Abstract
Objectives
The aim of this study is to introduce a novel 3D cephalometric analysis (3DCA) and to validate its use in evaluating the reproducibility of virtual orthodontic-surgical planning (VOSP) in surgery-first approach (SF) comparing VOSP and post-operative outcome (PostOp).
Methods
The cohort of nineteen patients underwent bimaxillary orthognathic surgery following the VOSP designed in SimPlant O&O software by processing cone-beam computed tomography (CBCT) scans and intraoral digital scanning of the dental arches. Said records were re-acquired once the post-operative orthodontic treatment was completed. The 3DCA was performed by three expert operators on VOSP and PostOp 3D models. Descriptive statistics of 3DCA measures were evaluated, and outcomes were compared via Wilcoxon test.
Results
In the comparison between cephalometric outcomes against planned ones, the following values showed significant differences: Wits Index, which suggests a tendency towards skeletal class III in PostOp (p = 0.033); decreased PFH/AFH ratio (p = 0.010); decreased upper incisors inclination (p < 0.001); and increased OVJ (p = 0.001). However not significant (p = 0.053), a tendency towards maxillary retroposition was found in PostOp (A/McNamara VOSP: 5.05 ± 2.64 mm; PostOp: 4.1 ± 2.6 mm). On average, however, when McNamara’s plane was considered as reference, a tendency to biprotrusion was found. Upper incisal protrusion was greater in PostOp as an orthodontic compensation for residual maxillary retrusion (VOSP: 5.68 ± 2.56 mm; PostOp: 6.53 ± 2.63 mm; p = 0.084). Finally, the frontal symmetry in relation to the median sagittal plane decreased in craniocaudal direction.
Limitations
A potential limit of studies making use of closest point distance analysis is represented by the complexity that surgeons and orthodontists face in applying this three-dimensional evaluation of SF accuracy/predictability to everyday clinical practice and diagnosis. Also, heterogeneity and limited sample size may impact the results of the study comparison.
Conclusions
The presented 3DCA offers a valid aid in performing VOSP and analysing orthognathic surgery outcomes, especially in SF. Thanks to the cephalometric analysis, we found that surgery-first approach outcome unpredictability is mainly tied to the sagittal positioning of the maxilla and that the transverse symmetry is progressively less predictable in a craniocaudal direction.
Similar content being viewed by others
Introduction
In orthognathic surgery, surgery-first approach (SF) is an increasingly popular alternative to the conventional orthodontics-first approach (OF), with a growing body of the literature and interest from orthodontists, surgeons, and patients themselves. Alfaro et al. reported 18.8% of their orthognathic cases are treated by means of SF [1].
When compared to standard OF, the SF approach is tied to higher uncertainty in terms of both morphological and occlusal results; the main drawback of SF is the challenge in predicting combined skeletal and dental movements, since teeth cannot guide the planning of skeletal movements [2]. Therefore, SF requires a clear definition of the dentoskeletal deformity, a personalized orthodontic-surgical planning and accurate reproduction of the surgical planning in theatre and orthodontics post-operatively. Only if these conditions are met, the outcome can be both accurate and predictable [3].
To overcome this limitation, recent improvements in both orthodontics and surgery can be integrated to increase the accuracy of said approach [4]. Alfaro et al. [5] described a specific orthodontic and surgical protocol for SF, discussing the benefits and limitations of this treatment. We also presented a new computer-assisted method, which combines virtual orthodontic planning (VOP) and virtual surgical planning (VSP) into a virtual orthodontic-surgical planning (VOSP) to simulate the treatment [6].
By overlapping three-dimensional surfaces in a post-operative analysis, the VOSP demonstrated to be reliably transferred to the patient. However, a limit of studies making use of surface comparison evaluation is the complex, and at times not univocal, interpretation of results given by such method [7].
With its many facets and uncertainties, both on the skeletal and dental side, SF outcome analysis is a perfect test bench for a diagnostic tool such as three-dimensional cephalometry (3DCA), which carries the advantages of allowing a more standardized interpretation and a stronger correlation to clinical outcomes.
