Abstract
Background
Brucellosis is a severe zoonotic disease that is often overlooked, particularly in impoverished countries. Timely identification of focal complications in brucellosis is crucial for improving treatment outcomes. However, there is currently a lack of established indicators or biomarkers for diagnosing these complications. Therefore, this study aimed to investigate potential warning signs of focal complications in human brucellosis, with the goal of providing practical parameters for clinicians to aid in the diagnosis and management of patients.
Methods
A multi-center cross-sectional study was conducted in China from December 2019 to August 2021. The study aimed to investigate the clinical characteristics and complications of patients with brucellosis using a questionnaire survey and medical record system. The presence of warning signs for complications was assessed using univariate and multivariate logistic regression models. Receiver operating characteristic (ROC) curves and the area under the curve (AUC) were used for variable screening and model evaluation.
Results
A total of 880 participants diagnosed with human brucellosis were enrolled. The median age of the patients was 50 years [interquartile range (IQR): 41.5–58.0], and 54.8% had complications. The most common organ system affected by complications was the osteoarticular system (43.1%), with peripheral arthritis (30.0%), spondylitis (16.6%), paravertebral abscess (5.0%), and sacroiliitis (2.7%) being the most prevalent. Complications in other organ systems included the genitourinary system (4.7%), respiratory system (4.7%), and hematologic system (4.6%). Several factors were found to be associated with focal brucellosis. These factors included a long delay in diagnosis [odds ratio (OR) = 3.963, 95% confidence interval (CI) 1.906–8.238 for > 90 days], the presence of underlying disease (OR = 1.675, 95% CI 1.176–2.384), arthralgia (OR = 3.197, 95% CI 1.986–5.148), eye bulging pain (OR = 3.482, 95% CI 1.349–8.988), C-reactive protein (CRP) > 10 mg/L (OR = 1.910, 95% CI 1.310–2.784) and erythrocyte sedimentation rate (ESR) elevation (OR = 1.663, 95% CI 1.145–2.415). The optimal cutoff value in ROC analysis was > 5.4 mg/L for CRP (sensitivity 73.4% and specificity 51.9%) and > 25 mm/h for ESR (sensitivity 47.9% and specificity 71.1%).
Conclusions
More than 50% of patients with brucellosis experienced complications. Factors such as diagnostic delay, underlying disease, arthralgia, eye pain, and elevated levels of CRP and ESR were identified as significant markers for the development of complications. Therefore, patients presenting with these conditions should be closely monitored for potential complications, regardless of their culture results and standard tube agglutination test titers.
Similar content being viewed by others
Background
Brucellosis is a zoonotic disease that has significant negative impacts on both livestock productivity and human health worldwide, particularly in developing countries [1]. It is a disease of poverty [2], with an estimated 3.5 billion individuals at risk of contracting brucellosis globally [3]. In recent years, there has been a sharp increase in human brucellosis incidence, posing a significant public health threat in China [4]. Transmission primarily occurs through direct contact with infected animal fluids and secretions, consumption of unpasteurized or raw dairy products, or inhalation of infectious aerosols [5]. Brucellosis can affect various organs and systems, sometimes presenting with acute systemic symptoms, but may also manifest without such symptoms. Early and accurate diagnosis is crucial for effective management and treatment of brucellosis.
Brucellosis is caused by Gram-negative bacteria of the genus Brucella, which have the ability to establish long-term infections in their hosts [6, 7]. Brucella evades the host immune system’s clearance mechanisms, and the duration of infection within host cells depends on the host's immunity and the appropriate use of specific antibiotics. Therefore, early diagnosis and proper treatment are crucial in reducing the risk of chronicity and relapse. However, the clinical manifestations of brucellosis can vary greatly and mimic other diseases, leading to misdiagnosis and missed diagnosis [8]. Confirming brucellosis requires a combination of exposure history, clinical manifestations, and specific laboratory tests. Underdiagnosis of brucellosis leads to higher rates of complicated cases [9]. Focal involvement in brucellosis requires longer treatment duration and additional antimicrobial agents compared to uncomplicated cases [10]. Unfortunately, there are currently no specific biomarkers reported for diagnosing complications. It is challenging to distinguish complications based solely on general symptoms, signs, or single biomarkers [4]. Therefore, it is necessary to explore comprehensive diagnostic warning indicators for complicated brucellosis to aid clinicians in promptly diagnosing and treating the disease.
