Abstract
Background
To date, the vast majority of research on disordered eating symptomatology and body image disturbances from the Arab world have been performed exclusively among women; and mainly used thinness-oriented measures that are not sensitive to detect muscularity-oriented symptoms, which are more evident in males. Therefore, the objective of our study was to validate the Arabic version of the Muscle Dysmorphic Disorder Inventory (Ar-MDDI), in order to make it accessible for Arabic-speaking populations.
Methods
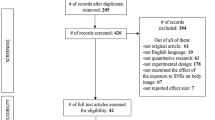
Using a snowball sampling technique, men university students (n = 396) from multiple universities in Lebanon filled the survey in this cross-sectional designed study (January–May 2022). A soft copy of the questionnaire was created using google forms software, and sent to participants through the different social media platforms such as Facebook, Instagram, and WhatsApp. We used the Muscle Dysmorphic Disorder Inventory to assess Muscle Dysmorphia, along with the Big Three Perfectionism Scale to assess perfectionism and Eating Attitude Test (EAT) to evaluate the inappropriate eating attitudes. To explore the factor structure of Ar-MDDI, we computed a principal-axis Exploratory Factor Analysis (EFA) with the first split-half subsample using the FACTOR software. We used data from the second split-half to conduct a Confirmatory Factor Analysis (CFA) using the SPSS AMOS v.29 software. Pearson correlation test was used to test the convergent and divergent validity of the Ar-MDDI scale with the other scores included in the study.
Results
The results of the EFA revealed three factors, which explained 57.68% of the common variance: Factor 1 = Appearance intolerance, Factor 2 = Drive for size, and Factor 3 = Functional impairment. The CFA fit indices of the three-factor model of the Ar-MDDI scale showed good results. Moreover, 254 (64.1%) of the participants had inappropriate eating attitudes (EAT scores ≥ 20). Indices suggested that configural, metric, and scalar invariance was supported according to eating attitudes. No significant difference between participants with appropriate versus inappropriate eating attitudes in terms of functional impairment, drive for size and appearance intolerance. Perfectionism scores correlated positively with the Ar-MDDI, which suggests divergent validity.
Conclusion
Our findings revealed that the validation of the Arabic scale yielded excellent properties, preliminarily supporting its use for the assessment of muscle dysmorphia among Arabic-speaking university men. This would hopefully allow for its timely detection and management in Arab clinical settings and encourage cross-cultural research on this topic.
Plain English Summary
Muscle dysmorphic disorder (MDD) refers to an important muscularity-oriented dimension related to eating disorder (ED) symptoms and body image disturbances. One widely used self-report measure to assess the MDD construct is the Muscle Dysmorphic Disorder Inventory (MDDI). Despite its high clinical relevance, MDD has not been previously investigated in the Lebanese context and among the Arabic-speaking communities in general. Indeed, the multiple scales assessing ED symptomatology that have previously been translated to the Arabic language and adapted to the Lebanese population have been mainly focused on thinness-oriented ED; and no Arabic validation of muscularity-oriented body image and disordered eating symptoms measures, including the MDDI, exists so far to the best of our knowledge. To overcome this gap, the present study aimed to validate the Arabic version of the MDDI (Ar-MDDI) in a sample of Lebanese men university students. The findings showed that the AR-MDDI is robust in terms of reliability, factor structure, convergent and divergent validity. We, therefore, preliminarily recommend its use in clinical practice, preventive interventions and future research in Arab settings.
Similar content being viewed by others
Background
Traditionally, research on eating disorder (ED) symptoms, weight, and body image has mainly focused on women populations [1]; while men have for a long time remained largely under-researched [2, 3]. However, in recent years growing evidence has accumulated on occurrence of ED symptoms in men [2,3,4,5,6,7], which attracted increasing attention from researchers around the world [8]. Disordered eating behaviors and body image issues have different characteristics and features across genders [9], manifesting as a drive for muscularity and leanness (body composition) in men versus a drive for thinness in women [9, 10]. Indeed, men became increasingly affected by sociocultural body ideals, that may in turn result in the development of body dissatisfaction [11, 12] and muscularity-oriented symptoms [4]. It is of note, however, that the vast majority of previous literature on ED pathology and body dissatisfaction have been performed in Western societies due to an overrepresentation of the problem in these societies [2]. Although there has been a recent rise in ED symptoms prevalence in the Arab world [13, 14], only a dearth of research has been conducted in this region. Recent meta-analyses have even shown inverted patterns of prevalence rates due to a westernization expansion, with increased risk of ED among participants from non-Western cultures as compared to those from Western cultures [15, 16]. Particularly in Lebanon, studies documented high prevalence rates of ED symptoms in clinical populations (estimated as 46.1% for bulimia nervosa, 39.4% for anorexia nervosa, and 14.4% for binge eating) [17]. Lebanese studies in non-clinical populations also showed alarmingly high prevalence of ED pathology, such as orthorexia nervosa tendencies and behaviors (75.2%) [18], restrained eating (48.3%) [19] and disordered eating attitudes (23.8–25.3%) [20] in healthy adults, and body dissatisfaction in adolescents (45.1%) [21]. Another Lebanese study found that 36% of university students were slightly to extremely worried about their body image [22]. Hoteit et al. found that 22.5% of health science students and healthcare practitioners in Lebanon were at high risk of ED [23]. Significant gender differences have also been noted in the prevalence and correlates of a range of ED symptoms in the Lebanese general population (e.g., [24,25,26]). Despite this evidence, the existing literature on ED in the Arab world in general, and Lebanon in particular, is hindered by two major limitations. The first limitation lies to the fact that, to date, the vast majority of research on disordered eating symptomatology and body image disturbances have been performed exclusively among women [27]. The second limitation is that, although several scales assessing ED symptomatology have been translated to the Arabic language and adapted to the Lebanese population, these scales have been mainly focused on thinness-oriented ED, such as the Dutch Restrained Eating Scale [28], the ORTO-R [29, 30], the Dusseldorf Orthorexia Scale [31], the Teruel Orthorexia Scale [32], and the Eating Attitude Test (EAT-7 [33], EAT-26 [20]). These measures are not sensitive to detect ED symptoms in men, of a muscularity-oriented nature [9].