On a literature basis, we selected 3D cephalometric measurements which transpose 2D cephalometry in a three-dimensional environment [8, 9], adding new measurements which are purely three-dimensional [10,11,12,13]. Thus, we here introduce a 3DCA based on our clinical practice, by means of which we analysed a cohort of SF patients, with the aim of deepening our comprehension of the uncertain aspects in this approach.
Materials and methods
Study design
Nineteen consecutive Caucasian patients who presented with dentofacial deformities at the Oral and Maxillofacial Surgery Unit of the S. Orsola University Hospital in Bologna (Italy) were enrolled between 2013 and 2019 and treated with a SF approach, according to the inclusion/exclusion criteria listed in Table 1.
This monocentric prospective protocol was approved in 2013 by our local ethics committee. The study conformed to the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients upon enrolment in the trial.
Eleven males and eight females were enrolled in the study, with mean age 26.5 years (range 18–55 years). The cohort was composed of 65% class 3, 30% class 2, and 5% class 1 patients.
Each patient underwent the workflow described below:
Data acquisition
Patients underwent CBCT scan (VGi; NewTom, Verona, Italy) with a 19 × 19 field-of-view (FOV) and intraoral digital scanning of the dental arches (Trios; 3Shape, Copenhagen, Denmark) in the pre-operative phase.
The DICOM datasets and the STL files were processed using the SimPlant O&O platform (Dentsply-Sirona; York, PA, USA), to produce an accurate 3D model of the patient’s hard and soft tissues. The 3DCA completed the diagnostic process; VOSP was subsequently performed on the 3D models.
3D cephalometry
3D cephalometry was performed by three expert operators (two orthodontists and one maxillofacial surgeon) for each patient using the Simplant O&O Software.
The three analyses performed were compared via a Friedman test for inter-operator concordance. Once the concordance was ascertained, the average of each value was used in further comparisons.
The authors developed a specific 3DCAderived from traditional 2D analyses (Ricketts, McNamara, Arnett, Tweed) plus several measurements regarding both vertical and transverse symmetry, which are only possible in three-dimensional studies, with the aim of identifying an array of clinically relevant landmarks and measurements in orthodontic-surgical patient treatment [14].
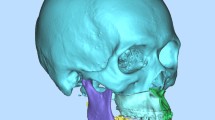
The analysis consists of 42 skeletal and dental landmarks, listed in Table 2, that the operator selects on patient’s 3D reconstruction (Fig. 1) and on the three-plane reslicing of the CT images.
Part of these points are used by the software to generate reference planes, which are listed in Table 3 and shown in Fig. 2. Based on these points and planes, linear and angular measurements are computed by the software according to the rules set by the clinician.
Sagittal skeletal analysis
The sagittal skeletal analysis includes the so-called strictly sagittal parameters which identify the skeletal class, anterior/posterior position of the jaw, divergence, and facial type of the patient. It also includes sagittal symmetry values.
Moreover, the linear measurements of both sides (right and left) are compared computing the difference between the two (△) (Fig. 3, Table 4).
Frontal skeletal analysis
The frontal skeletal analysis focuses on frontal symmetry, using both midline parameters, which represent the distances in millimetres of the points ANS, A, B and Pog from the sagittal plane and differences between distances of theoretically symmetrical points from the sagittal plane (Fig. 4, Table 5).
Vertical skeletal analysis
The vertical skeletal analysis allows clinicians to evaluate the patient’s vertical proportions and classify them as a long / short face. It also includes vertical symmetry values. (Fig. 5, Table 6).
Sagittal dento-alveolar analysis
The dento-alveolar sagittal analysis evaluates the incisors’ position in respect to the maxillary and mandibular bone, in respect to the occlusal plane and in respect to each other (Fig. 6, Table 7).
Frontal dento-alveolar analysis
The dento-alveolar frontal analysis evaluates the distance between the inter-incisal line, canines and molars to the sagittal plane (Fig. 7, Table 8).
Vertical dento-alveolar analysis
The dento-alveolar vertical analysis evaluates the vertical distance between the cusp of the upper canine and the mesiovestibular cusp of the first upper molar and the Frankfurt plane (Fig. 8, Table 9).
