Abstract
Parkinson’s disease (PD) is a progressive neurodegenerative disorder characterized by motor and non-motor symptoms. More than 200 years after its first clinical description, PD remains a serious affliction that affects a growing proportion of the population. Prevailing treatments only alleviate symptoms; there is still neither a cure that targets the neurodegenerative processes nor therapies that modify the course of the disease. Over the past decades, several animal models have been developed to study PD. Although no model precisely recapitulates the pathology, they still provide valuable information that contributes to our understanding of the disease and the limitations of our treatment options. This review comprehensively summarizes the different animal models available for Parkinson’s research, with a focus on those induced by drugs, neurotoxins, pesticides, genetic alterations, α-synuclein inoculation, and viral vector injections. We highlight their characteristics and ability to reproduce PD-like phenotypes. It is essential to realize that the strengths and weaknesses of each model and the induction technique at our disposal are determined by the research question being asked. Our review, therefore, seeks to better aid researchers by ensuring a concrete discernment of classical and novel animal models in PD research.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is the second most common age-related neurodegenerative disease, affecting up to 3% of individuals aged 65 and older [1, 2]. The disease is a progressive, multifactorial, and heterogeneous disorder. PD patients show motor dysfunction, such as resting tremors, rigidity, and bradykinesia [3, 4]. These cardinal symptoms are caused by the degeneration of dopamine (DA) neurons in the substantia nigra pars compacta (SNpc). PD is also accompanied by non-motor symptoms, including sleep disorders and dysfunction, autonomic dysfunction, cognitive and neuropsychiatric symptoms, gastrointestinal symptoms, weight and visual disturbances, and fatigue [2]. The pathology arises alongside the accumulation of Lewy bodies composed of aggregated α-synuclein (α-syn). The cause of DA neuronal loss remains unclear, but several pieces of evidence link these neuropathologic processes to impaired proteasomal protein clearance, mitochondrial dysfunction, and neuroinflammation [5, 6] (Fig. 1). Despite being well-characterized, the diagnosis of PD is only confirmed with a post-mortem autopsy, and what triggers this disease is still not clearly understood.
The hallmarks of Parkinson’s disease (PD). Predominant PD motor symptoms arise from DA neuron loss in the SNpc, and the denervation of their axons in the caudate nucleus and putamen, also called the striatum. The cause of PD remains unclear but involves loss of DA neurons, α-syn aggregation, mitochondrial dysfunction, autophagy impairments, and neuroinflammation. PD patients additionally exhibit non-motor symptoms. The figure was generated using BioRender.
Animal models have only been able to reproduce partial signs of the PD pathology. Compared to the clinical characteristics seen in patients, the onset, progression, and disease outcome in these models remain incomplete. Nevertheless, these animal models are still necessary to study the complexity of the brain networks involved in brain pathologies or to evaluate the impact of potential therapeutic approaches. The choice of the animal model is crucial, and studies must be interpreted with the inherent limitations of the paradigm chosen. In this review, we encompass a wide range of animal species, including rodents, non-human primates, and non-mammalian organisms such as Drosophila and C. elegans. Our aim is to provide an updated and comprehensive overview of both conventional and unconventional animal models of PD, including models that have received comparatively less attention. Moreover, our review goes beyond the primary pathogenic hallmarks of PD and sheds light on the secondary traits observed in each model, such as mitochondrial and autophagic dysfunctions, as well as neuroinflammation. By offering researchers a valuable resource, our review aims to assist them in selecting the most relevant animal model that aligns with their specific scientific questions.
Drug-induced parkinsonism
Drug-induced parkinsonism (DIP) is the most common form of secondary parkinsonism, meaning that in patients, DIP produces symptoms similar to those of PD. Typical symptoms in DIP include olfactory dysfunction, difficulty starting and controlling movement, loss or weakness of movement, and resting tremors [7]. DIP is the second most common cause of parkinsonism after idiopathic PD [8, 9]. In the following subsections, we will summarize existing drug-induced models, which reproduce several motor impairments in animals but fail to replicate the majority of neuropathologies associated with PD.
Reserpine
One of the first animal models of PD was generated with the injection of reserpine in 1957 by Carlsson and colleagues [10]. This molecule is an inhibitor of the vesicular monoamine transporter (VMAT) type 2 (Fig. 2) [11]. Reserpine administration causes monoamine depletion in nerve terminals by reducing vesicular storage and release. This loss of monoamines leads to hypolocomotion and muscular rigidity. Firstly used as an antihypertensive drug due to its capacity to deplete cellular monoamine content [12], the clinical application of reserpine resulted in patients developing lethargy, depression, and motor dyskinesia [12,13,14]. In rodents, administration of reserpine induces motor impairment as well as memory, cognitive, and emotional deficits [15, 16]. Injection of reserpine partially mimics the pathogenesis of PD, developing akinesia and rigidity that reflect the clinical features of the disease. Furthermore, the work of Carlsson and colleagues showed that Levodopa (L-DOPA) can partially rescue the effect of reserpine administration [10]. In rats, reserpine administration produces sexually dimorphic impairments in motor performance, as present in PD [17]. Within weeks, DA neuronal loss in the SNpc and fibers in the dorsal striatum can be seen. However, this phenotype is transient. A partial recovery of nigral DA neurons occurs 30 days post-injection, rescuing motor deficits [16,17,18]. It should be noted that no significant loss of DA axonal innervation in the dorsal striatum is observed in female rats, which could explain the dimorphic impairments in motor behavior [17]. Overall, reserpine can induce PD symptoms in humans and parkinsonian-like signs in rodents (Table 1). The facility for adjusting dose concentration and administration allows multiple levels of studies of PD symptomatology. Nevertheless, the reserpine model is not commonly used to study late-stage hallmarks of PD pathology, because it fails to generate Lewy body-like inclusions [19] and permanent loss of DA neurons. While there are reports of oxidative stress in the striatum of rodents upon treatment with reserpine, there is neither indication of mitochondrial or lysosomal dysfunction, nor inflammation [20]. However, other than memory deficits, reserpine also generates several non-motor features relevant to the preclinical manifestations of PD, i.e., sleep abnormalities, anxiety, depressive-like behavior, and gastrointestinal dysfunction [21]. For this reason, reserpine can be used as a model to study the disease progression and neurochemical features of PD.
Schematic summary of the current known mechanisms that trigger DA neuron death, and the action of different genes and compounds used to model PD. The loss of DA neurons could result from impaired protein degradation, mitochondrial dysfunction, α-syn aggregation, and neuroinflammation, which can be induced by neurotoxic or genetic alteration. The reduced DA signaling through drug inhibition could also lead to a PD-like phenotype. LPS: lipopolysaccharide, DAT: dopamine transporter, VMAT: vesicular monoamine transporter, NM: neuromelanin, DA: dopamine. The figure was generated using BioRender.