The present paper focuses on an important muscularity-oriented dimension related to ED symptoms and body image disturbances, muscle dysmorphic disorder (MDD). MDD has been listed in the Diagnostic and Statistical Manual-5 (DMS-5) as a variant of body dysmorphic disorder [34]. The disorder refers to an obsessive preoccupation with muscles’ size and shape [35], perceived as small, unattractive, and/or not sufficiently muscular and lean [36,37,38,39]; which often leads to a desire to hide one’s body [35] and avoid social situations [35, 40, 41], as well as a great shame [38], and substantial social and occupational impairments [35].
Overall, MDD has been shown to have numerous health consequences (for review, see [42]). More specifically, it was found to be significantly associated with high perfectionism [42]. The negative consequences highlight the crucial necessity for adequate treatment. It is clear that a timely recognition and diagnosis of MDD plays a major role in its effective management [43]; however, some evidence has shown that men-specific eating and body dysmorphic disorders remain largely unrecognized, undetected and untreated [36, 44, 45]. This is exacerbated by men's reluctance to seek help, partially because of stigma [46]. Therefore, early screening and detection are key to intervening before symptoms become disabling and therefore reducing delays to care attributable to stigma in this specific population.
Several self-report measures have been developed to evaluate muscularity-oriented body image and disordered eating symptoms. Among them, the most commonly used is the Muscle Dysmorphic Disorder Inventory (MDDI). The MDDI [47] is an instrument consisting of 13 items on a 5-point Likert type scale (from 1 “never” to 5 “always”), and has three subscales: appearance intolerance, drive for size, and functional impairment. The latter subscale is considered a key diagnostic indicator of MDD that other measures (such as the MASS (Muscle Appearance Satisfaction Scale) or the MDI (Muscle Dysmorphic Inventory)) omit to assess [42]. MDDI has been translated in different languages and countries, including Spanish [48], Portuguese [49], Turkish [50], and Chinese [51]. However, no Arabic validation has been done so far to the best of our knowledge. This has led to a lack of research on this topic in Lebanese and the broader Arabic-speaking communities; which strongly supports the need for making instruments assessing men-specific ED symptoms available for Arabic-speaking men in Lebanon and other parts of the world. A recent literature review by Melisse et al. concluded that the existing research on ED symptoms in Arab countries “suffers from potential limitations due to the use of non-validated assessment tools”, and called for more validation studies [52].
To address the above-mention limitations, this study aimed to translate and validate the MDDI into the Arabic language, by examining its internal consistency, factorial structure, convergent and divergent validity in a sample of Lebanese men university students. We expected that (1) the Arabic version scale would have good internal consistency; (2) the MDDI would have a three-factor structure; and (3) the total scores of the scale would be significantly correlated with disordered eating attitudes and perfectionism scores, indicating both its convergent and divergent validity. Evidence for the convergent validity of the MDDI through significant strong positive correlations with ED measures has previously been demonstrated (e.g., [53]). Additionally, perfectionism has been shown as a consistent risk factor for developing muscle dysmorphia [54]; and has, therefore, been chosen as a relevant construct for divergent validity.
Methods
Participants
University men (N = 396) from multiple universities in Lebanon were invited to fill the survey. Any student enrolled in any educational level (bachelor, master or PhD) was invited to fill the survey. Participants had a mean age of 25.63 years (SD = 5.84), ranging from 18 to 60 years and had a mean self-reported body mass index (BMI) 24.46 kg/m2 (SD = 3.51), ranging from 15.82 to 47.75 kg/m2. Most participants were single (79.0%).
Our sample was chosen using the snowball technique; a digital questionnaire was created using google forms software, and an online approach was conceived to proceed with the data collection (by sending the questionnaire through the different social media platforms such as Facebook, Instagram and WhatsApp). The study’s main aims and goals, in addition to instructions for filling the questionnaire, were conveyed online for the participants, prior to their participation. Later, initial participants were asked to recruit other participants they know, preferably as diverse as possible regarding place of habitat within the Lebanese governorates and within the same age interval required to participate in the study. There were no credits received for participation.
Study design
One certified interpreter translated the MDDI scale from English into Arabic, while a second interpreter translated the Arabic version back into English. Next, the English version was assessed by a committee consisting of the research team and the two translators. There were very minor discrepancies (e.g., word choice differences) in the translation of the scale, which were resolved through consensus. The items of the MDDI scale in Arabic are presented in Additional file 1: Appendix 1.
Data collection took place between January and May 2022. Data was collected through the snowball technique, where the research team initiated the first contact with some participants by sending them the Google form link to the survey; those participants were solicited to send the link to other men they know. The link contained a brief introduction related to information about the study (e.g., objectives of the study, confidentiality of answers, estimated duration, etc.). Those who agreed to participate answered “yes” to the question related to their full willingness to participate in the study. The questionnaire took between 15 and 20 min to complete. Participation was voluntary, with no remuneration was given to any participant in return.
Translation procedure
All scales, except the Eating Attitude Test, were first translated from English into Arabic by one psychologist, then back to English from Arabic by another psychologist. The Arabic version was verified by a linguistic professional. The principal investigator compared the English version to discern any discrepancies; all procedures were done according to the international recommendations of forward-back translation [55]. The questionnaire was pilot-tested on 20 participants before data collection. As all 20 participants could interpret the items correctly without difficulties, no changes were made. Thus, the translated scales were used in the present study.