Virtual planning
Virtual orthodontic planning (VOP)
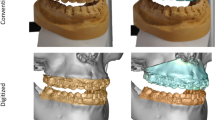
For each patient, an individualized orthodontic treatment was planned (VOP), to simulate orthodontic decompensation and to simulate the pursued occlusion when planning skeletal movements. During the VOP, teeth are positioned in an ideal virtual arch (IVA) (Fig. 9); then, the IVAs were registered to the skeletal base in a manner compatible with the native arches (Fig. 9a–c).
VOSP wokflow. Figures are labelled form top left to bottom right. A, Patient 3D reconstruction; B, The ideal virtual arches of both arches were registered on the skeletal base, superimposed on the native arches; C, Skeletal base with ideal virtual arches; D,E, Virtual osteotomy of the base of the facial skeleton with ideal virtual arch and both ideal and native; F, Virtual surgical plan: repositioning of the upper jaw, followed by the virtually planned dental arches; G, Positioning of the lower jaw by reference to the ideal virtual occlusion; and H upper and lower jaw surgical virtual planning with native arches
Virtual surgical planning (VSP)
In VSP, virtual osteotomies (i.e. LeFort 1, BSSO and/or segmental osteotomy, Fig. 9d, e) are performed on the patient model and subsequently the skeletal segments are repositioned to fulfil both aesthetic and cephalometric criteria (aiming for norm values), within a range of surgical feasibility. First, the upper jaw is repositioned (Fig. 9f) with the native dental arch and upper IVA. Then, the lower jaw is positioned to simulate an ideal virtual occlusion via coordination of both upper and lower IVAs. (Fig. 9g).
After the simulation, a new 3D cephalometry was performed on the virtual setup.
Treatment
Pre-operatively a passive arch wire was positioned 48 h before surgery. We did not use temporary anchorage devices and did not perform corticotomies.
Surgery was performed without the aid of any additional patient-specific devices (i.e. surgical cutting guides and/or patient-specific implants) besides CAD/CAM surgical splints. Maxillary and mandibular osteosynthesis was obtained using standard titanium miniplates and screws [15, 16]. Patients wore the final surgical splints for 30 days (12–24 h/day) in the post-operative phase. After that, post-operative orthodontic treatment started with replacement of orthodontic wires every 2–3 weeks.
Once the orthodontic treatment was completed, all patients underwent a follow-up CBCT (without braces, at maximum intercuspation) as well as a post-treatment scan of the dental arches. These datasets were used to obtain 3D soft and hard tissue models, on which a new 3D cephalometric study (PostOp) was performed. Mean and standard deviations of the values obtained were considered.
Planned and post-treatment cephalometric measures were compared.
Statistical analysis
Descriptive statistics (mean and standard deviation) were used to summarize the data, comparing VOSP and PostOp cephalometric analysis. All symmetry measurements were tabulated both as signed and absolute values. The nonparametric Wilcoxon test was used to compare the cephalometric analyses. The significance level was set to α = 0.05.
Results
VOSP and PostOp 3D Cephalometric data are listed in Table 10.
According to the Sagittal skeletal analysis, in both VOSP and PostOp, jaws resulted on average in a slight biprotrusion, as the distances of points A, B, and Pog from their projections on the McNamara plane were increased when compared to their respective standards. However, the post-operative upper jaw appeared to remain retro-positioned when compared to the planned position; this difference, represented by the A/McNamara distance, is close to statistical significance (p = 0.053).
We also observed a slight mean tendency towards skeletal class III in both VOSP and PostOp Wits analysis. When compared, the obtained results appear to be significantly different from the planned ones (p = 0.033).
Sagittal dento-alveolar analysis showed that the upper incisor is more protruded in the post-treatment sample, and slightly outside the normal ranges described by James A. McNamara Jr. Accordingly, upper incisor inclination (UIs/Occulsal) is more acute post-treatment (p < 0.001).
Regarding the Tweed angle, we obtained an average tendency to hypodivergence, but the norm value still lies within the standard deviation of our cohort.
The strictly frontal values showed a progressively increasing deviation from the sagittal plane in craniocaudal direction, both in VOSP and PostOp (Subnasal Deviation (ANS–SagPL), Maxillary Deviation (A–SagPL), Mandibular Deviation (B–SagPL), Mental Deviation (Pog–SagPL)).