Haloperidol
Haloperidol is a typical antipsychotic that binds post-synaptic dopaminergic D2 receptors [22] (Fig. 2). The block of striatal DA transmission results in abnormal downstream firing within the basal ganglia circuits, manifesting muscle rigidity and catalepsy [23, 24]. Acute administration of haloperidol also reduces the striatal content of DA, noradrenaline, and serotonin [25]. A prolonged administration in mice causes mitochondrial complex I (MCI) deficiency in the frontal cortex, hippocampus, striatum, and midbrain [26]. The haloperidol model is used for modelling rigidity, dyskinesia or catalepsy, and for discovering novel antiparkinsonian agents in rodents [27,28,29,30] and non-human primates [31,32,33,34]. Additionally, chronic treatment of rodents with haloperidol results in significant increases in the levels of pro-inflammatory cytokines TNF-α and IL-1β in the cortex and striatum compared to control animals [35]. However, no midbrain DA neuron degeneration has been reported with haloperidol. Thus, haloperidol may be less relevant for studying novel neuroprotective or neurorepair strategies for PD (Table 1).
Neurotoxic models
6-Hydroxydopamine (6-OHDA)
Identified more than 60 years ago [36], the neurotoxin 6-OHDA is widely used to model PD by lesioning the nigrostriatal DA system [37,38,39]. 6-OHDA is a highly oxidizable DA analogue that transfers through the dopamine transporter (DAT) and the noradrenaline reuptake transporter. It exerts cytotoxic effects through different pathways: production of free radicals, and direct inhibition of MCI in the respiratory chain [40, 41] (Fig. 2). These different mechanisms may be linked to the generation of reactive oxygen species (ROS) and the release of cytochrome c, which leads to the activation of astrocytes and microglia [42, 43]. Because 6-OHDA does not cross the blood-brain barrier (BBB), an intracranial injection is required to exert its toxic effects [44]. In the past, at least three 6-OHDA lesional models have been used to mimic PD: an injection into the medial forebrain bundle, the SNpc, or the terminal regions of the nigrostriatal pathway in the striatum. The intravenous co-administration of desipramine helps protect the noradrenergic system from damage, and allows the targeting of catecholaminergic neurons, such as the DA neurons of the SNpc [40]. The 6-OHDA injection in the striatum leads to more progressive degeneration of DA neurons. In rodents, axonal denervation can be seen 3 h after injection in the striatum, while reduction of tyrosine hydroxylase (TH)-positive neurons in the SNpc is delayed by several days post-surgery [45, 46]. By comparison, an injection of the neurotoxin into the medial forebrain bundle or directly into the SNpc results in more severe and rapid neurodegeneration [47]. These injections result in motor impairments and non-motor phenotypes in rodents that include cognitive and gastrointestinal dysfunction [48,49,50,51]. This toxin not only induces a reduced expression of the lysosomal-associated membrane protein 1, but also impairs the hydrolase activities of lysosomal proteases [52]. 6-OHDA is not accompanied by α-syn aggregation or the formation of Lewy body-like inclusions. The 6-OHDA model is also used in Caenorhabditis elegans (C. elegans) [53], mainly for rapid studies such as drug screenings. More used in rodents, specifically in rats, the time course and severity of the 6-OHDA PD pattern depends on the amount and the injection location in the brain. No model has been developed yet for Drosophila melanogaster (D. melanogaster).
In summary, 6-OHDA is an affordable drug frequently used to generate rapid and specific neurodegeneration of the nigrostriatal system (Table 1). This model mimics several cellular processes identified in PD and is suitable for studying the molecular basis of cytotoxicity, oxidative stress processes, neuroinflammation, and neuronal death [43, 54, 55]. Although the 6-OHDA model has many advantages, its course differs from that observed in idiopathic PD, where neuronal degeneration occurs over the years. Despite its limitations, it remains an excellent tool for studying anti-PD drugs, L-DOPA-induced dyskinesia, or cell transplantation therapy.
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)
First discovered in humans, this neurotoxin soon became a vital research tool in the early 1980s. Mistaken for synthetic heroin, MPTP produced clinical and pathological PD features in young drug addicts [56]. After systemic administration, MPTP rapidly crosses the BBB and is metabolized to MPDP+ (1-methyl-4-phenyl-2,3-dihydropyridinium) by astrocytes [57]. The active toxic compound, 1-methyl-4-phenylpyridinium (MPP+), quickly enters DA neurons through DAT, where it binds to the VMAT and translocates to synaptosomal vesicles or remains within the mitochondria and cytosol (Fig. 2). MPP + leads to an acute deficit in ATP formation and ROS production, via binding to MCI, and ends in neuronal death [58]. Furthermore, MPTP administration drives microglial activation and cytokine release [59]. In humans and non-human primates, MPTP can replicate almost all the motor impairments of PD, including tremors, rigidity, slowness of movement, postural instability, and freezing [60]. The loss of SNpc DA neurons can also be accompanied by an almost complete depletion in DA and associated metabolites in the putamen [61]. It must be noted that this model is highly variable depending on the neurotoxin dosage, and the species and strains used. Unlike primates, rodents (and variable strains of mice) are less sensitive to MPTP toxicity and require multiple doses over several days to induce neuronal degeneration. Thus, an appropriate administration schedule is needed [62]. While mice treated with MPTP do not develop persistent and progressive motor dysfunctions [60], they are arguably a viable choice for studying neuroanatomical and neurochemical alterations. In the SNpc and ventral tegmental area (VTA) of treated mice, MPTP causes the loss of more than half of all DA neurons. Recent studies show that the administration of MPTP can increase the total and the phosphorylated α-syn as well as tubulin-associated unit (Tau) in the hippocampus and SNpc [63]. Hence, MPTP is widely used as a model to study the molecular and neuropathological events in PD, especially in non-human primates (Table 1).
Lipopolysaccharide (LPS)-induced neuroinflammation
In PD patients, a dense population of reactive microglia and astrocytes can be found in the brain, accompanied by an increased amount of pro-inflammatory cytokines, suggesting that neuroinflammation could play a key role in the pathogenesis [64]. Neuroinflammation can be modeled using LPS, an endotoxin produced by Gram-negative bacteria and is well-known for its pro-inflammatory properties. LPS binds the toll-like receptor 4 mainly expressed in microglia [65]. The use of LPS was initially intended for systemic inflammation models and the discovery of novel therapies in the treatment of acute inflammation [66, 67]. However, in 2001, a clinical case report showed that a 22-year-old laboratory worker developed PD syndrome after accidental exposure to Salmonella minnesota LPS through an open wound. Positron emission tomography confirmed that the subject also suffered from a dopaminergic neuronal loss in the SNpc [68]. Furthermore, two studies published earlier showed that injecting LPS into the SNpc of rats leads to neurodegeneration of nigral DA neurons [69, 70]. The neuronal loss is permanent and selective to DA neurons [71]. Since then, several LPS-induced models of PD have been developed, but their phenotypes greatly depend on the administration route [65, 72]. LPS can be delivered systemically or locally to the striatum, pallidum, or SNpc through intracerebral injections or intranasally.
While a few studies have used mice, LPS is more commonly used in rats [73,74,75]. Intrastriatal and intranigral injection of LPS in rats results in severe neurodegeneration of DA neurons from the SNpc with reduced striatal DA and motor impairments within a month [76,77,78,79,80,81,82,83]. Reduced MCI and II can be observed in nigral neurons [78]. A similar phenotype is seen when injecting LPS into the pallidum of rats, but motor impairments appear transient and return to normal after a few weeks [84]. It should be noted that using older rats can increase the severity of the phenotype [78, 84]. Furthermore, it has been reported that LPS increases the expression of α-syn in the brain [78, 85], the amount of oligomerized α-syn [86], and the expression of cytokines and activated microglia in both the SNpc and the striatum [78, 82]. Overall, local delivery of LPS to the brain generates features relevant to PD and can thus be used to clarify the role of neuroinflammation in SNpc DA neuron degeneration. However, the pathology is limited to the injection site.