Measures
Sociodemographic information
We collected information about age, marital status and the self-reported height and weight to calculate the BMI.
Muscle dysmorphic disorder inventory
This scale is composed of 13 items, scored on a five-point Likert-type scale (0 = never to 4 = always) [47]. Three factors were previously identified: desire for size (DFS), appearance intolerance (AI), and functional impairment (FI). The Arabic items of the scale are available in Additional file 1: Appendix 1.
Big three perfectionism scale
This scale is composed of 16 items, scored on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree) [56]. It yields three subscale scores: rigid perfectionism, self-critical perfectionism and narcissistic perfectionism. Higher scores reflect higher perfectionism in the three aspects. In this study, the Cronbach’s alpha values for the three scores were as follows: rigid perfectionism (McDonald’s ω = 0.91), self-critical perfectionism (McDonald’s ω = 0.88) and narcissistic perfectionism (McDonald’s ω = 0.84).
Eating attitude test
Validated in Lebanon [20], it is composed of 26 questions rated on a six-point Likert scale; higher scores reflect more inappropriate eating attitudes [57], specifically when participants score 20 and above on the test (McDonald’s ω = 0.97).
Analytic strategy
Data treatment
There were no missing responses in the dataset. To examine the factor structure of the MDDI, we used an EFA-to-CFA strategy [58]. To ensure adequate sample sizes for both EFA and CFA, we split the main sample using the SPSS computer-generated random technique; the description of the two samples are shown in Table 1. There were no significant differences between the two subsamples in terms of mean age, t(394) = 0.02, p = 0.984, and BMI, t(393) = 1.81, p = 0.072.
Exploratory factor analysis (EFA)
To explore the factor structure of Ar-MDDI, we conducted a principal-axis EFA with the first split-half subsample using the FACTOR software [59]. We verified all requirements related to item-communality [60], average item correlations, and item-total correlations [61]. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy (which should ideally be ≥ 0.80) and Bartlett’s test of sphericity (which should be significant) ensured the adequacy of our sample [62]. The procedure followed for determining the number of dimensions was the Parallel Analysis (PA) [63]. Weighted Root Mean Square Residual (WRMR) were also calculated to assess the model fit (values < 1 have been recommended to represent good fit) [64]. Item retention was based on the recommendation that items with “fair” loadings and above (i.e., ≥ 0.33) and with low inter-item correlations (suggestive of low item redundancy) as indicated by the anti-image correlation matrix should be retained [65].
Confirmatory factor analysis (CFA)
We used data from the second split-half to conduct a CFA using the SPSS AMOS v.26 software. A previous study suggested that the minimum sample size to conduct a confirmatory factor analysis ranges from 3 to 20 times the number of the scale’s variables [66]. Therefore, we assumed a minimum sample of 130 participants needed to have enough statistical power based on a ratio of 10 participants per one item of the scale, which was exceeded in this subsample. Our intention was to test the MDDI model extracted from the EFA. Parameter estimates were obtained using the maximum likelihood method and fit indices. For this purpose, the normed model chi-square (χ2/df), the Steiger-Lind root mean square error of approximation (RMSEA), the Tucker-Lewis Index (TLI) and the comparative fit index (CFI). Values ≤ 3 for χ2/df, and ≤ 0.06 for RMSEA, and 0.90 for CFI and TLI indicate acceptable fit of the model to the data [67].
Measurement invariance by eating attitudes and weight status
To examine measurement invariance of the Ar-MDDI scores according to the eating attitudes, we conducted multi-group CFA [68] using the total sample. Measurement invariance was assessed at the configural, metric, and scalar levels [69]. Configural invariance implies that the latent MDD variable(s) and the pattern of loadings of the latent variable(s) on indicators are similar across eating attitudes and weight status (i.e., the unconstrained latent model should fit the data well in both groups). Metric invariance implies that the magnitude of the loadings is similar across eating attitudes and weight status; this is tested by comparing two nested models consisting of a baseline model and an invariance model. Lastly, scalar invariance implies that both the item loadings and item intercepts are similar across gender and is examined using the same nested-model comparison strategy as with metric invariance [68]. Following the recommendations of Cheung and Rensvold [70] and Chen [68], we accepted ΔCFI ≤ 0.010 and ΔRMSEA ≤ 0.015 or ΔSRMR ≤ 0.010 (0.030 for factorial invariance) as evidence of invariance. We aimed to test for eating attitudes and weight status differences on latent MDD scores using an independent-samples t-test only if scalar or partial scalar invariance were established.
Further analyses
Composite reliability in both subsamples was assessed using McDonald’s (1970) ω, with values greater than 0.70 reflecting adequate composite reliability [71]. McDonald’s ω was selected as a measure of composite reliability because of known problems with the use of Cronbach’s α (e.g., [72]). Finally, we examined the skewness and kurtosis values for the MDDI subscales scores, which were within defined range (skewness <|3|, kurtosis <|10|; [73]). Therefore, the sample was considered normally distributed. Consequently, Pearson correlation test was used to test the convergent and divergent validity of the Ar-MDDI scale with the other scores included in the study. Based on Cohen (1992) [74], values ≤ 0.10 were considered weak, ~ 0.30 were considered moderate, and ~ 0.50 were considered strong correlations. The latter analysis was done using SPSS software v.22.
Results
Exploratory factor analysis in the first split-half sample
Bartlett’s test of sphericity, χ2(78) = 813.7, p < 0.001, and KMO (0.786) indicated that the Ar-MDDI items had adequate common variance for factor analysis. The results of the EFA revealed three factors, which explained 57.68% of the common variance. The WRMR value was also adequate (= 0.079; 95% CI 0.065–0.087), indicating good fit of the model. McDonald’s ω was adequate for Factor 1 = Appearance intolerance (ω = 0.77), Factor 2 = Drive for size (ω = 0.71), and Factor 3 = Functional impairment (ω = 0.79).