The dento-alveolar frontal analysis showed an increase in the inter-incisal midline deviation in the post-operative outcome compared to planning; however, it was not statistically significant.
The average distance from the sagittal plane and deltas of canine and molars do not show statistically significant differences, and the same applies to the dento-alveolar vertical analysis.
Overbite was slightly less in VOSP, while overjet differed between plan and outcome by around 1 mm; however, only the latter was statistically significant.
Discussion
3DCA is poorly described in the literature, and no general consensus has been reached regarding standard landmarks and measurements to adopt [8, 11, 13, 17]. To our knowledge, no study describes a 3D cephalometric analysis to be employed as a diagnostic and planning tool with a focus on surgery-first approach.
Although an already established approach, some aspects of SF need further investigation to improve its reliability. In particular, we focused on the description of its shortcomings in VSP reproducibility by means of a 3D cephalometry.
In our cohort, the maxillary position compared to VSP was, on average, less advanced by around 1 mm, as demonstrated by the difference in A–SagPL close to statistical significance (p = 0.053) (Fig. 10). This result can be partly attributed to the less optimal occlusal stability during the peri-surgical period, partly to a posterior displacement of the A point for intraoperative aesthetic management by means of maxillary reshaping, and partly to posterior condylar sagging in the fossa when guiding the upper maxilla into position [18].
The retruded position of the maxilla is also indicated by the dento-alveolar sagittal analysis score of incisal protrusion, which is greater than planned (5.68 ± 2.56 mm) in the post-operative outcome (6.53 ± 2.63 mm). This can be explained by the inevitable orthodontic compensation that must be performed after maxillary repositioning, a positive torque is set on the central incisors to obtain a correct occlusal relationship. These data find further confirmation in the incisal inclination value, which is more acute post-treatment (53.85 ± 4.77°) compared to the planned one (59.65 ± 4.94°) (Fig. 11), and in the increased post-operative overjet value (VOSP: 1,93 ± 0,84 mm; PostOp: 3,11 ± 0,8 mm). Moreover, the increased occlusal instability is likely to require greater mandibular compensation. Overall, it can be hypothesized that the unpredictability inherent to SF may lead to a slight, clinically imperceptible, under-correction of the dysmorphism.
Although the upper maxilla was less advanced than planned, patients showed, on average, maxillo-mandibular protrusion when McNamara’s plane was considered as reference. This finding is in accordance with the available literature, which reports this trend to be mostly prevalent in younger patients (i.e. juvenile biprotrusion) [19]. Such finding may also be justified by an aesthetic preference for slight biprotrusion in Mediterranean countries, as reported by Pironi et al.[20].
Most patients showed a trend towards skeletal class III in the post-treatment cephalometric analysis, according to Wits index. However, it should be noted that 65% of the sample suffered from skeletal Class III malocclusion before treatment: frequently class III patients tend to show mild class III traits even after surgery, due to surgical and anatomical limitations as similarly reported in the existing literature [21, 22]. All in all, Wits index is a construction measure that cannot represent the only guide within the global case planning, in which the entirety of the aesthetic outcome must be considered; therefore, it is the authors’ opinion that a compromise on the cephalometric outcome can be accepted.
A further interesting finding is that in the cohort analysed, the frontal symmetry tends to decrease in craniocaudal direction. This phenomenon can be again related to the poorer perioperative occlusal stability, which can result in imperfect alignment of the incisor median lines as well as a slight, clinically imperceptible, roll of the maxillary segment. In fact, once the upper maxilla is correctly centred, the other frontal symmetry values may still be more prone to be displaced during the post-operative orthodontic finalization. Another reason for the under-correction of mandibular asymmetries is the possible presence of mild deformities of the mental region which cannot be fully corrected with BSSO surgery alone; thus, the sole cephalometric mandibular midline points are unreliable for an evaluation of the outcome.