Systemic injection of LPS in mice through intraperitoneal injection induces loss of DA neurons, motor deficits, and α-syn accumulation [85, 87, 88]. Autophagic impairment has also been described in nigral neurons with this route of administration [89]. It has been reported that there may be a delay in the appearance of the phenotype depending on the recurrence of the dose injected [72]. After a single intraperitoneal injection of LPS in mice, neurodegeneration of DA neurons can take several months [87, 88]; this delay can be reduced to 1 week by performing daily injections of LPS [85]. Recently, the administration of LPS through the nasal route in mice has gained popularity. A chronic administration via the nasal cavity leads to an approximate loss of 50% of DA neurons from the SNpc and reduces the amount of striatal DA within a month. This phenotype is accompanied by microglial activation, motor deficits, and a twofold increase of expression of α-syn in the SNpc [80, 90]. Lastly, bilateral administration can also be performed to increase the severity of the phenotype [91]. This route of administration could be used to better understand the involvement of environmental exposure through the nasal cavity in developing PD. Overall, LPS-induced PD models are useful in studying the role of neuroinflammation in PD (Table 1). However, the LPS-induced models could involve a more extensive phenotype that is less specific to PD characteristics. In fact, systemic LPS can be used as a chronic inflammation model of Alzheimer’s disease since it can cause memory deficits and an increase in Tau phosphorylation [92,93,94,95].
Agrochemical-induced models
Pesticide exposure is highly associated with PD development and is believed to influence its onset significantly. Epidemiological studies found that working in farming fields and pesticide exposure are positively associated with an increased risk of developing PD [96,97,98]. Rotenone, paraquat, and maneb are three pesticides that have been linked with PD onset [99, 100].
Rotenone
Rotenone was first introduced as a PD model in 2000 [101]. After systemic administration, the lipophilic property of rotenone allows it to cross the BBB and diffuse across the cellular membranes of neurons, inhibiting MCI and proteasomal activity. It induces oxidative stress and α-syn accumulation [102, 103]. In rodents, selective degeneration of the DA neurons from the SNpc and axonal denervation in the striatum arise within weeks, accompanied by motor impairments and α-syn inclusions [101, 104, 105]. Consistent with what is observed in idiopathic PD, rotenone activates microglia and impairs autophagy [106,107,108]. In lower-order species, such as C. elegans and Drosophila, rotenone can be used to mimic PD by inducing motor deficits and a loss of DA neurons [109]. Due to the genetic simplicity of these species, fast screening approaches can be used when looking for novel neuroprotective targets (Table 1). While rotenone reproduces several features of PD, the main limitation remains in its significant inter-individual variability [110, 111]. This might explain why no studies are reported using rotenone in non-human primates since a greater sample size would be required to account for variability [112].
Paraquat and Maneb
Paraquat is one of the most widely used herbicides in the world [113]. The mechanism of paraquat leading to PD remains unclear because it cannot cross the BBB. DAT does not directly transport paraquat, but paraquat can be converted to PQ2+, which seems to be the active agent penetrating the DA neurons through DAT [114] (Fig. 2). In rodents, paraquat administered alone has a mild effect on nigral neurons. This herbicide induces partial degeneration of DA cell bodies in the SNpc, without clear denervation of striatal fibers or motor impairments [115,116,117,118]. It also transiently increases the amount of α-syn protein leading to inclusions within SNpc DA neurons [119, 120]. Additionally, paraquat drives neuroinflammation and microglial activation [121]. However, particular attention must be given to the paraquat dose since it can result in pulmonary fibrosis, which might interfere with the motor behavioral assessment [122].
In agriculture, paraquat is often used in combination with other agrochemicals, such as maneb. The combined administration of paraquat and maneb in rodents increases the toxicity by inducing microglial activation, a significant loss of DA neurons from the SNpc and striatal fibers, as well as motor impairments [115, 117, 118, 123, 124]. However, in rats, the combined exposure does not seem to affect striatal DA fibers [115, 123]. Over the last two decades, interest has grown in using paraquat to mimic PD in animal models such as Drosophila [125] and C. elegans [126] since it efficiently causes the loss of DA neurons, and increases ROS levels, cellular dysfunction and motor impairments. In these species, this agrochemical can be used to perform neuroprotective studies by fast screening or to study the gene interaction pathogenesis (Table 1). Although rats are an exception, paraquat and maneb models successfully reproduce many PD hallmarks.
PD-associated gene models
It is estimated that up to 10% of diagnosed cases of PD have a familial origin [2]. Several genes have been identified as risk factors for PD, including Parkin RBR E3 ubiquitin-protein ligase (PRKN), PTEN-induced putative kinase 1 (PINK1), Leucine-rich repeat kinas 2 (LRRK2), Daisuke-Junko-1 (DJ-1), ubiquitin carboxy-terminal hydrolase L1 (UCH-L1), and β-glucocerebrosidase (GBA1) [127]. In animals, the manipulation of most of these genes can mimic some features of idiopathic PD, such as Lewy body-like formation, and lysosomal and mitochondrial dysfunction. The SNCA gene, encoding α-syn protein, is also heavily implicated in genetic and sporadic forms of PD [128]. Existing SNCA transgenic models will be discussed in the following section.
PRKN and PINK1
Of all the familial forms of PD, PRKN is the most frequently mutated gene accounting for about 50% of early-onset genetic cases, followed by mutations in PINK1, which represent up to 8% of early-onset familial forms of PD [127]. PRKN and PINK1 are both involved in the mitochondrial stress response and are believed to act along the same pathway. Indeed, mitochondrial stress leads to the accumulation of PINK1 within mitochondria and initiates autophagy of damaged mitochondria through the recruitment of PRKN [129] (Fig. 2). PRKN and PINK1 mutations are recessive and generally lead to a loss of function. Interestingly, almost all clinical cases of PRKN-induced parkinsonism lack Lewy body pathology [130].