Confirmatory factor analyses
The fit indices of the three-factor model of the Ar-MDDI scale showed good results as follows: The Maximum Likelihood Chi-Square = 123.80 and Degrees of Freedom = 62, which gave a χ2/df = 2.00, TLI = 0.90, CFI = 0.92 and RMSEA = 0.073 [90% CI 0.054–0.091]. The standardized loading factors of the MDDI scale are summarized in Table 1. McDonald’s ω values were adequate for Factor 1 = Appearance intolerance (ω = 0.78), Factor 2 = Drive for size (ω = 0.69), and Factor 3 = Functional impairment (ω = 0.83). The standardized loading factors ranged from 0.50 to 0.85.
Measurement invariance
254 (64.1%) of the participants had disordered eating attitudes (EAT scores ≥ 20). Indices (Table 2) suggested that configural and metric invariance were supported; but scalar invariance was not upheld. Thus, it is inappropriate to conduct further group comparisons. Moreover, 128 (32.4%) of the participants had abnormal BMI (BMI > 25). Indices suggested that configural, metric, and scalar invariance was supported according to the dichotomized BMI (Table 2). People with abnormal BMI scored higher in terms of appearance intolerance (11.82 ± 4.46 vs 10.44 ± 3.57; t(393) = 3.32; p = 0.001) and lower in terms of drive for size (7.23 ± 2.93 vs 7.87 ± 2.88; t(393) = 2.03; p = 0.044) than those with normal BMI. Finally, no significant difference was observed between the two groups in terms of functional impairment (8.56 ± 3.58 vs 8.19 ± 3.31; t(393) = 1.02; p = 0.310).
Confirmatory analysis of the Big Three Perfectionism (BTP) scale using the total sample
Before conducting the analysis divergent validity, we ran a CFA on the BTP using the total sample to make sure that its three-factor structure is conserved in the Arabic version of the scale. The fit indices were adequate as follows: χ2/df = 370.48/101 = 3.67, SRMR = 0.049, TLI = 0.91, CFI = 0.93 and RMSEA = 0.082 [90% CI 0.073–0.091]. McDonald’s ω values were adequate for Factor 1 = rigid perfectionism (ω = 0.91), Factor 2 = self-critical perfectionism (ω = 0.88), and Factor 3 = narcissistic perfectionism (ω = 0.84).
Divergent validity
Higher Ar-MDDI subscales scores were significantly associated with higher rigid, narcissistic perfectionism and self-critical perfectionism (except for drive for size). Older age was significantly associated with less drive for size. Finally, higher BMI was significantly associated with more functional impairment and lower drive for size (Table 3).
Discussion
We conducted this study with the aim of validating the MDDI in Arabic in order to make it available for the Arabic-speaking populations around the world. Overall, our findings revealed that the validation of the Ar-MDDI yielded excellent properties in terms of factor structure, reliability, as well as convergent and divergent validity. Therefore, we preliminarily recommend its use for the assessment of MDD among Arabic-speaking men, at least in the Lebanese context.
CFA allowed the replication of the original three-factor structure of the MDDI. This three-factors structure has been originally highlighted by Hildebrandt et al. [47] and found in multiple validation papers tackling different populations (such as Brazilian women [75], American transgender men [76] [54], cisgender populations across distinct cultural settings [48,49,50,51, 77,78,79,80,81] and cisgender sexual minority populations [82])) was confirmed in our sample. In terms of reliability, the Cronbach’s alpha value of the Ar-MDDI obtained in the present study (0.81) corroborates the results of previous validation studies (e.g., the Brazilian [75], the Italian [83], and the German [78] versions), enabling us to suggest that the present Arabic versions of the MDDI seems to offer a reliable measure of MDD.
Beyond factorial validity and reliability, our findings revealed that perfectionism scores correlated positively with MDDI, which suggests divergent validity and align with previous evidence [42, 84,85,86,87]. The relationship between perfectionism and MDD is rather well-established [42, 84]. Perfectionism has even been suggested as a potential factor implicated in the development and maintenance of MDD, making affected individuals struggle to achieve an ideal body shape [88, 89].
Our data also provided preliminary evidence for the convergent validity of the Ar–MDDI scale, as it showed a significant correlation with eating attitudes. Our results are in agreement with a previous research [47]. Indeed, it has been shown that the traditional masculinity model is associated with more disordered eating [90]. Body ideals spread by sociocultural agents (parents, peers and media) incline to be internalized by the individuals, which can cause body image disturbances, MDD and the adoption of harmful behaviors such as restrictive eating, compulsive exercise, and others [91]. Furthermore, dysfunctional eating patterns significantly contribute to the onset and persistence of MDD [37, 88, 92]. MDD shares clinical features with ED symptoms, because of the presence of the compulsive exercise and rigid diet characterizing both disorders. In this line, a previous study revealed that orthorexia nervosa emerged as predictors of MDD symptoms in the bodybuilders [93].
Limitations
Some limitations of the current work should be noted. First, since MDD could manifest among women (albeit with different features) [93,94,95], it is worthy to test the validity and reliability of the scale using women samples. Other validation studies are also required in specific groups, such as Arabic-speaking athletes and bodybuilders; given that this population is at a particularly heightened risk of MDD symptomatology and associated behaviors as compared to the non-bodybuilder population [42]. Second, the results of this study do not allow the generalizability of the results to other men from other age ranges. Third, the snowball technique and the unknown refusal rate predispose us to a selection bias. Fourth, other psychometric properties of the scales were not addressed in this paper (i.e. test–retest and convergent validity). Fifth, divergent validity was tested only using perfectionism measure.
