimer, elevated thrombin-antithrombin III complex (TAT), and decreased fibrinogen may also be complementary indicators of deteriorated function of artificial lung. If the PaO2 in the return cannula is less than 300 mmHg, deteriorated function of artificial lung is strongly suspected. Repeated training is required to complete the replacement of the ECMO circuit in less than 1 min at the latest.
Weaning from ECMO
Once the primary lung disease has sufficiently improved, withdrawal of ECMO will be attempted. First, change the ventilator settings to controlled ventilation mode, FIO2 of 0.4–0.6, plateau pressure of 20–25 cm H2O, PEEP of 10 cm H2O, and respiratory rate of 10–14 breaths/min, respectively. Next, the sweep gas flow rate is set to zero. After observing the patient for 30 to 120 min, the cannula will be removed after confirming no decrease in PaO2, increase in PaCO2, tachycardia, tachypnea, restlessness, or increase in respiratory workload. Normal skin sutures are sufficient for removal of cannulae.
Clinical evidences
The EOLIA trial [64] an international prospective RCT that investigated the efficacy of V-V ECMO in patients with severe ARDS. A total of 249 patients were included, and 44 of 124 patients (35%) in the ECMO group and 57 of 125 (46%) in the control group had died at 60-day follow-up. The primary endpoint of 60-day mortality showed no significant benefit of early use of ECMO compared with a strategy of conventional mechanical ventilation (35% vs 46%; p = 0.09). However, this study was a crossover trial, which included a total of 35 patients (28%) in the control group received ECMO for refractory hypoxemia. If the crossover to ECMO in the control group was defined as treatment failure, the relative risk of treatment failure was 0.62 (95%CI, 0.47–0.82; p < 0.001).
Munshi et al. [65] conducted a meta-analysis to evaluate the benefit V-V ECMO in patients with ARDS. They included 5 studies, 2 RCTs, and 3 observational studies with a total of 773 patients. In the primary outcome of 60-day mortality, the use of V-V ECMO was associated with the better outcome compared with the use of conventional mechanical ventilation (34% vs 47%; RR, 0.73; 95%CI, 0.58–0.92; p = 0.008). Combes et al. [66] further collected individual patient data and conducted a meta-analysis of RCTs. Seventy-seven (36%) of the ECMO group and 103 (48%) of the control group had died on day 90. The risk ratio of 90-day treatment failure, defined as death for the ECMO group and death or crossover to ECMO for the control group was 0.65 (95%CI, 0.52–0.80). This meta-analysis of individual patient data also supported the previous meta-analysis by Munshi et al. [65].
Aoyama et al. [67] investigated the associations of currently available ventilatory strategies and adjunctive therapies with mortality to determine the best intervention for reducing mortality in adult patients with moderate to severe ARDS. They have included a total of 25 RCTs evaluating 9 interventions for Bayesian random-effects network meta-analyses. A total of 2686 of 7743 patients (35%) died within 28 days. They found that prone positioning was associated with lower 28-day mortality compared with lung-protective ventilation alone. In patients with severe ARDS, V-V ECMO was associated with lower 28-day mortality. This network meta-analysis did not find any associations of recruitment maneuvers or higher PEEP with mortality. Inhaled nitric oxide was associate with an increased risk for renal failure with no significant mortality benefit. The effect of neuromuscular blockade was similar to the results of the ROSE trial [68] and did not improve mortality in patients with moderate to severe ARDS.
Conclusions
I have discussed the recent advances in the oxygen administration for patients with ARDS. Lung-protective ventilation remains the mainstay of respiratory management in ARDS, whereas the benefit of recruitment maneuver or high PEEP is not confirmed. Although ECMO has the potential to be a new procedure of oxygen administration for patients with ARDS, each physician should also become proficient in managing complications and troubles for improving patient outcome.