In C. elegans and Drosophila, genetic deletion of the ortholog form of human PRKN and PINK1 results in typical Parkinson-like phenotypes. In C. elegans, these mutations are associated with motor impairment, mitochondrial dysfunction, and loss of DA neurons [131, 132]. In Drosophila, PINK1 ortholog deletions lead to the development of similar features, with the addition of the degeneration of muscles [133]. PRKN ortholog-deficient Drosophila have a comparable phenotype, except for the absence of DA neuron loss [134]. These models are particularly suitable for fast screening approaches when studying PRKN/PINK1 regulatory mechanisms involved in the pathogenicity. In mice, the genetic deletion of both PINK1 and PRKN leads to mitochondrial dysfunction and neuroinflammation without affecting the basal mitophagy. This model does not appear to exhibit α-syn aggregates, behavioral abnormalities, reduced striatal DA levels, or loss of nigral DA neurons [135, 136]. However, it is possible that neurodegeneration only occurs in older mice. In fact, a recent study showed that hind limb defects and loss of DA neurons in the SNpc can be seen in 2-year-old PRKN knock-out (KO) mice [137]. Thus, mice lacking PINK1 or PRKN might be used to better understand the role and the involvement of these genes in vivo. Nevertheless, the time required for these mice to develop neurodegeneration could be a major limiting factor for using this model in neuroprotective studies. Recently, a non-human primate model with a genetic deletion of PINK1 was generated. This model presents behavioral abnormalities at 1.5 years of age and DA neuron degeneration in the SNpc at 3 years of age, without changes in mitochondrial morphology [138]. It is still unknown if these animals develop Lewy body-like inclusions. While the loss of PINK1 more closely reflects parkinsonian phenotypes, this model is not yet fully characterized. Further studies are needed to assess its importance as a PD animal model (Table 1). Although promising and relevant to PD, no PRKN-transgenic model in non-human primates has been generated. This model requires specialized expertise and installations to maintain these animals, which may exceed the technical capacities of many research teams.
LRRK2
Mutations in the LRRK2 gene are dominant and account for around 4% of familial cases of PD [139]. LRRK2 is a protein containing both a kinase and a GTPase domain. In addition, this gene interacts with many proteins, regulating various cellular functions (Fig. 2), including autophagy, mitochondrial functions, and vesicular trafficking [140]. Most LRRK2 mutations, such as G2019S and R1441C/G, affect one of the enzymatic domains. Hyperactivity of LRRK2 kinase has also been observed in idiopathic cases [141]. While DA neuron loss from the SNpc is one characteristic of parkinsonian patients carrying a LRRK2 mutation, approximately 21%–54% of these clinical cases do not show apparent Lewy bodies [149, 150], suggesting that this mutation could induce neurodegeneration through another factor than synucleinopathy. Some evidence indicates that the toxic effect might be mediated through the protein Tau, since about 79% of PD patients carrying a LRRK2 mutation show some features of Tau pathology [142]. In C. elegans and Drosophila, overexpression of human wild-type (WT) or G2019S and mutated LRRK2 causes motor dysfunctions and progressive degeneration of DA neurons [144,145,146,147,148]. LRRK2 G2019S overexpression in both species results in mitochondrial and autophagic dysfunction [144, 146, 147, 149]. In Drosophila, overexpression of the G2019S mutated form of LRRK2 induces a loss of dendritic arborization by hyperphosphorylation of endogenous Tau. Furthermore, overexpression of the Drosophila ortholog of WT LRRK2, Lrrk, has been seen to increase the neurotoxicity of pathological Tau when the human mutated R406W form of Tau is expressed [148]. The Drosophila model can therefore be useful in understanding the interaction of LRRK2 and Tau pathology. Moreover, as C. elegans and Drosophila do not naturally express α-syn, the function of LRRK2 can additionally be studied in the absence of endogenous α-syn.
In mice, G2019S LRRK2 overexpression and Knock-In (KI) models generate synaptic alterations, impaired DA transmission, behavioral abnormalities and increased Tau phosphorylation [150,151,152,153,154,155,156]. These rodent models usually lack degeneration of DA neurons in the SNpc, unless the mouse line overexpresses G2019S LRRK2 under the neuron-specific platelet-derived growth factor beta (PDGF-β) promoter. These transgenic mice show striatal denervation, DA neuron degeneration, and increased phosphorylated Tau protein in the SNpc at 16 months of age [157]. Features of neuroinflammation, as well as autophagic and mitochondrial abnormalities are also present despite the absence of synucleinopathies [158, 159]. More recently, neurodegeneration has been reported in a mouse line expressing G2019S LRRK2 in DA neurons under the TH promoter. The alteration drives a progressive loss of DA neurons in the SNpc by 15 months of age, with additional neuronal loss observed in the olfactory bulb and locus coeruleus. By 24 months of age, this phenotype is accompanied by reduced synaptic vesicles in the DA neurons, motor deficits, and an increased amount of phosphorylated α-syn [160] (Table 1). Overall, LRRK2 mutant mice might be used to study the pathogenesis of PD and to identify neuroprotective therapies aimed at inhibiting its kinase activity or its downstream targets.
DJ-1
First discovered as a novel oncogene in 1997 [161], the DJ-1 gene encodes a protein of the peptidase C56 family. It is also known for its function against oxidative stress [162, 163] via its direct interaction with mitochondria [164] and DA neurons in the SNpc, which drive the nigrostriatal motor pathway inhibition (Fig. 2) [165]. Deficiency of DJ-1 has been identified as a causative factor in familial PD with recessive inheritance [166], where it downregulates the level of lysosomal 70 kDa heat-shock cognate protein. By simultaneously inhibiting the activation of chaperone-mediated autophagy, DJ-1 deficiency may augment α-syn aggregation [167] and mitochondrial abnormalities [168] in PD. Although DJ-1 KO mice exhibit alterations in DA metabolism, the KO alone is not sufficient to induce loss of DA neurons and PD-like signs in young mice. However, in older mice, there are significant DA neuronal losses and motor deficits [169]. A similar age-dependent difference is also visible in the Drosophila model with two existing orthologs for DJ-1 [170]. While the major limitation of this model lies within the prolonged time required for a phenotype to appear, it remains promising, as ageing seems to be a crucial factor in progressive neurodegenerative diseases like Parkinson’s. Because PD similarly evolves in older adults, this progressively developing model may be suitable for targeting the earlier phases of the phenotype induction and its subsequent manifestation.
Recent studies have used MPTP hybrid models that take advantage of the usual role DJ-1 has as a negative regulator of the inflammatory response, alleviating neuroinflammation, and playing an essential role in neurodegeneration [171]. DJ-1 KO mice tend to present PD-like pathology after MPTP treatment, resulting in accelerated DA axonal denervation in the striatum, DA neuron loss in the SNpc, and motor impairments after 2 weeks [165]. The MPTP treatment accelerates the phenotype seen in KO models alone by increasing the oxidative stress burden [163] (Table 1).
UCH-L1
UCH-L1 is a deubiquitinating enzyme believed to be one of the most abundant proteins in neurons, accounting for about 1%–5% of the total amount of proteins in the brain [172]. The first association between the UCH-L1 gene and PD was revealed in 1998, following the identification of the autosomal mutation I93M in the pedigree of a German family [173]. Although this mutation is rare, UCH-L1 localizes with Lewy bodies in some sporadic cases of PD [174, 175]. While UCH-L1 is involved in the clearance of proteins via the ubiquitin-proteasome system, a recent study also suggests that UCH-L1 can modulate mitochondrial functions by regulating the expression of Mitofusin-2 [176] (Fig. 2). To date, there are relatively few transgenic animal models for UCH-L1. In mice, the deletion of UCH-L1 induces axonal degeneration in sensory and motor nerve terminals [177,178,179] without affecting DA nigral neurons [175]. The only transgenic mouse model that affects the DA neurons of the SNpc is the UCH-L1 I93M mice, which overexpress I93M mutated UCH–L1 under the control of the PDGF-β neuron-specific promoter [180]. Although these mice may be useful for studies aimed at discovering neuroprotective therapies for PD by targeting UCH-L1 activity, this approach is limited because UCH-L1 I93M transgenic mice lack α-syn inclusions. Furthermore, the degeneration of DA neurons and motor deficits can take more than 20 months to develop [180]. To accelerate the degeneration of SNpc DA neurons, this model has been previously combined with viral α-syn overexpression [175]. More recently, knock-down (KD) of the UCH-L1 ortholog gene (dUCH) in a Drosophila PD model was created using the GAL4-UAS system. This model exhibits motor alterations, degeneration of DA neurons, and a reduction in the level of DA in the brain [181], thus making this model appropriate for fast screening approaches to identify UCH-L1 interactors (Table 1).