A limitation of this study is tied to the non-homogeneity of the sample, due to the fact that the majority of patients were suffering from class III deformity, as it is more likely for skeletal Class III patients to undergo surgery-first approach than Class II or Class I [23]. Relapse patterns in different dysmorphisms can cancel each other on average when considered in a single cohort. However, the statistical analysis used for comparison is free from this shortcoming.
Overall, the significant differences highlighted in this analysis may deserve further analysis in class-specific cohorts for further evaluation.
A further limitation can be found in the lack of an immediately post-operative cephalometric analysis, so to be able to separate an immediate under-realization of VOSP from a relapse caused by muscle tension and dental interferences with bone remodelling during osteotomy healing. This was not performed as, in our workflow, an immediately post-operative CBCT scan is avoided to reduce the radiation exposure of the patient.
Conclusions
Our 3DCA offers a valid guide for surgeons and orthodontists in planning and analysing the outcome of orthognathic surgery procedures, also in surgery-first approach. However, operator learning curve, global landmarks uniformity and time efficiency in the execution of 3DCA can be object of further evaluation.
This analysis allowed us to evaluate specific aspects which may hinder the predictability of SF approach. Within our sample, the sagittal repositioning of the maxilla represents the main unpredictable factor, as it shows an average tendency to be less advanced compared to the planned position, and therefore leading to an orthodontic compensation via incisal protrusion and proclination. Frontal symmetry is also less controllable, particularly in its mandibular component.
Availability of data and materials
The datasets used in this study are available by request at the corresponding author.
References
Hernández-Alfaro F, Guijarro-Martínez R. On a definition of the appropriate timing for surgical intervention in orthognathic surgery. Int J Oral Maxillofac Surg. 2014;43(7):846–55.
Peiró-Guijarro MA, Guijarro-Martínez R, Hernández-Alfaro F. Surgery first in orthognathic surgery: a systematic review of the literature. Am J Orthod Dentofac Orthop Off Publ Am Assoc Orthod Const Soc Am Board Orthod. 2016;149(4):448–62.
Yang L, Xiao Y-D, Liang Y-J, Wang X, Li J-Y, Liao G-Q. Does the surgery-first approach produce better outcomes in orthognathic surgery? a systematic review and meta-analysis. J oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2017;75(11):2422–9.
Janakiraman N, Feinberg M, Vishwanath M, NalakaJayaratne YS, Steinbacher DM, Nanda R, et al. Integration of 3-dimensional surgical and orthodontic technologies with orthognathic “surgery-first” approach in the management of unilateral condylar hyperplasia. Am J Orthod Dentofac Orthop. 2015;148(6):1054–66.
Hernández-Alfaro F, Guijarro-Martínez R, Peiró-Guijarro MA. Surgery first in orthognathic surgery: what have we learned? a comprehensive workflow based on 45 consecutive cases. J Oral Maxillofac Surg. 2014;72(2):376–90.
Badiali G, Costabile E, Lovero E, Pironi M, Rucci P, Marchetti C, et al. Virtual orthodontic surgical planning to improve the accuracy of the surgery-first approach: a prospective evaluation. J Oral Maxillofac Surg. 2019. https://doi.org/10.1016/j.joms.2013.08.013.
Marlière DAA, Demétrio MS, Schmitt ARM, Lovisi CB, Asprino L, Chaves-Netto HDDM. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm and color maps: a retrospective cohort study. Med Oral Patol Oral y Cir Bucal. 2019;24(2):e243–53.
Yoshikawa H, Tanikawa C, Ito S, Tsukiboshi Y, Ishii H, Kanomi R, et al. A three-dimensional cephalometric analysis of Japanese adults and its usefulness in orthognathic surgery: a retrospective study. J Cranio-Maxillofacial Surg. 2022;50(4):353–63. https://doi.org/10.1016/j.jcms.2022.02.002.
Farronato M, Baselli G, Baldini B, Favia G, Tartaglia GM. 3D cephalometric normality range: auto contractive maps (ACM) analysis in selected caucasian skeletal class I age groups. Bioengineering. 2022;9(5):216.