Understanding the true clinical spectrum of brucellosis and its complications is crucial for medical practitioners to make early decisions. Although a few studies have reported on the clinical spectrum of brucellosis complications and related factors [8, 11, 12], these studies had limitations such as being single center, having small sample sizes, and focusing only on inpatients, which will likely overestimate the reported complication rates, and latent indicators for identifying focal involvement in outpatients might have been missed. To address these limitations, we conducted a multi-center observational study to determine the real incidence and clinical spectrum of brucellosis complications in both inpatients and outpatients and to identify clinical and laboratory warning indicators for complications, which could improve the diagnostic criteria and enhance the management of patients. Furthermore, it is worth noting that the current version of the guideline on the diagnosis and therapy of brucellosis in China does not include diagnostic principles for complications [13]. Therefore, our study is valuable in standardizing the diagnosis and treatment of brucellosis complications, ultimately reducing the incidence of chronic brucellosis.
Methods
Study design and setting
A multi-center cross-sectional study was conducted in five cities in China, namely Bayannur City in Inner Mongolia Autonomous Region, Ili and Changji City in Xinjiang Uygur Autonomous Region, and Jinan and Dongying City in Shandong Province, from December 2019 to August 2021. These cities were selected based on their high incidence rates of brucellosis, being among the top 10% in their respective provincial-level administrative divisions (PLADs). All project sites were designated medical institutions for brucellosis treatment and had the necessary capacity to conduct the required examinations and laboratory tests. To maintain biosafety, Brucella blood cultures were performed at CDC laboratory, while other tests were carried out at the project sites. The laboratory test results were consistent across all project sites. The study protocol was approved by the Research Ethics Review Committee of the Chinese Center for Disease Control and Prevention (Approval number: 201942), and signed informed consent was obtained from all participants prior to the investigation.
Sample size
A cross-sectional study was conducted to estimate the sample size for assessing the prevalence of focal complications in human brucellosis. The “Confidence Intervals for One Proportion” module from Power Analysis and Sample Size Software (Version 15, NCSS LLC., East Kaysville, Utah, United States) was used to perform the sample size calculation. Based on a previous study reporting a range of brucellosis complication rates from 27.7–89.7% [11, 14], we chose a conservative estimate of 50% to ensure the maximum sample size. Considering confidence levels: 95% confidence intervals (CIs) formula was Exact (Clopper-pearson), the width of the CIs (two sided) was 10%, the dropout rate was 20%, the minimum sample size was 503 individuals. Ultimately, a total of 880 brucellosis patients were included in the study.
Sampling and participants
A multi-stage random sampling method was utilized to select specific hospitals and patients with human brucellosis. In regions of Inner Mongolia, Xinjiang, and Shandong with high incidence rates, five county-level designated medical institutions were chosen. From December 2019 to August 2021, doctors from these designated medical institutions enrolled eligible brucellosis patients who met the criteria, following the principle of informed consent. Enrollment continued until the desired sample size was achieved.
The inclusion criteria for cases were as follows: (1) patients diagnosed with brucellosis; (2) aged 15 years and above; (3) provided informed consent and willingly participated in the study.
The criteria for case exclusion were: (1) infected with the human immunodeficiency virus (HIV), undergoing chemotherapy, having other immune system disorders, or suffering from other severe illnesses; (2) suffering from mental disorders, deafness and other disorders resulting in poor communication and inability to cooperate with the investigation; (3) pregnant woman.
The definition of confirmed cases of brucellosis includes patients who have both a history of exposure and clinical symptoms, and meet one of the following criteria: (1) Isolation and culture of Brucella bacteria from the patient's blood or other specimens; (2) A serum agglutination test (SAT) titer of ≥ 1:100 (++) or a duration of illness of over one year with a titer of ≥ 1:50 (++); (3) A Coombs test titer of ≥ 1:400 (++).
Data collection and definitions
After obtaining informed consent, each patient diagnosed with brucellosis was interviewed by a qualified physician using a standardized questionnaire. The purpose of the questionnaire was to gather the following information: gender, age, nationality, occupation, region of residence, level of education, exposure to animals (specifically sheep & goats, cattle, etc.), methods of animal exposure (such as raising, grazing, slaughter, delivering lambs, etc.), consumption of unpasteurized food, family history of brucellosis, and number of days since symptoms onset. Additionally, relevant variables from the Hospital Information System were extracted, such as date of diagnosis, presence of underlying diseases, previous history of brucellosis, symptoms and signs experienced (such as fever, chills, fatigue, etc.), complications, and laboratory test results.