GBA1
Mutations in GBA1 are among the most common genetic risk factors for PD and Lewy body dementia [182, 183]. The GBA1 gene is located on chromosome 1q21 and encodes the lysosomal glucocerebrosidase enzyme (GCase) [184]. Thus, GBA1 mutations induce a deficiency of GCase activity that leads to an accumulation of glycosphingolipids [185]. Clinical, epidemiological, and experimental studies have confirmed a connection between PD and Gaucher disease, a prevailing autosomal recessive lysosomal storage disorder [186]. Recently, GBA1-derived PD clinical cases have shown impaired DA neurotransmission early in the pathogenesis, although the underlying mechanisms are still not well understood. So far, approximately 130 different GBA1 mutations have been observed in patients with PD. The most frequent cases with declined GCase activity are the L444P and N370S GBA1 mutations [185, 187, 188]. Recent studies have focused on the association between mutated GBA1 and PD, highlighting the possibility that lysosomal impairment and altered GCase activity could facilitate the proliferation of α-syn aggregates [188,189,190]. Today, several animal models of GBA1 have been created [182]. GBA1-associated PD mouse models combine a GBA1 mutation with overexpression of α-syn mutations to generate α-syn aggregation and pronounced PD-like signs. Additionally, different KI models carry the human L444P GBA1 gene [191]. GBA1 L444P homozygous mice show an increase of α- syn accumulation in the striatum and astrogliosis at 1 year of age [192]. GBA1 L444P heterozygous mice develop mitochondrial dysfunction, increased ROS production, impaired neuronal autophagic degradation [193], and higher levels of α-syn [194], but fail to develop α-syn aggregates even by 24 months of age [194]. Unlike L444P, heterozygosity for N370S does not affect phenotype progression in A30P-SNCA mice [193], and N370S homozygote mice die at birth. Injection of adeno-associated virus (AAV) expressing N370S GBA1 in the striatum of A53T-SNCA mice results in increased α-syn protein, defects in mitophagy, and abnormal autophagy [191, 193]. GBA1-associated PD models can also be found in Drosophila and C. elegans. In these PD-GBA Drosophila models, an increased aggregation of mutant α-syn A53T is observed, causing enhanced DA neuronal loss and exacerbating the motor and non-motor phenotypes [195]. Drosophila expressing the mutant human N370S and L444P variants exhibit a significant decrease in GCase activity and present parkinsonian features with DA cell death, defective locomotion, and a shorter lifespan [196]. Overall, fly models expressing human WT or N370S and L444P GBA1 provide an interesting tool to assess the contribution of defective GCase function to PD development. In C. elegans expressing a human α-syn, KD of GCase ortholog, C33C12.8, increases aggregation of α-syn [197], similar to what has been described in other animal models [198]. In sum, GBA1-associated models of PD provide insight into the pathogenesis by replicating many hallmarks of the disease. GBA1 models show increased α-syn accumulation, disruption of lysosomal homeostasis, exacerbated endoplasmic reticulum stress, and mitochondrial dysfunction. These cellular features lead to DA neuron death and motor phenotypes, making them an appealing tool for studying PD (Table 1).
Transcription factors
During the development of midbrain DA neurons, transcription factors play key roles in specifying and differentiating neural progenitors. Interestingly, most of these transcription factors remain expressed in the adult brain [199, 200]. Indeed, Lmx1a/b, Otx2, Foxa1/2, Pitx3, Nurr1, and En1/2 are present throughout development and are required for the survival of midbrain DA neurons [201,202,203,204]. Genome-wide association studies have revealed genes that may contribute to PD [205]. Among them, genetic variants of human transcription factors such as Lmx1a and Lmx1b were found [204, 206,207,208], with the expression of Lmx1b being notably decreased in the DA neurons of PD patients [209]. Lmx1a and Lmx1b are LIM homeodomain transcription factors essential for the development of midbrain DA neurons [210,211,212,213] and are still expressed in post-mitotic midbrain DA neurons [214,215,216]. Conditional deletion of Lmx1a and Lmx1b genes in mouse DA neurons induces progressive neurodegeneration in the SNpc and VTA [203, 217]. Lmx1a and Lmx1b are particularly important in regulating mitochondrial [217] and autophagic-lysosomal functions [209]. Moreover, loss of Lmx1a and Lmx1b leads to α-syn pathology with the accumulation of α-syn in both DA axons and cell bodies [217]. Specific deletion of Lmx1a and Lmx1b in adult DA neurons also leads to progressive loss of DA neurons, α-syn pathology, and motor impairments [209, 217]. Depletion of Otx2, Foxa1/2, and Pitx3 leads to a reduction of midbrain DA neurons with motor deficits [218,219,220,221,222,223]. While heterozygous KO mice for Nurr1 and En1 develop progressive loss of DA neurons with motor deficits [224, 225], total depletion of Nurr1 [224, 226] and En1 [227] in midbrain DA neurons is embryonically lethal. Lastly, KO of the transcription factor c-Rel can induce α-syn aggregation in the SNpc, midbrain DA neuronal loss, and motor deficits [228] (Table 1). Overall, several signs of PD can be reproduced by modulating the expression of DA transcription factors; however, the phenotype is restricted to DA neurons. Most of these models also require multiple crosses to obtain a conditional deletion in adult mice, which could thus represent a limiting factor.
Mitochondrial impairment
Several lines of evidence have previously linked mitochondrial dysfunction to PD pathogenesis [229, 230]. This is supported by a large set of PD-associated genes that are involved in mitochondrial function [231, 232]. Furthermore, α-syn and neurotoxins linked to PD, including MPTP and rotenone, are known to inhibit MCI activity [233]. MCI deficiency was also reported in DA neurons of the SNpc for human PD post-mortem brains [234]. One of the first transgenic mouse models of PD to induce mitochondrial impairment in DA neurons was created by crossing DJ-1-deficient mice with a mouse strain encoding a mutated mitochondrial polymerase gamma, resulting in an accelerated accumulation of mitochondrial DNA errors. Even at 1 year of age, these mice do not exhibit behavioral abnormalities, degeneration of nigrostriatal DA neurons, or evidence of neuroinflammation [235]. A similar phenotype has recently been observed in mice lacking PRKN [236].