Availability of data and materials
Not applicable
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CaO2 :
-
Oxygen content
- CI:
-
Confidence interval
- COVID-19:
-
Coronavirus disease-19
- CT:
-
Computed tomography
- DAD:
-
Diffuse alveolar damage
- DO2 :
-
Oxygen supply
- DpostO2 :
-
Oxygen supply after the artificial lung
- DpreO2 :
-
Oxygen supply before the artificial lung
- ECMO:
-
Extracorporeal membrane oxygenation
- ELSO:
-
Extracorporeal Life Support Organization
- FIO2 :
-
Fraction of inspiratory oxygen
- HFNC:
-
High-flow nasal cannula
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- NPPV:
-
Non-invasive positive pressure ventilation
- OR:
-
Odds ratio
- P 0.1 :
-
Airway occlusion pressure
- PaCO2 :
-
Partial pressure of carbon dioxide
- PaO2 :
-
Partial pressure of arterial oxygen
- PBW:
-
Predicted body weight
- PEEP:
-
Positive end-expiratory pressure
- P occ :
-
Airway pressure during an end-expiratory airway occlusion
- P plat :
-
Plateau pressure
- P-SILI:
-
Patient self-inflicted lung injury
- PSV:
-
Pressure support ventilation
- RCT:
-
Randomized clinical trial
- ROC:
-
Receiver operating characteristics
- SIMV:
-
Synchronized intermittent mandatory ventilation
- SpO2 :
-
Oxygen saturation
- SpostO2 :
-
Oxygen saturation after the artificial lung
- SpreO2 :
-
Oxygen saturation before the artificial lung
- SvO2 :
-
Oxygen saturation in central vein
- TAT:
-
Thrombin-antithrombin III complex
- VAP:
-
Ventilator-associated pneumonia
- VIDD:
-
Ventilator-induced diaphragm dysfunction
- VILI:
-
Ventilator-induced lung injury
- VO2 :
-
Oxygen consumption
- V-V:
-
Venoveous
References
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–33.
Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2(7511):319–23.
Zambon M, Vincent JL. Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest. 2008;133(5):1120–7.
Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD. Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med. 2009;37(5):1574–9.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: The Berlin definition. JAMA. 2012;307(23):2526–33.
Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Taylor Thompson B, Marco RV. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38(10):1573–82.
Esnault P, Cardinale M, Hraiech S, Goutorbe P, Baumstrack K, Prud’homme E, Bordes J, Forel J-M, Meaudre E, Papazian L, Guervilly C. High respiratory drive and excessive respiratory efforts predict relapse of respiratory failure in critically ill patients with COVID-19. Am J Respir Crit Care Med. 2020;202(8):1173–8.
Bertoni M, Spadaro S, Goligher EC. Monitoring patient respiratory effort during mechanical ventilation: lung and diaphragm-protective ventilation. Crit. Care. 2020;24(1):106.
Telias I, Damiani F, Brochard L. The airway occlusion pressure (P 0.1) to monitor respiratory drive during mechanical ventilation: increasing awareness of a not-so-new problem. Intensive Care Med. 2018;44(9):1532–5.
Telias I, Junhasavasdikul D, Rittayamai N, Piquilloud L, Chen L, Ferguson ND, Goligher EC, Brochard L. Airway occlusion pressure as an estimate of respiratory drive and inspiratory effort during assisted ventilation. Am J Respir Crit Care Med. 2020;201(9):1086–98.
de Wit M, Pedram S, Best AM, Epstein SK. Observational study of patient-ventilator asynchrony and relationship to sedation level. J Crit Care. 2009;24(1):74–80.
Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32(10):1515–22.
Mauri T, Yoshida T, Bellani G, Goligher EC, Carteaux G, Rittayamai N, Mojoli F, Chiumello D, Piquilloud L, Grasso S, Jubran A, Laghi F, Magder S, Pesenti A, Loring S, Gattinoni L, Talmor D, Blanch L, Amato M, Chen L, Brochard L, Mancebo J. Esophageal and transpulmonary pressure in the clinical setting: meaning, usefulness and perspectives. Intensive Care Med. 2016;42(9):1360–73.
Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L. Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med. 2008;34(8):1477–86.
Pohlman MC, McCallister KE, Schweickert WD, Pohlman AS, Nigos CP, Krishnan JA, Charbeneau JT, Gehlbach BK, Kress JP, Hall JB. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit Care Med. 2008;36(11):3019–23.
de Haro C, López-Aguilar J, Magrans R, Montanya J, Fernández-Gonzalo S, Turon M, Gomà G, Chacón E, Albaiceta GM, Fernández R, Subirà C, Lucangelo U, Murias G, Rué M, Kacmarek RM, Blanch L. Double cycling during mechanical ventilation: frequency, mechanisms, and physiologic implications. Crit Care Med. 2018;46(9):1385–92.