A standardized protocol was implemented to ensure consistency in interviewer training and quality control supervision throughout all survey instances. Cases were included based on specific inclusion and exclusion criteria. Face-to-face interviews were conducted with all eligible cases by physicians who received professional training. Each questionnaire underwent thorough review by qualified supervisory staff. Data management specialists checked the collected questionnaires for completeness and logical consistency. The laboratory tests were carried out by properly trained laboratory technicians following national standardized methods and procedures.
The clinical stages of brucellosis were classified as follows: the acute stage, which lasted less than 3 months from the onset of symptoms to admission; the subacute stage, which lasted from 3 to 6 months; and the chronic stage, which lasted longer than 6 months. Age was calculated by determining the time period between the date of study participation and the date of birth for each brucellosis case. Fever was defined as axillary temperature of > 37.3 °C. Anemia: hemoglobin (Hb) female and children < 110 g/L, male < 120 g/L. Leukopenia: white blood cells (WBC) < 4 × 109 /L; Leukocytosis: WBC > 10 × 109 /L; Thrombocytopenia: platelet < 100 × 109 /L. ESR elevation: female > 20 mm/h and male > 15 mm/h.
In this study, we defined “focal complication” as a patient with symptoms of brucellosis who has at least one affected organ and tests positive for brucellosis through serology or culture. We defined “osteoarticular involvement” as the presence of inflammatory signs (swelling, pain, functional disability, heat, or redness) in any peripheral osteoarticular location, along with radiographic evidence of abnormalities. Peripheral arthritis was diagnosed based on clinical findings of joint swelling, effusion, and limited motion, as well as X-ray imaging. Sacroiliitis, spondylitis, and paravertebral abscesses were diagnosed based on clinical findings, as well as bone scans or magnetic resonance imaging (MRI). Neurological complications were confirmed in cases where the patient had a positive Brucella culture and/or positive blood or spinal Brucella culture with abnormal cerebrospinal fluid, as well as symptoms and signs of encephalitis or meningitis, while excluding other neurological diseases. Cardiovascular complications were identified by the presence of signs and symptoms such as heart murmur, retrosternal pain, and abnormalities in electrocardiogram (ECG) or ultrasonic cardiogram (UCG), after ruling out other causes and/or with positive Brucella culture in cases of pericardial effusion. Hematological complications were diagnosed based on abnormal clinical manifestations (anemia or bleeding) and abnormal laboratory findings, while excluding other causes. Genitourinary complications such as Orchitis, epididymitis, and pelvic inflammation were diagnosed based on signs and symptoms of urogenital system inflammation (orchialgia, testicular enlargement, and lower back pain in men; lower abdominal pain in women), confirmed by ultrasound. Respiratory system complications presented as bronchitis, pneumonia, or pleural effusion, and could be confirmed through chest X-rays, computed tomography (CT) scans, or MRI scans once other possible causes were ruled out. Cutaneous complications were defined as clinical manifestations of skin rash, purpura, ecchymosis, erythema nodosum, ulceration, or abscess in confirmed cases of brucellosis, while excluding other causes.
Statistical analysis
Data storage was done using EpiData version 3.1 (EpiData Association, Odense, Denmark). The normality assumption for quantitative variables was assessed using the Kolmogorov–Smirnov (KS) test with Lilliefors correction for significance. Non-normally distributed variables were described using median and inter-quartile ranges (IQRs). Categorical variables were described using frequency and percentage. Differences in proportions were tested using Pearson’s χ2 test or Fisher’s exact test. Logistic regression models were used to investigate the association between brucellosis complications and demographic, clinical, and laboratory characteristics. Univariate logistic regression was used to screen variables, considering P < 0.1 as statistically significant. Correlation analyses were performed using Spearman’s or Pearson’s correlation, and variables with strong correlations were removed. Factors selected from the screening were included in a multivariate analysis using a backward stepwise procedure. Multiple categorical variables were included in the model as dummy variables. Odds ratio (OR) and 95% CIs were calculated for categorical variables using a two-tailed test. Model evaluation and refinement were conducted using covariance checking, overdispersion correction, and other methods. Receiver operating characteristic (ROC) curves were generated to determine optimal cutoff values for diagnosing complicated brucellosis. Sensitivity and specificity were computed for each parameter in distinguishing complicated from uncomplicated brucellosis, and the area under the curve (AUC) was calculated. Data analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, USA). All tests were two-sided with significance set at P ≤ 0.05.