In mice, conditional deletion of the Ndufs4 gene (which encodes a subunit of MCI) in DA neurons results in loss of striatal DA at 9 months, followed by increased α-syn phosphorylation in DA neurons at 24 months of age. However, deletion of Ndufs4 in DA neurons does not cause motor deficits or DA neuron degeneration in the SNpc [237]. One possible explanation for this phenotype is that Ndufs4 KO results in about 65% reduction of MCI activity [237] and DA neurons could compensate for the lack of oxidative phosphorylation [238]. Recently, another model of MCI disruption by deletion of the essential MCI subunit Ndufs2 in DA neurons was generated. Compared to the Ndufs4 KO model, the KO of Ndufs2 almost completely disrupts the oxidative phosphorylation activity in DA neurons. Deletion of Ndufs2 induces loss of DA axons in the dorsal striatum by 1 month of age, followed by motor deficits after 1 to 2 months. These motor deficits are accompanied by a decrease in the number of cells expressing TH in the SNpc. However, despite the decrease in TH expression, there is no loss of dopaminergic cell bodies [238]. No α-syn aggregates have been observed in this model, but it might be because that these mice die at 5–6 months of age before developing α-synucleinopathies [238]. Additional characterization of neuroinflammatory and autophagic features is still needed. However, the Ndufs2 KO mouse model remains of interest in the study of neuroprotective therapies aiming to rescue oxidative phosphorylation or MCI activity.
α-syn models
The α-syn protein, encoded by SNCA, has a central role in PD, although its physiological function is not yet fully understood. Usually clustering into monomers and tetramers [239, 240], α-syn assembles into higher-order structures under pathological conditions. These oligomers, protofibrils, and fibrils form insoluble aggregates that are toxic to neurons [241]. As a principal constituent of Lewy bodies [242], these aggregates can not only alter the integrity of the cell membrane, but may also disrupt the functions of mitochondria, the Golgi apparatus, and the endoplasmic reticulum [243] (Fig. 2). At least eight different identified missense mutations of SNCA (A53T/E/V, A30P/G, E46K, H50Q and G51D) [244], gene duplication, and triplication have been linked to the accumulation of pathologic α-syn in the brain [245]. This new knowledge gave rise to several animal models mimicking α-syn pathology. Transgenic models expressing WT, A53T, A30P, and E46K SNCA mutations have been utilized to recapitulate PD pathology in vivo. However, to date, there are no reported studies on A53E, A53V, A30G, H50Q, or G51D transgenic models, which could be of interest for future investigations.
WT and truncated human α-syn
As one of the first transgenic animal models of α-syn, the mouse line 61 (M61) is generated by overexpressing human WT α-syn using the neuron-specific Thymocyte differentiation antigen 1 (Thy1) promoter [246]. Mitochondrial dysfunction and neuroinflammation have been described in these mice [247, 248]. Moreover, motor deficits and α-syn inclusions appear within a few months of age, although nigral DA neurons are only mildly affected. In fact, while a decreased amount of striatal DA and axonal denervation are observed, no degeneration of DA neurons in the SNpc is reported [246, 249]. M61 mice have thus been used to test candidate drugs targeting α-syn aggregation and axonal denervation. The MI2 mouse line expressing C-terminal-truncated human α-syn under the TH promoter shows α-syn aggregates in DA neurons by 1.5 months of age. By 9 months, motor impairments appear; by 12 months, a significant loss of DA neurons in the SNpc can be seen [250]. Additionally, because MI2 mice possess a null endogenous α-syn background, human α-syn seeding is facilitated. However, since the α-syn expression is restricted to DA neurons, the MI2 mouse line does not recapitulate synucleinopathies in other brain regions.
E46K human α-syn
Identified within a Spanish family with autosomal dominant parkinsonism and dementia, the cortical and subcortical Lewy body pathology found was attributed to a shared nonconservative heterozygous E46K mutation within α-syn [251]. While the mutant mouse PD models created based on this mutation are still recent and warrant further research, this initiative can provide insight into familial PD and synucleinopathies. Transgenic mouse lines carrying the PrP (Prion protein)-driven E46K mutation have been generated. The mouse line 47 (M47) shows higher levels of α-syn transgene expression, with motor impairments starting at 15–16 months of age. These mice develop α-syn inclusions in the spinal cord, brainstem, deep cerebellar nuclei, motor cortex, and most of the thalamus. The inclusions and affected areas are accompanied by phosphorylation of α-syn, significant astrocytic gliosis, elevated reactive microglia, and Tau inclusions [252]. DA neurons of the SNpc remain spared of α-syn inclusions. These results may corroborate those observed in rat models with the same mutation, where no loss of DA neurons or striatal terminals was reported [253].
A30P α-syn
The A30P α-syn mutation was first detected in a German family [254]. The few existing transgenic mouse strains that model the A30P mutation include overexpression of the human A30P α-syn gene under the Prp promoter (Prnp-A30P) [255] or the Thy1 promoter (Thy1-A30P) [256], and a KI mouse model with an introduced A30P point mutation in the WT gene [255]. All these A30P models show an increase and accumulation of α-syn in neuronal cell bodies with age. However, it is most robust in the Prnp-A30P mice. For Thy1-A30P α-syn transgenic mice, abnormal α-syn protein is observed in several brain regions like the superior colliculus or the cerebellum, but α-syn pathology is spared in the striatum and SNpc [255]. Mitochondrial oxidative stress and autophagy defects are also reported in A30P models [257]. Only the neuronal cell loss in the SNpc does not seem to be consistently detectable. While Thy1-A30P mice show reduced TH levels in the SNpc at 8 and 11 months [256], the loss of DA is not visible in the strains [255, 258]. Locomotor disabilities and α-syn aggregation seen in rodent models are similarly observed in flies overexpressing the A30P mutant form of α-syn. Flies also exhibit selective loss of DA neurons when A30P is expressed in all neurons [259, 260]. In C. elegans, A30P α-syn models are mild. Compared to control animals, worms expressing A30P α-syn in muscles have modest reduction of movement speed and increased rate of paralysis [261]. In a C. elegans model of A30P under the control of the DAT-1 (C. elegans DAT) promoter, the expression is restricted to DA neurons. The worms exhibit DA neuron-specific dysfunction caused by accumulation of α-syn but do not show significant neurodegeneration compared to controls, even at 15 days of age [262]. Overall, the A30P models show mild phenotypes. The progressive and relatively long development of pathological abnormalities, such as α-syn accumulation and motor disorders, may provide an interesting approach to study the early stages of PD.
A53T human α-syn
The A53T mutation in the α-syn gene was initially identified in Italian and Greek pedigrees [263]. The PrP-driven mouse line 83 (M83) was the first to be genetically engineered to overexpress human A53T α-syn. M83 mice show a mid-to-late onset of neurodegenerative phenotype with evidence of dystrophic neurites. They present increased phosphorylated α-syn and aggregation, similar to patients [264,265,266,267]. These inclusions become apparent between 8 to 16 months of age in homozygous M83 mice, resulting in motor impairments. Like M47 mice, the highest density of these inclusions is localized in the spinal cord, brain stem, deep cerebellar nuclei, white matter, and some thalamic regions. An identical inclusion profile arises in hemizygous M83 mice between 22 and 28 months of age when animals spontaneously develop motor dysfunction [264]. No loss of DA neurons has been reported, and there is no alteration of striatal DA at 12 months of age in M83 homozygous mice [268]. Altogether, this mutation owes its pathological nature to its tendency to form α-syn inclusions, much like in the clinical setting. While the location of pathological lesions in mice does not precisely mirror the human condition, they do share many similarities, such as neuroinflammation, as well as autophagic and mitochondrial dysfunction [269,270,271,272]. This human A53T mutation model is proposed to be a valuable asset in screening potential therapeutics that inhibit or reverse α-syn aggregate formation or spreading.