Swennen GRJ, Schutyser F, Hausamen JE, Van Cleynenbreugel J. Three-dimensional cephalometry: a color atlas and manual. Three-dimensional cephalometry: a color atlas and manual. Springer Berlin Heidelberg; 2006. pp 1–365
De Oliveira LC, Masterson D, da Motta AFJ, Motta AT. Reliability and reproducibility of three-dimensional cephalometric landmarks using CBCT: a systematic review. J Appl Oral Sci. 2015;23(2):112–9.
Teng C, Liu C, Yu Q, Liu S. Cone-beam computed tomography-based three-dimensional cephalometric analysis of mandible symmetry and the occlusal plane of adult patients with high-angle skeletal class III malocclusion and jaw deformity. Arch Oral Biol. 2021;127: 105157.
Pittayapat P, Limchaichana-Bolstad N, Willems G, Jacobs R. Three-dimensional cephalometric analysis in orthodontics: a systematic review. Orthod Craniofacial Res. 2014;17(2):69–91.
Pironi M, Bianchi A, Lancellotti L, Giorgini F, Morselli-Labate AM, Marchetti C. 3D cephalometric mean values in a postsurgical esthetically balanced Italian sample. Ital J Maxillofac Surg. 2012;23(1–3):39–48.
Badiali G, Bevini M, Ruggiero F, Cercenelli L, Lovero E, De Simone E, et al. Validation of a patient-specific system for mandible-first bimaxillary surgery: ramus and implant positioning precision assessment and guide design comparison. Sci Rep. 2020;10(1):1–11.
Mazzoni S, Bianchi A, Schiariti G, Badiali G, Marchetti C. Computer-aided design and computer-aided manufacturing cutting guides and customized titanium plates are useful in upper maxilla waferless repositioning. J Oral Maxillofac Surg. 2015;73(4):701–7.
Rossini G, Cavallini C, Cassetta M, Barbato E. 3D cephalometric analysis obtained from computed tomography. Rev Lit Ann Stomatol. 2011;2(3–4):31–9.
Hoffmannová J, Foltán R, Vlk M, Klíma K, Pavlíková G, Bulik O. Factors affecting the stability of bilateral sagittal split osteotomy of a mandible. Prague Med Rep. 2008;109:286–97.
Sforza C, Laino A, D’Alessio R, Grandi G, Binelli M, Ferrario VF. Soft-tissue facial characteristics of attractive Italian women as compared to normal women. Angle Orthod. 2009;79(1):17–23.
Pironi M, Bianchi A, Lancellotti L, Giorgini F, Morselli-Labate AM, Marchetti C. 3D cephalometric mean values in a postsurgical esthetically balanced Italian sample. Italian J Maxillofacial Surg. 2012;23(1–3):39–48.
De Riu G, Virdis PI, Meloni SM, Lumbau A, Vaira LA. Accuracy of computer-assisted orthognathic surgery. J Cranio-Maxillofacial Surg. 2018;46(2):293–8.
Georgalis K, Woods MG. A study of Class III treatment: orthodontic camouflage vs orthognathic surgery. Aust Orthod J. 2015;31(2):138–48.
Park JK, Choi JY, Yang IH, Baek SH. Patient’s satisfaction in skeletal class III cases treated with two-jaw surgery using orthognathic quality of life questionnaire: Conventional three-stage method versus surgery-first approach. J Craniofac Surg. 2015;26(7):2086–93.
Acknowledgments
Not applicable.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
GB contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript, MB contributed to the analysis of the results and to the writing of the manuscript, and designed the figures, CG contributed to the writing of the manuscript and designed the figures, OL processed the experimental data, performed the analysis, drafted the manuscript and designed the figures, SIP contributed to the final version of the manuscript, MP contributed to the design and implementation of the research and the final versione of the manuscript, AB contributed to the final version of the manuscript, PF contributed to the final version of the manuscript, and CM contributed to the design and implementation of the research and the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical Approval by the Sant’Orsola-Malpighi Polyclinic Independent Ethics Committee. Approved in 2013.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Badiali, G., Bevini, M., Gulotta, C. et al. Three-dimensional cephalometric outcome predictability of virtual orthodontic-surgical planning in surgery-first approach. Prog Orthod. 23, 51 (2022). https://doi.org/10.1186/s40510-022-00448-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40510-022-00448-x