Results
In our study, we enrolled a total of 880 participants diagnosed with human brucellosis. The study period spanned from December 2019 to August 2021. Among the participants, 482 individuals (54.8%) presented with complicated brucellosis. Complications were observed in seven different anatomical systems, with osteoarthritis being the most prevalent focal complication. Please refer to Table 1 for further details.
Demographic and epidemiological characteristics
Demographic and epidemiological characteristics, stratified by complicated, are displayed in Table 2. A total of 642 (80.0%) patients were male. The median age was 50 years (IQR: 42–58, ranged from 16 to 73 years) and about four-fifths were aged from 31 to 60 years. The proportion of complications is higher in the age group over 60 years, P = 0.009. Of 880 cases, 85.7% were farmers or herders, 94.3% had a history of animal exposure and 14.8% ingested unpasteurized foods. The subjects mainly presented with the acute stage, followed by subacute stage and chronic stage, accounting for 90.1%, 5.7% and 4.2%, respectively. Complications occurred more frequently in subacute group (P = 0.002). The proportion of complications is higher in the underlying disease group (P < 0.001). The median number of days from illness onset to definitive diagnosis was 22 days (IQR: 11–53) in complicated cases, and 15 days (IQR: 8–30) in uncomplicated cases (P < 0.001). There were no significant differences in the proportion of complications found among groups based on nationality, occupation, region, education, family history of brucellosis, or previous history of brucellosis (P > 0.05).
Clinical presentation and laboratory findings
The most prevalent symptoms among all patients were arthralgia (83.2%), fatigue (71.1%), fever (53.0%), sweating (49.8%), and inappetence (36.6%). The most commonly affected joints were the knee (37.3%), spine (34.5%), shoulder (21.9%), sacral (19.4%), and iliac (19.0%). Furthermore, elevated CRP levels (> 10 mg/L) were observed in 48.9% of patients, while elevated ESR was seen in 54.3% of patients.
The symptoms and signs observed in patients with focal brucellosis were similar to those without focal complications, except for a higher occurrence of arthralgia, inappetence, nausea, orchialgia, and eye bulging pain (P < 0.05). Patients with focal brucellosis were more likely to present with arthritis in large joints such as sacral, iliac, shoulder, and spine (P < 0.05). Fatigue was more common in patients without focal brucellosis (67.2% vs 75.9%, P < 0.05). The levels of ESR and CRP were higher in patients with complicated brucellosis compared to those with uncomplicated brucellosis (P < 0.001). Moreover, the rate of Brucella culture positivity was higher in patients with uncomplicated brucellosis compared to those with complicated brucellosis (6.9% vs 14.1%, P < 0.001). Please refer to Table 3 for additional information.
Warning signs associated with complications
The univariate logistic regression analysis revealed that several factors were significantly associated with focal brucellosis, including age, nationality, time from onset to diagnosis, presence of underlying disease, fatigue, arthralgia, inappetence, nausea, orchialgia, eye bulging pain, anemia, CRP > 10 mg/L, ESR elevation, positive culture, and SAT ≥ 400.
We conducted multivariate logistic regression analysis to identify independent factors associated with complications. Our findings indicate that several factors were independently associated with focal brucellosis, including the number of days from onset to diagnosis, underlying disease, symptoms such as arthralgia and myalgia, eye bulging pain, CRP > 10 mg/L, ESR elevation, positive culture, and SAT ≥ 400 (Table 4). The model demonstrated good prediction performance with an AUC of 0.732, as shown in Fig. 1.
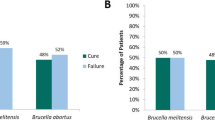
ROC curve analysis of clinical biomarkers in patients with and without complications
The AUC values for RBC, Hb, PLT, creatinine, CRP, and ESR as indicators of complicated cases were 0.576 (95% CI 0.542–0.610, P < 0.001), 0.546 (95% CI 0.512–0.580, P = 0.019), 0.546 (95% CI 0.512–0.580, P = 0.019), 0.567 (95% CI 0.533–0.600, P = 0.001), 0.634 (95% CI 0.598–0.668, P < 0.001), and 0.607 (95% CI 0.571–0.642, P < 0.001) (Additional file 1: Table S1). The optimal cutoff value determined by the ROC analysis was > 5.4 mg/L for CRP (sensitivity 73.4% and specificity 51.9%) and > 25 mm/h for ESR (sensitivity 47.9% and specificity 71.1%) (Fig. 2).