Conclusion
Our psychometric examination confirms the robustness of the Ar-MDDI, supporting the idea that the MDDI subscales evaluate three distinct elements of the psychopathology and manifestations of the MD. Functional impairment, which is required for the DSM-5 diagnosis of muscle dysmorphia, is not evaluated by the other commonly used assessment tools, supporting the main role of MDDI in screening for clinically relevant symptoms. Overall, our study provides a useful tool to assess muscle dysmorphia among Arabic-speaking men. Our Arabic version of the scale adds to the multitude of translated versions of this scale, allowing for cross-cultural comparisons of muscle dysmorphia among men. This would allow future clinicians to evaluate whether it is a public health concern in order to create appropriate strategies to reduce it.
Availability of data and materials
All data generated or analyzed during this study are not publicly available due the restrictions from the ethics committee.
Abbreviations
- AR-MDDI:
-
The Arabic version of the Muscle Dysmorphic Disorder Inventory
- DSM-5:
-
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- CFA:
-
Confirmatory factor analysis
- EFA:
-
Exploratory factor analysis
- MDDI:
-
The Muscle Dysmorphic Disorder Inventory
- MDD:
-
Muscle dysmorphic disorder
References
Sharan P, Sundar AS. Eating disorders in women. Indian J Psychiatry. 2015;57(Suppl 2):S286–95. https://doi.org/10.4103/0019-5545.161493.
Murray SB, Nagata JM, Griffiths S, Calzo JP, Brown TA, Mitchison D, et al. The enigma of male eating disorders: a critical review and synthesis. Clin Psychol Rev. 2017;57:1–11. https://doi.org/10.1016/j.cpr.2017.08.001.
Mitchison D, Mond J. Epidemiology of eating disorders, eating disordered behaviour, and body image disturbance in males: a narrative review. J Eat Disord. 2015;3(1):1–9. https://doi.org/10.1186/s40337-015-0058-y.
Lavender JM, Brown TA, Murray SB. Men, muscles, and eating disorders: an overview of traditional and muscularity-oriented disordered eating. Curr Psychiatry Rep. 2017;19(6):1–7. https://doi.org/10.1007/s11920-017-0787-5.
Murray SB, Griffiths S, Lavender JM. Introduction to a special issue on eating disorders and related symptomatology in male populations. Int J Eat Disord. 2019;52(12):1339–42. https://doi.org/10.1002/eat.23184.
Mitchison D, Mond J. Epidemiology of eating disorders, eating disordered behaviour, and body image disturbance in males: a narrative review. J Eat Disord. 2015;3:20.
Bentley C, Gratwick-Sarll K, Harrison C, Mond J. Sex differences in psychosocial impairment associated with eating disorder features in adolescents: a school-based study. Int J Eat Disord. 2015;48(6):633–40.
Edwards C, Tod D, Molnar G. A systematic review of the drive for muscularity research area. Int Rev Sport Exerc Psychol. 2014;7(1):18–41.
Murray SB, Griffiths S, Mond JM. Evolving eating disorder psychopathology: conceptualising muscularity-oriented disordered eating. Br J Psychiatry J Mental Sci. 2016;208(5):414–5.
Murray SB, Brown TA, Blashill AJ, Compte EJ, Lavender JM, Mitchison D, et al. The development and validation of the muscularity-oriented eating test: a novel measure of muscularity-oriented disordered eating. Int J Eat Disord. 2019;52(12):1389–98. https://doi.org/10.1002/eat.23144.
Karazsia BT, Crowther JH. Social body comparison and internalization: mediators of social influences on men’s muscularity-oriented body dissatisfaction. Body Image. 2009;6(2):105–12.
Schneider C, Rollitz L, Voracek M, Hennig-Fast K. Biological, psychological, and sociocultural factors contributing to the drive for muscularity in weight-training men. Front Psychol. 2016;7:1992.
Abou-Saleh MT, Younis Y, Karim L. Anorexia nervosa in an Arab culture. Int J Eat Disord. 1998;23(2):207–12.
Pike KM, Hoek HW, Dunne PE. Cultural trends and eating disorders. Curr Opin Psychiatry. 2014;27(6):436–42. https://doi.org/10.1097/YCO.0000000000000100.
Fekih-Romdhane F, Daher-Nashif S, Alhuwailah AH, Al Gahtani HMS, Hubail SA, Shuwiekh HAM, et al. The prevalence of feeding and eating disorders symptomology in medical students: an updated systematic review, meta-analysis, and meta-regression. Eat Weight Disord. 2022. https://doi.org/10.1007/s40519-021-01351-w.
Podar I, Allik J. A cross-cultural comparison of the eating disorder inventory. Int J Eat Disord. 2009;42(4):346–55. https://doi.org/10.1002/eat.20616.
Zeeni N, Safieddine H, Doumit R. Eating disorders in Lebanon: directions for public health action. Community Ment Health J. 2017;53(1):117–25. https://doi.org/10.1007/s10597-015-9917-x.
Haddad C, Obeid S, Akel M, Honein K, Akiki M, Azar J, et al. Correlates of orthorexia nervosa among a representative sample of the Lebanese population. Eat Weight Disord. 2019;24(3):481–93. https://doi.org/10.1007/s40519-018-0631-x.
Saade S, Hallit S, Haddad C, Hallit R, Akel M, Honein K, et al. Factors associated with restrained eating and validation of the Arabic version of the restrained eating scale among an adult representative sample of the Lebanese population: a cross-sectional study. J Eat Disord. 2019;7(1):1–13. https://doi.org/10.1186/s40337-019-0254-2.