Yoshida T, Nakamura MAM, Morais CCA, Amato MBP, Kavanagh BP. Reverse triggering causes an injurious inflation pattern during mechanical ventilation. Am. J. Respir. Crit. Care Med. 2018;198(8):1096–9.
Pham T, Telias I, Piraino T, Yoshida T, Brochard LJ. Asynchrony consequences and management. Crit. Care Clin. 2018;34(3):325–41.
Telias I, Beitler JR. Reverse triggering, the rhythm dyssynchrony: potential implications for lung and diaphragm protection. Am. J. Respir. Crit. Care Med. 2021;203(1):5–6.
Rodriguez PO, Tiribelli N, Fredes S, Gogniat E, Plotnikow G, Ceballos IF, Pratto R, Raimondi A, Guaymas M, Ilutovich S, San Roman E, Madorno M, Maskin P, Brochard L, Setten M. Prevalence of reverse triggering in early ARDS: Results from a multicenter observational study. Chest. 2021;159(1):186–95.
Vassilakopoulos T, Petrof BJ. Ventilator-induced diaphragmatic dysfunction. Am. J. Respir. Crit. Care Med. 2004;169(3):336–41.
Sassoon CSH. Ventilator-associated diaphragmatic dysfunction. Am. J. Respir. Crit. Care Med. 2002;166(8):1017–8.
Hermans G, Agten A, Testelmans D, Decramer M, Gayan-Ramirez G. Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care. 2010:14(4).
Jaber S, Petrof BJ, Jung B, Chanques G, Berthet JP, Rabuel C, Bouyabrine H, Courouble P, Koechlin-Ramonatxo C, Sebbane M, Similowski T, Scheuermann V, Mebazaa A, Capdevila X, Mornet D, Mercier J, Lacampagne A, Philips A, Matecki S. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans. Am J Respir Crit Care Med. 2011;183(3):364–71.
Gottesman E, McCool FD. Ultrasound evaluation of the paralyzed diaphragm. Am J Respir Crit Care Med. 1997;155(5):1570–4.
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, Rittayamai N, Lanys A, Tomlinson G, Singh JM, Bolz SS, Rubenfeld GD, Kavanagh BP, Brochard LJ, Ferguson ND. Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192(9):1080–8.
Esteban A, Anzueto A, Frutos F, Alía I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguía C, Nightingale P, Arroliga AC, Tobin MJ. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. J Am Med Assoc. 2002;287(3):345–55.
Supinski GS, Ann Callahan L. Diaphragm weakness in mechanically ventilated critically ill patients. Crit Care. 2013:17(3).
Demoule A, Girou E, Richard JC, Taille S, Brochard L. Benefits and risks of success or failure of noninvasive ventilation. Intensive Care Med. 2006;32(11):1756–65.
Dres M, Dube BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med. 2017;195(1):57–66.
McCool FD, Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med. 2012;366(10):932–42.
Mayo P, Volpicelli G, Lerolle N, Schreiber A, Doelken P, Vieillard-Baron A. Ultrasonography evaluation during the weaning process: the heart, the diaphragm, the pleura and the lung. Intensive Care Med. 2016;42(7):1107–17.
Dubé BP, Dres M, Mayaux J, Demiri S, Similowski T, Demoule A. Ultrasound evaluation of diaphragm function in mechanically ventilated patients: comparison to phrenic stimulation and prognostic implications. Thorax. 2017;72(9):811–8.
Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care. 2017;30(1):37–43.
Dinino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax. 2014;69(5):423–7.
Kim WY, Suh HJ, Hong S-B, Koh Y, Lim C-M. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39(12):2627–30.
Hudson MB, Smuder AJ, Nelson WB, Bruells CS, Levine S, Powers SK. Both high level pressure support ventilation and controlled mechanical ventilation induce diaphragm dysfunction and atrophy. Crit Care Med. 2012;40(4):1254–60.
Gayan-Ramirez G, Testelmans D, Maes K, Rácz GZ, Cadot P, Zádor E, Wuytack F, Decramer M. Intermittent spontaneous breathing protects the rat diaphragm from mechanical ventilation effects. Crit Care Med. 2005;33(12):2804–9.
Marin-Corral J, Dot I, Boguña M, Cecchini L, Zapatero A, Gracia MP, Pascual-Guardia S, Vilà C, Castellví A, Pérez-Terán P, Gea J, Masclans JR. Structural differences in the diaphragm of patients following controlled vs assisted and spontaneous mechanical ventilation. Intensive Care Med. 2019;45(4):488–500.