Discussion
Our study aimed to compare the demographic, clinical, and laboratory characteristics of brucellosis patients with or without complications to provide practical reference indices for clinicians in early diagnosis and patient management. More than half of the brucellosis patients experienced complications. Several factors were identified as warning signs for complications, including delayed diagnosis, underlying diseases, arthralgia, myalgia, eye bulging pain, CRP levels greater than 10 mg/L, and elevated ESR levels.
Large-scale epidemiological studies have reported complication rates ranging from 27.7 to 90% [11, 14]. The main affected anatomical sites were the osteoarticular, hematologic, and genitourinary systems, with incidence ranging from 2 to 77%, 2% to 53%, and 2% to 20%, respectively [15]. In this study, complications were observed in 54.8% of brucellosis cases, with osteoarticular involvement being the most common, consistent with previous studies. Therefore, brucellosis should be considered in the differential diagnosis of osteoarthropathy, orchitis, and other physiotherapy-related diseases in the rehabilitation department, especially in endemic regions. The spectrum of clinical symptoms and the distribution of focal involvement were found to be different from previous studies [16,17,18]. In our study, the complicated group showed a significantly higher incidence of arthralgia, inappetence, nausea, orchialgia, and eye bulging pain, while fatigue was significantly less frequent compared to the uncomplicated group. These differences may be attributed to variations in the definition of complications, diagnostic methods and instruments, epidemiological research methods, and the characteristics of the study subjects. For instance, a large epidemiological study conducted in China among inpatients at a high-level hospital reported a high incidence of complications at 90%, with 26% classified as subacute or chronic type [11]. The subjects of our research may be considered representative of brucellosis patients in China due to the proper study design, thus providing a comprehensive profile of the clinical spectrum of complicated brucellosis in the country.
In our study, we found that arthralgia, loss of myalgia, and eye bulging pain were statistically significant indicators of complications in patients. Specifically, osteoarticular complications were more commonly seen in large joints, such as the spine. Our results align with previous studies, which also identified arthralgia, absence of myalgias, and low back pain as associated factors for complications [16, 19,20,21]. Notably, eye bulging pain, although not common in brucellosis patients, should be carefully considered during diagnosis and treatment.
Several previous studies have shown that delayed diagnosis of brucellosis can lead to an increased rate of complications [19, 22, 23]. The longer brucellosis symptoms persist, the higher the risk of complications, likely due to the prolonged presence of the bacteria in the body. Therefore, early diagnosis is crucial in order to prevent complications and achieve better clinical outcomes. However, delayed diagnosis is a common occurrence, with medical practitioners citing the various atypical clinical manifestations of brucellosis and its resemblance to other diseases as major factors [24]. Additionally, prompt and accurate identification of complications is important, as extended treatment and the use of additional antibiotics are necessary for complete eradication of Brucella in patients with focal brucellosis [10]. Inadequate and inappropriate treatment can easily lead to chronicity [25], resulting in significant harm to patients and imposing a heavy economic burden on both their families and society as a whole. Therefore, it is essential to explore the use of biomarkers as comprehensive diagnostic indicators for complicated brucellosis.
This study identified CRP and ESR as indicators of focal involvement in brucellosis, with a cutoff value of 5.4 mg/L for CRP and 25 mm/h for ESR. Consistent with these findings, other studies have also reported higher levels of CRP and ESR in patients with complications [19]. Betul et al. [21] discovered that an ESR > 30 mm/h was a predictive factor for brucellosis complications. Additionally, Colmenero et al. [22] found that the risk of organ involvement was roughly doubled in cases of brucellosis diagnosed 30 days later with an ESR > 40 mm/h. Furthermore, the titer levels of IgG, IgM, and the neutrophil–lymphocyte ratio in the serum have been associated with complications [12, 26, 27].