Haddad C, Khoury C, Salameh P, Sacre H, Hallit R, Kheir N, et al. Validation of the Arabic version of the Eating Attitude Test in Lebanon: a population study. Public Health Nutr. 2021;24(13):4132–43. https://doi.org/10.1017/S1368980020002955.
Al-Musharaf S, Rogoza R, Mhanna M, Soufia M, Obeid S, Hallit S. Factors of body dissatisfaction among lebanese adolescents: the indirect effect of self-esteem between mental health and body dissatisfaction. BMC Pediatr. 2022;22(1):302. https://doi.org/10.1186/s12887-022-03373-4.
Yahia N, El-Ghazale H, Achkar A, Rizk S. Dieting practices and body image perception among Lebanese university students. Asia Pac J Clin Nutr. 2011;20(1):21–8.
Hoteit M, Mohsen H, Bookari K, Moussa G, Jurdi N, Yazbeck N. Prevalence, correlates and gender disparities related to eating disordered behaviors among health science students and healthcare practitioners in Lebanon: findings of a national cross sectional study. Front Nutr 2022:1635.
Zakhour M, Haddad C, Sacre H, Tarabay C, Zeidan RK, Akel M, et al. Differences in the associations between body dissatisfaction and eating outcomes by gender? A Lebanese population study. Rev Epidemiol Sante Publique. 2021;69(3):134–44. https://doi.org/10.1016/j.respe.2021.02.003.
Afifi-Soweid RA, Najem Kteily MB, Shediac-Rizkallah MC. Preoccupation with weight and disordered eating behaviors of entering students at a university in Lebanon. Int J Eat Disord. 2002;32(1):52–7. https://doi.org/10.1002/eat.10037.
El Ayoubi LM, Abou Ltaif D, El Masri J, Salameh P. Effects of night eating and binge eating disorders on general health in university students in Lebanon. Irish J Med Sci 2022:1–6.
Fatima W, Fatima R, Anwar NS. Disordered eating attitude and body dissatisfaction among adolescents of Arab countries: a review. Asian J Biol Sci. 2019;12(3):373–9.
Boulos Nakhoul T, Mina A, Soufia M, Obeid S, Hallit S. Restrained eating in Lebanese adolescents: scale validation and correlates. BMC Pediatr. 2021;21(1):1–11.
Hallit S, Brytek-Matera A, Obeid S. Orthorexia nervosa and disordered eating attitudes among Lebanese adults: assessing psychometric proprieties of the ORTO-R in a population-based sample. PLoS ONE. 2021;16(8):e0254948. https://doi.org/10.1371/journal.pone.0254948.
Rogoza R, Mhanna M, Gerges S, Donini LM, Obeid S, Hallit S. Validation of the Arabic version of the ORTO-R among a sample of Lebanese young adults. Eat Weight Disord. 2022;27(6):2073–80. https://doi.org/10.1007/s40519-021-01350-x.
Rogoza R, Hallit S, Soufia M, Barthels F, Obeid S. Validation of the Arabic version of the Dusseldorf Orthorexia Scale (DOS) among Lebanese adolescents. J Eat Disord. 2021;9(1):130. https://doi.org/10.1186/s40337-021-00488-4.
Mhanna M, Azzi R, Hallit S, Obeid S, Soufia M, et al. Validation of the Arabic version of the Teruel Orthorexia Scale (TOS) among Lebanese adolescents. Eat Weight Disord. 2022;27(2):619–27. https://doi.org/10.1007/s40519-021-01200-w.
Fekih-Romdhane F, Obeid S, Malaeb D, Hallit R, Hallit S. Validation of a shortened version of the Eating Attitude Test (EAT-7) in the Arabic language. J Eat Disord. 2022;10(1):1–8. https://doi.org/10.1186/s40337-022-00651-5.
American Psychiatric Association A, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5: Washington, DC: American psychiatric association; 2013.
Pope HG Jr, Gruber AJ, Choi P, Olivardia R, Phillips KA. Muscle dysmorphia: an underrecognized form of body dysmorphic disorder. Psychosomatics. 1997;38(6):548–57.
Grieve FG, Truba N, Bowersox S. Etiology, assessment, and treatment of muscle dysmorphia. ProQuest. 2009;23(4):306–14.
Olivardia R. Mirror, mirror on the wall, who’s the largest of them all? The features and phenomenology of muscle dysmorphia. Harv Rev Psychiatry. 2001;9(5):254–9.
Olivardia R, Pope HG Jr, Hudson JI. Muscle dysmorphia in male weightlifters: a case-control study. Am J Psychiatry. 2000;157(8):1291–6. https://doi.org/10.1176/appi.ajp.157.8.1291.
Grieve FG, Truba N, Bowersox S. Etiology, assessment, and treatment of muscle dysmorphia. J Cogn Psychother. 2009;23(4):306–14.
Cafri G, Olivardia R, Thompson JK. Symptom characteristics and psychiatric comorbidity among males with muscle dysmorphia. Compr Psychiatry. 2008;49(4):374–9.
Pope CG, Pope HG, Menard W, Fay C, Olivardia R, Phillips KA. Clinical features of muscle dysmorphia among males with body dysmorphic disorder. Body Image. 2005;2(4):395–400. https://doi.org/10.1016/j.bodyim.2005.09.001.
Mitchell L, Murray SB, Cobley S, Hackett D, Gifford J, Capling L, et al. Muscle dysmorphia symptomatology and associated psychological features in bodybuilders and non-bodybuilder resistance trainers: a systematic review and meta-analysis. Sports Med. 2017;47(2):233–59. https://doi.org/10.1007/s40279-016-0564-3.
Lowes J, Tiggemann M. Body dissatisfaction, dieting awareness and the impact of parental influence in young children. Br J Health Psychol. 2003;8(2):135–47.