α-syn preformed fibrils (PFFs)
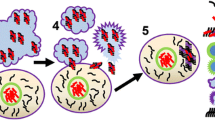
PFFs are first generated from monomeric recombinant α-syn. When fragmented by sonication, PFFs can phosphorylate endogenous α-syn into its pathological state [273]. In mice, α-syn spreading is enhanced with PFFs generated from brain homogenates of aged symptomatic α-syn mice or human samples, or recombinant synthetic α-syn fibrils (Fig. 2). In WT mice, injection of mouse PFFs in the dorsal striatum induces hyperphosphorylation of α-syn within 30 days [274]. Degeneration of DA striatal fibers and cell bodies in the SNpc, as well as motor impairments, occurs 6 months post-injection [274]. Whole-brain homogenate extracts of parkinsonian symptomatic M83 mice can be injected into the M83 mice at birth to accelerate the development of the phenotype and α-syn aggregation [275,276,277]. There is also a robust inflammatory response before end-stage paralysis occurs by 8 to 16 months in homozygous mice and by 22 to 28 months in heterozygous mice [278]. Similarly, extracts from post-mortem PD brain tissues have previously been used in the intranigral and intrastriatal inoculation of WT mice and macaque monkeys. The fractions enriched with nigral Lewy bodies have demonstrated the ability to induce pathogenic effects, such as progressive nigrostriatal neurodegeneration and the accumulation of pathological α-syn, which cannot be achieved by non-Lewy body fractions or vehicle buffers [279]. A new alternative created with the bacterial artificial chromosome plasmid consists of A53T overexpressing mice injected with recombinant synthetic α-syn. This hybrid model produces phosphorylated α-syn inclusions and striatal DA denervation within 2 weeks post-injection [280]. Within 1 month, there is 25% DA neuronal loss in the SNpc. Motor impairments were reported at 2 months post-injection [280], but they can be expected to appear earlier since DA denervation appears before this time point [277]. In cell-based models, PFFs were shown to additionally produce autophagic and mitochondrial dysfunction [281, 282]. Lastly, recent studies in 26-month-old non-human primates have shown that PFFs are also sufficient to drive phosphorylated α-syn accumulation and DA neuronal loss by 3 months post-injection [273]. However, the injection site of the PFFs is consequential in further characterizing the α-syn seeding and spreading [274, 277, 283]. We cannot overlook that α-syn transmission also occurs in the periphery and that α-synucleinopathy in the brain may develop via the gut-to-brain axis [284]. Inoculation of the rodent gut with PFFs results in midbrain DA neuron loss, α-syn histopathology, and motor defects in a temporal manner [285,286,287]. Nevertheless, despite differences from the human pathology, PFFs can reproduce specific aspects or stages of α-syn pathology, as well as neurodegenerative and neuroinflammatory hallmarks of PD [288]. Overall, both in vitro and in vivo, fibril formation and aggregation are not synonymous with pathological aggregation and LB formation. Therefore, strict quality control must be taken so that the pathogenicity of the PFFs used ensures reproducible results [284, 289, 290].
Non-mammalian models of α-syn
Non-mammalian models, including those based on C. elegans and D. melanogaster, do not produce α-syn endogenously. In C. elegans [291,292,293] and Drosophila [294,295,296], the overexpression of human WT and A53T α-syn in an ubiquitous or DA-specific manner induces α-syn aggregates, mitochondrial fragmentation, motor impairments, and loss of DA neurons. These non-mammalian models offer an interesting way for rapid screening of anti-aggregation targets. However, they might be too simplistic to transpose the results directly to complex and still not fully understood mechanisms of aggregation, propagation, and toxicity of synucleinopathies in the human brain.
Viral vector-mediated models
α-syn viral expression
Another alternative to model PD in animals is to overexpress WT or mutated α-syn, including A53T and A30P forms [297], using lentiviral [298] or AAV vectors [299, 300]. These viral vectors can transduce diverse cell types and drive the expression of α-syn in the brain region of interest [301]. This technique thus makes it feasible to study the possible transmission of α-syn pathology from the periphery to the central nervous system [302]. In general, α-syn overexpression in the SNpc results in the progressive DA neuron loss, and DA projection decrease in the striatum within weeks to months, and models early and late hallmarks of PD pathogenesis, depending on the model organism [300, 303,304,305]. However, studies have yielded variable results, showing a range from slight to substantial loss of DA neurons. Several factors, including virus titer or serotype, age, sex, strain, or species of the animal, can strongly influence the outcomes obtained (see [306, 307] for reviews). In rodents, viral α-syn overexpression results in an approximate 40% DA cell loss in the SNpc, accompanied by motor deficits at 8 weeks post-injection [308]. Less commonly used, non-human primates receiving intranigral AAV injections of WT or A53T α-syn show a ~ 30% loss of nigral DA neurons 8 weeks post-injection. Like rodents, non-human primates also develop motor deficits with a progressive deterioration of motor coordination after 16 weeks, albeit with a greater variability [309]. Non-human primates enable a more extended period of studies on the effects of α-syn injections than their rodent counterparts [310, 311]. Moreover, monkeys were found to be more vulnerable to neurodegeneration and pathologies induced by injections with viral vectors that encode A53T α-syn [311]. Overexpression of α-syn in the midbrain typically leads to mitochondrial dysfunction [312], impaired autophagy [313], Lewy body-like structures [300, 314], and an early and persistent inflammatory response [315,316,317,318]. Recently, a light-inducible α-syn aggregation system (LIPA) was designed to regulate spatiotemporal protein aggregation [319]. This system could control α-syn aggregation into insoluble deposits that mimic key features of Lewy bodies. LIPA is encoded in a viral vector and injected into the SNpc. The α-syn aggregation is then induced by light stimulation through an optical fiber implanted above the injection site. Following repeated optogenetic stimulations, the nigrostriatal transmission is compromised, leading to Lewy body-like structure formation, neurodegeneration, and motor impairments within 2 months. This inducible model of α-syn aggregation allows for real-time monitoring of α-syn aggregation and Lewy body-like formation with high spatiotemporal control. Altogether, viral vectors are very versatile and powerful tools that offer the opportunity to closely mimic PD pathology by inducing the overexpression of α-syn within multiple animal species (Table 1). Viral overexpression allows us to study α-synucleinopathy more precisely and to follow the progressive development of PD-like phenotypes. Lastly, this tool may also target other non-dopaminergic systems, following the impact of α-syn in the periphery or other neuronal cell populations.