The utility of blood culture for early identification of complications in brucellosis remains controversial, with limited and conflicting evidence available. Xu et al. [12] found that positive blood cultures were indicative of complicated brucellosis, while Bircan et al. [19] reported that negative blood cultures were statistically significant factors for complications. In other studies [20,21,22], the rates of blood culture and SAT positivity were similar in groups with and without focal involvement. The accuracy of blood culture results was greatly influenced by the conditions and techniques used [8]. In our study, we observed that negative blood cultures and low SAT titers were associated with brucellosis complications, suggesting the need for further in-depth research on this topic.
This study has several limitations. First, we selected provinces with a high number of brucellosis cases as study sites, which limited our ability to explore the association between Brucella strain type and brucellosis complications. Second, due to financial constraints, we were unable to include certain biomarkers related to immunity, such as CD4+ T lymphocyte, CD8+ T lymphocyte, IL2, and IL6. Third, using conventional indicators like inflammatory markers may not be appropriate as they can be influenced by autoimmune conditions and immunodeficiency diseases. Furthermore, future research should incorporate metabolomics, proteomics, and immunomics to detect biomarkers of brucellosis complications in serum and interstitial fluid. Such expansion of research is warranted in the future.
Conclusions
Complications are a frequent occurrence in patients with brucellosis. It is important to closely monitor patients with delayed diagnosis, underlying diseases, significant joint pain, eye bulging pain, and elevated levels of CRP or ESR during their initial visit. Additionally, early treatment should be administered with vigilance to prevent the onset of complications.
Availability of data and materials
The datasets produced and/or analyzed in this study can be obtained from the corresponding author upon request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the curve
- CI:
-
Confidence intervals
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ECG:
-
Electrocardiogram
- ESR:
-
Erythrocyte sedimentation rate
- Hb:
-
Hemoglobin
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- OR :
-
Odds ratio
- PLT:
-
Platelets
- RBC:
-
Red blood cells
- ROC:
-
Receiver operating characteristic
- SAT:
-
Standard tube agglutination test
- UCG:
-
Ultrasound cardiogram
- WBC:
-
White blood cells
References
Pappas G, Papadimitriou P, Akritidis N, Christou L, Tsianos EV. The new global map of human brucellosis. Lancet Infect Dis. 2006;6:91–9.
O’Callaghan D. Human brucellosis: recent advances and future challenges. Infect Dis Poverty. 2020;9:101.
Rossetti CA, Arenas-Gamboa AM, Maurizio E. Caprine brucellosis: a historically neglected disease with significant impact on public health. PLoS Negl Trop Dis. 2017;11: e0005692.
Zheng R, Xie S, Lu X, Sun L, Zhou Y, Zhang Y, Wang K. A systematic review and meta-analysis of epidemiology and clinical manifestations of human brucellosis in China. Biomed Res Int. 2018;2018:5712920.
Franco MP, Mulder M, Gilman RH, Smits HL. Human brucellosis. Lancet Infect Dis. 2007;7:775–86.
Jiao H, Zhou Z, Li B, Xiao Y, Li M, Zeng H, Guo X, Gu G. The mechanism of facultative intracellular parasitism of Brucella. Int J Mol Sci. 2021;22:3673.
Byndloss MX, Tsolis RM. Brucella spp. virulence factors and immunity. Annu Rev Anim Biosci. 2016;4:111–27.
Yagupsky P, Morata P, Colmenero JD. Laboratory diagnosis of human brucellosis. Clin Microbiol Rev. 2019;33:10–1128.
Mohammadbeigi A, Saghafipour A, Hamta A, Khazaei S, Maghsoudi A, Shams S. Epidemiological features of brucellosis and factors affecting its treatment failure and relapse in Qom Province, Iran. Ghana Med J. 2021;55:206–12.
Bosilkovski M, Keramat F, Arapovic J. The current therapeutical strategies in human brucellosis. Infection. 2021;49:823–32.
Shi Y, Gao H, Pappas G, Chen Q, Li M, Xu J, Lai S, Liao Q, Yang W, Yi Z, et al. Clinical features of 2041 human brucellosis cases in China. PLoS ONE. 2018;13: e0205500.
Xu N, Dong X, Yao Y, Guan Y, Chen F, Zheng F, Wang G. Improved early detection of focal brucellosis complications with anti-Brucella IgG. J Clin Microbiol. 2020;58:10–1128.
Ministry of Health of the People’s Republic of China. Brucellosis Diagnosis and Treatment Guidelines (Trial). Infect Dis Inf. 2012; 25(6):323–324, 359. (in Chinese).