Cunningham ML, Griffiths S, Mitchison D, Mond JM, Castle D, Murray SB. Muscle dysmorphia: an overview of clinical features and treatment options. J Cogn Psychother. 2017;31(4):255–71. https://doi.org/10.1891/0889-8391.31.4.255.
Hitzeroth V, Wessels C, Zungu-Dirwayi N, Oosthuizen P, Stein DJ. Muscle dysmorphia: a South African sample. Psychiatry Clin Neurosci. 2001;55(5):521–3.
Griffiths S, Mond JM, Li Z, Gunatilake S, Murray SB, Sheffield J, et al. Self-stigma of seeking treatment and being male predict an increased likelihood of having an undiagnosed eating disorder. Int J Eat Disord. 2015;48(6):775–8. https://doi.org/10.1002/eat.22413.
Hildebrandt T, Langenbucher J, Schlundt DG. Muscularity concerns among men: Development of attitudinal and perceptual measures. Body Image. 2004;1(2):169–81. https://doi.org/10.1016/j.bodyim.2004.01.001.
Compte EJ, Nagata JM, Sepúlveda AR, Rivas A, Sbdar LS, Menga S, et al. Assessment and validation of a Spanish version of the Muscle Dysmorphia Disorder Inventory in Argentinian men who exercise: Inventario de Dismorfia Muscular. Body Image. 2019;31:24–34. https://doi.org/10.1016/j.bodyim.2019.08.002.
Gomes VMGM, Compte EJ, Almeida M, Campos PF, Queiroz ACC, Pereira LF, et al. Psychometric properties of the Muscle Dysmorphic Disorder Inventory among physically active Brazilian college men. Psychol Men Masculinities. 2020;21(4):622.
Devrim A, Bilgic PJCN, Science F. Validity and reliability study of Turkish version of “muscle dysmorphic disorder inventory” and. J Eat Disord. 2019;15(5):517–24.
He J, Murray S, Compte EJ, Song J, Nagata JM. The muscularity-oriented eating test, drive for muscularity scale, and muscle dysmorphic disorder inventory among Chinese men: Confirmatory factor analyses. Int J Environ Res Public Health. 2021;18(21):11690. https://doi.org/10.3390/ijerph182111690.
Melisse B, de Beurs E, van Furth EF. Eating disorders in the Arab world: a literature review. J Eat Disord. 2020;8(1):1–19. https://doi.org/10.1186/s40337-020-00336-x.
Compte EJ, Cattle CJ, Lavender JM, Brown TA, Murray SB, Capriotti MR, et al. Psychometric evaluation of the muscle dysmorphic disorder inventory (MDDI) among gender-expansive people. J Eat Disord. 2022;10(1):1–11.
Krebs G, Quinn R, Jassi A. Is perfectionism a risk factor for adolescent body dysmorphic symptoms? Evidence for a prospective association. J Obsessive Compuls Relat Disord. 2019;22:100445. https://doi.org/10.1016/j.jocrd.2019.100445.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–91.
Smith MM, Saklofske DH, Stoeber J, Sherry SBJ. The big three perfectionism scale: a new measure of perfectionism. SAGE J. 2016;34(7):670–87.
Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. 1982;12(4):871–8. https://doi.org/10.1017/s0033291700049163.
Swami V, Barron D. Translation and validation of body image instruments: challenges, good practice guidelines, and reporting recommendations for test adaptation. Body Image. 2019;31:204–20.
Lorenzo-Seva U, Ferrando PJ. FACTOR: a computer program to fit the exploratory factor analysis model. Behav Res Methods. 2006;38(1):88–91.
Worthington RL, Whittaker TA. Scale development research: a content analysis and recommendations for best practices. Couns Psychol. 2006;34(6):806–38.
Clark L, Watson D. Construct validity: basic issues in objective scale development. Psychol Meas. 1995;28:61–75.
Hair Jr JF, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 7th Ed. Upper Saddle River; Prentice Hall; 2009. p. 761.
Timmerman ME, Lorenzo-Seva U. Dimensionality assessment of ordered polytomous items with parallel analysis. Psychol Methods. 2011;16(2):209.
Yu CY, editor Evaluation of model fit indices for latent variable models with categorical and continuous outcomes. Paper presented at the annual conference of the American Educational Research Association, April 4, 2002, New Orleans; 2002. Scientific Research—An accadamic Publisher.
Tabachnick B, Fidell L. Using Multivariate Statistics. 7th ed. New York: Pearson Publishers; 2019.
Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5(2):159–68.
Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55.
Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model. 2007;14(3):464–504.
Vadenberg R, Lance C. A review and synthesis of the measurement in variance literature: suggestions, practices, and recommendations for organizational research. Organ Res Methods. 2000;3:4–70.
Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002;9(2):233–55.
Dunn TJ, Baguley T, Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. 2014;105(3):399–412.
McNeish D. Thanks coefficient alpha, we’ll take it from here. Psychol Methods. 2018;23(3):412.
Weston R, Gore PA Jr. A brief guide to structural equation modeling. SAGE J. 2006;34(5):719–51.
Cohen J, editor Quantitative methods in psychology: A power primer. Psychological bulletin; 1992: Citeseer.
Nagata JM, Junqueira ACP, Cattle CJ, de Carvalho PHB, Bagolin V, Murray SB, et al. Validation of the muscle dysmorphic disorder inventory (MDDI) in Brazilian women. Body Image. 2022;41:58–66. https://doi.org/10.1016/j.bodyim.2022.02.003.
Nagata JM, Compte EJ, McGuire FH, Lavender JM, Murray SB, Brown TA, et al. Psychometric validation of the Muscle Dysmorphic Disorder Inventory (MDDI) among US transgender men. Body Image. 2022;42:43–9. https://doi.org/10.1016/j.bodyim.2022.05.001.