Lindqvist J, Van Den Berg M, Van Der Pijl R, Hooijman PE, Beishuizen A, Elshof J, De Waard M, Girbes A, Spoelstra-De Man A, Shi ZH, Van Den Brom C, Bogaards S, Shen S, Strom J, Granzier H, Kole J, Musters RJP, Paul MA, Heunks LMA, Ottenheijm CAC. Positive end-expiratory pressure ventilation induces longitudinal atrophy in diaphragm fibers. Am J Respir Crit Care Med. 2018;198(4):472–85.
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Vorona S, Sklar MC, Rittayamai N, Lanys A, Murray A, Brace D, Urrea C, Reid WD, Tomlinson G, Slutsky AS, Kavanagh BP, Brochard LJ, Ferguson ND. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018;197(2):204–13.
Frat J-P, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira J-P, Argaud L, Chakarian J-C, Ricard J-D, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin J-M, Tonnelier J-M, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard J-CM, Brochard L, Robert R. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–96.
Frat JP, Ragot S, Girault C, Perbet S, Prat G, Boulain T, Demoule A, Ricard JD, Coudroy R, Robert R, Mercat A, Brochard L, Thille AW. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med. 2016;4(8):646–52.
Kang BJ, Koh Y, Lim CM, Huh JW, Baek S, Han M, Seo HS, Suh HJ, Seo GJ, Kim EY, Hong SB. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41(4):623–32.
Roca O, Caralt B, Messika J, Samper M, Sztrymf B, Hernández G, García-De-Acilu M, Frat JP, Masclans JR, Ricard JD. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019;199(11):1368–76.
Azoulay E, Lemiale V, Mokart D, Nseir S, Argaud L, Pène F, Kontar L, Bruneel F, Klouche K, Barbier F, Reignier J, Berrahil-Meksen L, Louis G, Constantin JM, Mayaux J, Wallet F, Kouatchet A, Peigne V, Théodose I, Perez P, Girault C, Jaber S, Oziel J, Nyunga M, Terzi N, Bouadma L, Lebert C, Lautrette A, Bigé N, Raphalen JH, Papazian L, Darmon M, Chevret S, Demoule A. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH Randomized Clinical Trial. JAMA 2018;320(20):2099–107.
Duan J, Han X, Bai L, Zhou L, Huang S. Assessment of heart rate, acidosis, consciousness, oxygenation, and respiratory rate to predict noninvasive ventilation failure in hypoxemic patients. Intensive Care Med. 2017;43(2):192–9.
Innocenti F, Giordano L, Gualtieri S, Gandini A, Taurino L, Nesa M, Gigli C, Becucci A, Coppa A, Tassinari I, Zanobetti M, Caldi F, Pini R. Prediction of mortality with the use of noninvasive ventilation for acute respiratory failure. Respir Care. 2020;65(12):1847–56.
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8.
Simonis FD, Serpa Neto A, Binnekade JM, Braber A, Bruin KCM, Determann RM, Goekoop GJ, Heidt J, Horn J, Innemee G, De Jonge E, Juffermans NP, Spronk PE, Steuten LM, Tuinman PR, De Wilde RBP, Vriends M, Gama De Abreu M, Pelosi P, Schultz MJ. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial. JAMA. 2018;320(18):1872–80.
Constantin JM, Jabaudon M, Lefrant JY, Jaber S, Quenot JP, Langeron O, Ferrandière M, Grelon F, Nanadougmar H, et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir Med. 2019;7(10):870–80.
Rappaport SH, Shpiner R, Yoshihara G, Wright J, Chang P, Abraham E. Randomized, prospective trial of pressure-limited versus volume-controlled ventilation in severe respiratory failure. Crit Care Med. 1994;22(1):22–32.
Prella M, Feihl F, Domenighetti G. Effects of short-term pressure-controlled ventilation on gas exchange, airway pressures, and gas distribution in patients with acute lung injury/ARDS: comparison with volume-controlled ventilation. Chest. 2002;122(4):1382–8.
Chiumello D, Pelosi P, Calvi E, Bigatello LM, Gattinoni L. Different modes of assisted ventilation in patients with acute respiratory failure. Eur Respir J. 2002;20(4):925–33.