Buzgan T, Karahocagil MK, Irmak H, Baran AI, Karsen H, Evirgen O, Akdeniz H. Clinical manifestations and complications in 1028 cases of brucellosis: a retrospective evaluation and review of the literature. Int J Infect Dis. 2010;14:e469-478.
Jin M, Fan Z, Gao R, Li X, Gao Z, Wang Z. Research progress on complications of Brucellosis. Front Cell Infect Microbiol. 2023;13:1136674.
Zhang Z, Zhang X, Chen X, Cui X, Cai M, Yang L, Zhang Y. Clinical features of human brucellosis and risk factors for focal complications: a retrospective analysis in a tertiary-care hospital in Beijing. China Int J Gen Med. 2022;15:7373–82.
Jiang W, Chen J, Li Q, Jiang L, Huang Y, Lan Y, Li Y. Epidemiological characteristics, clinical manifestations and laboratory findings in 850 patients with brucellosis in Heilongjiang Province, China. BMC Infect Dis. 2019;19:439.
Jia B, Zhang F, Lu Y, Zhang W, Li J, Zhang Y, Ding J. The clinical features of 590 patients with brucellosis in Xinjiang, China with the emphasis on the treatment of complications. PLoS Negl Trop Dis. 2017;11: e0005577.
Kayaaslan B, Bastug A, Aydin E, Akinci E, But A, Aslaner H, Yetkin MA, Bodur H. A long-term survey of brucellosis: Is there any marker to predict the complicated cases? Infect Dis (Lond). 2016;48:215–21.
Demirdal T, Sen P. Risk factors for focal involvement in brucellosis. Diagn Microbiol Infect Dis. 2020;97: 115003.
Copur B, Sayili U. Laboratory and clinical predictors of focal involvement and bacteremia in brucellosis. Eur J Clin Microbiol Infect Dis. 2022;41:793–801.
Colmenero JD, Reguera JM, Martos F, Sanchez-De-Mora D, Delgado M, Causse M, Martin-Farfan A, Juarez C. Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine (Baltimore). 1996;75:195–211.
Eales KM, Norton RE, Ketheesan N. Brucellosis in northern Australia. Am J Trop Med Hyg. 2010;83:876–8.
Wang Y, Zhang W, Ke Y, Zhen Q, Yuan X, Zou W, Li S, Sun Y, Wang Z, Wang D, et al. Human brucellosis, a heterogeneously distributed, delayed, and misdiagnosed disease in china. Clin Infect Dis. 2013;56:750–1.
Yousefi-Nooraie R, Mortaz-Hejri S, Mehrani M, Sadeghipour P. Antibiotics for treating human brucellosis. Cochrane Database Syst Rev. 2012;10:CD007179.
Sen P, Demirdal T, Nemli SA. Predictive value of inflammation markers in brucellosis. Arch Iran Med. 2019;22:640–5.
Balin SO, Tartar AS, Akbulut A. The predictive role of haematological parameters in the diagnosis of osteoarticular brucellosis. Afr Health Sci. 2018;18:988–94.
Acknowledgements
We sincerely thank all the subjects, their families, collaborating clinicians, CDC staff, and nurses for their participation and contribution to the study. We thank the provincial CDC of Shandong, Xinjiang and Inner Mongolia for their assistance in biological sample testing. Thanks to the China CDC for their support in the research process.
Funding
The study received support from the Public Health Emergency Response Mechanism Operation Program (102393220020010000017).
Author information
Authors and Affiliations
Contributions
QNS was responsible for implementation of this study, data analysis, and writing for original draft. HJQ and QSL performed the field work. SL and ZFT searched literature and polished English. MGF, MHA, ZQK provided technical guidance. QLC conceived and designed the study. QLC, WWY and YPZ reviewed and revised the paper. QLC and WWY were the corresponding author. All authors read and approved the final version of the paper.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol received approval from the Research Ethics Review Committee of the Chinese Center for Disease Control and Prevention (Approval number: 201942). Prior to the investigation, all participants provided signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors state that they do not have any conflicts of interest.
Supplementary Information
Additional file 1
: Table S1. ROC analyses for various cutoff values of laboratory parameters in predicting complications associated with human brucellosis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, QN., Qin, HJ., Lu, QS. et al. Incidence and warning signs for complications of human brucellosis: a multi-center observational study from China. Infect Dis Poverty 13, 18 (2024). https://doi.org/10.1186/s40249-024-01186-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-024-01186-4