Sepúlveda AR, Rica R, Moreno A, Román FJ, Compte EJ. Asessing the male body image: Spanish validation of two instruments. Psychiatry Res. 2019;272:483–90. https://doi.org/10.1016/j.psychres.2018.12.125.
Zeeck A, Welter V, Alatas H, Hildebrandt T, Lahmann C, Hartmann A. Muscle Dysmorphic Disorder Inventory (MDDI): Validation of a German version with a focus on gender. PLoS ONE. 2018;13(11):e0207535. https://doi.org/10.1371/journal.pone.0207535.
Compte EJ, Nagata JM, Sepulveda AR, Rivas A, Sbdar LS, Menga S, et al. Assessment and validation of a Spanish version of the Muscle Dysmorphia Disorder Inventory in Argentinian men who exercise: Inventario de Dismorfia Muscular. Body Image. 2019;31:24–34.
Sepulveda AR, Rica R, Moreno A, Roman FJ, Compte EJ. Asessing the male body image: Spanish validation of two instruments. Psychiatry Res. 2019;272:483–90.
Zeeck A, Welter V, Alatas H, Hildebrandt T, Lahmann C, Hartmann A. Muscle Dysmorphic Disorder Inventory (MDDI): validation of a German version with a focus on gender. PLoS ONE. 2018;13(11): e0207535.
Compte EJ, Cattle CJ, Lavender JM, Murray SB, Brown TA, Capriotti MR, et al. Psychometric evaluation of the Muscle Dysmorphic Disorder Inventory (MDDI) among cisgender gay men and cisgender lesbian women. Body Image. 2021;38:241–50. https://doi.org/10.1016/j.bodyim.2021.04.008.
Santarnecchi E, Dèttore D. Muscle dysmorphia in different degrees of bodybuilding activities: validation of the Italian version of Muscle Dysmorphia Disorder Inventory and Bodybuilder Image Grid. Body Image. 2012;9(3):396–403. https://doi.org/10.1016/j.bodyim.2012.03.006.
Wade TD, Tiggemann M. The role of perfectionism in body dissatisfaction. J Eat Disord. 2013;1(1):1–6. https://doi.org/10.1186/2050-2974-1-2.
Zarei S. Drive for muscularity in male adolescents: the role of psychological factors (Self-Esteem, Maladaptive Perfectionism, and Interpersonal Sensitivity). Iran J Psychiatry Behav Sci. 2020;14(2):e98393.
Bento C, Pereira A, Maia B, Marques M, Soares M, Bos S, et al. Perfectionism and eating behaviour in Portuguese adolescents. Eur Eat Disord Rev. 2010;18(4):328–37. https://doi.org/10.1002/erv.981.
Boone L, Braet C, Vandereycken W, Claes L. Are maladaptive schema domains and perfectionism related to body image concerns in eating disorder patients? Eur Eat Disord Rev. 2013;21(1):45–51. https://doi.org/10.1002/erv.2175.
Grieve FG. A conceptual model of factors contributing to the development of muscle dysmorphia. Eat Disord. 2007;15(1):63–80. https://doi.org/10.1080/10640260601044535.
Skemp KM, Mikat RP, Schenck KP, Kramer NA. Muscle dysmorphia: risk may be influenced by goals of the weightlifter. J Strength Cond Res. 2013;27(9):2427–32. https://doi.org/10.1519/JSC.0b013e3182825474.
Toro-Alfonso J, Urzúa MA, Cardona IS. El Cuerpo del Delito: La imagen corporal e indicadores de trastornos alimentarios en una muestra de hombres gay de diez países latinoamericanos. Rev Argent Clín Psicola, 2012.
de Carvalho PHB, dos Santos Alvarenga M, Ferreira MEC. An etiological model of disordered eating behaviors among Brazilian women. Appetite. 2017;116:164–72. https://doi.org/10.1016/j.appet.2017.04.037.
Cafri G, Thompson JK, Ricciardelli L, McCabe M, Smolak L, Yesalis C. Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clin Psychol Rev. 2005;25(2):215–39. https://doi.org/10.1016/j.cpr.2004.09.003.
Cerea S, Bottesi G, Pacelli QF, Paoli A, Ghisi M. Muscle dysmorphia and its associated psychological features in three groups of recreational athletes. Sci Rep. 2018;8(1):1–8. https://doi.org/10.1038/s41598-018-27176-9.
Hale BD, Diehl D, Weaver K, Briggs M. Exercise dependence and muscle dysmorphia in novice and experienced female bodybuilders. J Behav Addict. 2013;2(4):244–8. https://doi.org/10.1556/JBA.2.2013.4.8.
Tod D, Edwards C, Cranswick I. Muscle dysmorphia: current insights. Psychol Res Behav Manag. 2016;9:179. https://doi.org/10.2147/PRBM.S97404.
Acknowledgements
The authors would like to thank all participants.
Funding
None.
Author information
Authors and Affiliations
Contributions
SO and SH designed the study; FFR drafted the manuscript; GM and VM collected the data and helped with the writing; SH carried out the analysis and interpreted the results; RH, JH and RR reviewed the paper for intellectual content; all authors reviewed the final manuscript and gave their consent.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Psychiatric Hospital of the Cross Ethics and Research Committee approved this study protocol (HPC-028-2022). A written informed consent was considered obtained from each participant when submitting the online form. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Appendix 1.
Arabic items of the Muscle Dysmorphic Disorder Inventory.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fekih-Romdhane, F., Merhy, G., Moubarak, V. et al. Validation of the Arabic version of the Muscle Dysmorphic Disorder Inventory (Ar-MDDI) among Lebanese male university students. J Eat Disord 11, 11 (2023). https://doi.org/10.1186/s40337-023-00737-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40337-023-00737-8