Davis WB, Rennard SI, Bitterman PB, Crystal RG. Pulmonary oxygen toxicity: early reversible changes in human alveolar structures induced by hyperoxia. N Engl J Med. 1983;309(15):878–83.
Chu DK, Kim LHY, Young PJ, Zamiri N, Almenawer SA, Jaeschke R, Szczeklik W, Schünemann HJ, Neary JD, Alhazzani W. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): a systematic review and meta-analysis. Lancet. 2018;391(10131):1693–705.
Barbateskovic M, Schjørring OL, Russo Krauss S, Jakobsen JC, Meyhoff CS, Dahl RM, Rasmussen BS, Perner A, Wetterslev J. Higher versus lower fraction of inspired oxygen or targets of arterial oxygenation for adults admitted to the intensive care unit. Cochrane Database Syst. Rev. 2019;2019(11):CD012631.
ICU-ROX Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group, Mackle D, Bellomo R, Bailey M, Beasley R, Deane A, Eastwood G, Finfer S, Freebairn R, Victoria King I-RI the A and NZICSCTG. Conservative oxygen therapy during mechanical ventilation in the ICU. N Engl J Med. 2020;382(11):989–98.
Barrot L, Asfar P, Mauny F, Winiszewski H, Montini F, Badie J, Quenot J-P, Pili-Floury S, Bouhemad B, Louis G, Souweine B, Collange O, Pottecher J, Levy B, Puyraveau M, Vettoretti L, Constantin J-M, Capellier G. Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med. 2020;382(11):999–1008.
Extracorporeal Life Support Organization (ELSO). Guidelines for adult respiratory failure [Internet]. 2017. Available from: https://www.elso.org/Portals/0/ELSO Guidelines For Adult Respiratory Failure 1_4.pdf
Combes A, Brodie D, Bartlett R, Brochard L, Brower R, Conrad S, De Backer D, Fan E, Ferguson N, Fortenberry J, Fraser J, Gattinoni L, Lynch W, MacLaren G, Mercat A, Mueller T, Ogino M, Peek G, Pellegrino V, Pesenti A, Ranieri M, Slutsky A, Vuylsteke A. Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. 2014;190(5):488–96.
Shekar K, Badulak J, Peek G, Boeken U, Dalton HJ, Arora L, Zakhary B, Ramanathan K, Starr J, Akkanti B, Antonini MV, Ogino MT, Raman L, Barret N, Brodie D, Combes A, Lorusso R, MacLaren G, Müller T, Paden M, Pellegrino V. Extracorporeal Life Support Organization Coronavirus Disease 2019 Interim Guidelines: a consensus document from an international group of interdisciplinary extracorporeal membrane oxygenation providers. ASAIO J. 2020;66(7):707–21.
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, DeBoisblanc B, Connors AF, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75.
Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, Da Silva D, Tirot P, Zafrani L, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Brodie D, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Mercat A. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Munshi L, Walkey A, Goligher E, Pham T, Uleryk EM, Fan E. Venovenous extracorporeal membrane oxygenation for acute respiratory distress syndrome: a systematic review and meta-analysis. Lancet Respir Med. 2019;7(2):163–72.
Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, Dechartres A, Elbourne D. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 2020;46(11):2048–57.
Aoyama H, Uchida K, Aoyama K, Pechlivanoglou P, Englesakis M, Yamada Y, Fan E. Assessment of therapeutic interventions and lung protective ventilation in patients with moderate to severe acute respiratory distress syndrome: a systematic review and network meta-analysis. JAMA Netw open. 2019;2(7):e198116.
Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, Gong MN, Grissom CK, Gundel S, Hayden D, Duncan Hite R, Hou PC, Hough CL, Iwashyna TJ, Khan A, Liu KD, Talmor D, Taylor Thompson B, Ulysse CA, Yealy DM, Angus DC. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380(21):1997–2008.
Acknowledgements
Not applicable
Funding
This work was supported by KAKENHI Grants from the Japan Society for the Promotion of Science (JSPS) (number JP 20K08541) as well as the Strategic Information and Communications R&D Promotion Programme (SCOPE) and Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Contributions
SO conceived, drafted, and proofread the manuscript. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
None declared
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ohshimo, S. Oxygen administration for patients with ARDS. j intensive care 9, 17 (2021). https://doi.org/10.1186/s40560-021-00532-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-021-00532-0