Viral neuromelanin (NM)-like production
Neurodegeneration is particularly prominent within brain regions containing NM. In 1919, a visually noticeable loss of pigmented neurons in the SNpc was first reported by Konstantin Tretiakoff [320]. This pigmentation loss in the brains of PD patients referred to a decrease in NM concentration, which was less than 50% of the expected levels for age-matched healthy individuals [321]. NM pigment appears black and consists of melanin, proteins, lipids, and metal ions. It can be found in different human central nervous system neurons and is particularly abundant in DA neurons of the SNpc and noradrenergic neurons of the locus coeruleus. The pigment itself is contained within specific types of lysosomes fused with autophagic vacuoles [322]. Additionally, DA and norepinephrine appear to be the principal substrates in its synthesis. However, NM may have both a protective and a toxic effect, depending on the conditions of the neuronal environment. Under physiological conditions, NM is proposed to have a protective role via iron binding. In PD, iron-bound NM can easily release excess iron, producing a toxic effect via redox processes. Moreover, the iron overload of NM can catalyze DA oxidation, forming DA-o-quinone, and modifying proteins that trigger neurotoxic effects [323] (Fig. 2). Yet, the structure and function of human NM in PD have proven to be difficult to investigate due to the limited quantities available for extraction from human brain tissues. Furthermore, animal models including rodents lack NM. Nevertheless, recent in vivo models have been explored, reporting microglial activation via intranigral synthetic NM injections [324,325,326]. A new approach was applied in rodents to virally express human tyrosinase (hTyr) in the SNpc. This model shows NM-like pigment accumulation in SNpc DA neurons in an age-dependent manner. In fact, overexpression of hTyr recapitulates the principal hallmarks of PD: mice show mitochondrial and autophagic dysfunction, as well as neuroinflammation. They also have impaired DA release, striatal denervation, loss of DA neurons in the SNpc, and motor deficits by 4 months post-injection [327]. This is accompanied by Lewy body-like structures and autophagic dysfunction within NM-like positive neurons [327, 328]. Therefore, this model provides a valuable experimental tool to study the effects of NM production and accumulation on neuronal function and viability (Table 1).
Discussion
Modelling PD pathogenesis remains a difficult task. Several animal models have been developed to understand the pathogenesis and test new drug candidates against PD. However, PD is a highly heterogeneous disease involving several factors and pathways that may differ among clinical cases. Therefore, none of the existing and future models will replicate the entire spectrum of clinical features listed in PD. In this review, we tried to summarize the most relevant PD animal models, their respective advantages and disadvantages, as well as their ability to reproduce the main hallmarks of PD.
The choice of the animal model must be based on the PD features addressed by the question the experimenter seeks to answer. Neurotoxin-induced animal models remain popular due to their cost-effectiveness in generating a PD-like phenotype in a relatively short time span. Thus, they are commonly used in drug validation for symptomatic treatment of PD or cell replacement therapy. On the other hand, to investigate the function of PD-linked genes in disease development, transgenic models should be considered. Other questions concerning the targeting of α-syn pathology can also be answered in animal models injected with PFFs or viral vectors encoding SNCA gene copies. In the absence of a suitable model fully recapitulating the targeted PD features of interest, a possible solution could be to complement the phenotypes by combining some of the listed models.
The selection of animal species is equally as important. Although the translational results to humans are valuable in mammalian models, the use of rodents and primates for drug or gene screening is untenable. C. elegans and Drosophila could be considered to identify novel neuroprotective targets [293, 329]. However, the simplicity and lack of similarity with humans are limitations. Moreover, research in PD should not be limited to the use of in vivo models. Although animals offer a better pre-clinical prediction of a drug effect, in vitro models could provide complementary information on the underlying molecular mechanisms [330]. Still, most in vitro-based models cannot reproduce the non-cell autonomous impact of the complex cell network in the brain. The near future could shed light on the use of human brain organoids to perform drug or gene screenings, although additional characterization of these emerging models will be required [330, 331].
Conclusion
Despite efforts devoted to interpreting the pathogenesis of PD, the initial source of neuronal degeneration remains unclear. There is considerable evidence to suggest that α-syn aggregation, neuroinflammation, as well as lysosomal and mitochondrial dysfunction could all play a key role in neurodegeneration [3]. Basic research has yet to reconcile these features, discriminating causes from consequences in the PD pathogenesis. Existing animal models, many of which recapitulate multiple disease features from cellular pathology and pathogenesis to motor and non-motor symptoms, open new possibilities. However, the wide range available can make choosing a model for a given study challenging. This task becomes particularly complex if the study addresses multiple aspects of PD. This review compiles information on the diversity of animal models, and is therefore, a support for researchers to select the optimal animal model for their study. Carefully constructed research models are an essential first step to understand the disease and discover novel therapies, possibly improving the quality of life and the clinical fate of patients.
Availability data and materials
Not applicable.
Abbreviations
- 6-OHDA:
-
6-Hydroxydopamine
- AAV:
-
Adeno-associated virus
- α-syn:
-
α-synuclein
- BBB:
-
Blood-brain barrier
- DAT:
-
Dopamine transporter
- DIP:
-
Drug-induced parkinsonism
- DJ-1:
-
Daisuke-Junko-1 gene
- dUCH:
-
UCH-L1 ortholog gene
- GBA1:
-
β-Glucocerebrosidase
- GCase:
-
Glucocerebrosidase enzyme
- hTyr:
-
Human tyrosinase
- KD:
-
Knock-Down
- KI:
-
Knock-In
- KO:
-
Knock-Out
- L-DOPA:
-
Levodopa or l-3,4-dihydroxyphenylalanine
- LIPA:
-
light-inducible α-syn aggregation system
- LPS:
-
Lipopolysaccharide
- LRRK2:
-
Leucine-rich repeat kinase 2
- MCI:
-
Mitochondrial Complex I
- MPP+:
-
1-methyl-4-phenylpyridinium
- MPTP:
-
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- NM:
-
Neuromelanin
- PD:
-
Parkinson’s disease
- PDGF-β:
-
Platelet-derived growth factor beta
- PFF:
-
Preformed fibril
- PINK1:
-
PTEN-induced putative kinase 1
- POLG:
-
polymerase gamma
- PRKN:
-
Parkin RBR E3 ubiquitin-protein ligase or PARKIN
- Prp:
-
Prion protein
- ROS:
-
Reactive oxygen species
- SNpc:
-
Substantia nigra pars compacta
- Tau:
-
tubulin-associated unit
- TH:
-
Tyrosine hydroxylase
- Thy1:
-
Thymocyte differentiation antigen 1
- UCH-L1:
-
Ubiquitin carboxy-terminal hydrolase L1
- VTA:
-
Ventral tegmental area
References
Dorsey ER, Elbaz A, Nichols E, Abd-Allah F, Abdelalim A, Adsuar JC, et al. Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet Neurol. 2018;17:939–53.
Poewe W, Seppi K, Tanner CM, Halliday GM, Brundin P, Volkmann J, et al. Parkinson disease. Nat Rev Dis Primer. 2017;3:17013.
Kouli A, Torsney KM, Kuan WL. Parkinson’s disease: etiology, neuropathology, and pathogenesis. In: Stoker TB, Greenland JC, editors. Parkinson’s disease: pathogenesis and clinical aspects [Internet]. Brisbane (AU): Codon Publications; 2018.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30:1591–601.
Picca A, Guerra F, Calvani R, Romano R, Coelho-Júnior HJ, Bucci C, et al. Mitochondrial dysfunction, protein misfolding and neuroinflammation in Parkinson’s disease: roads to biomarker discovery. Biomolecules. 2021;11:1508.
Gerhard A, Pavese N, Hotton G, Turkheimer F, Es M, Hammers A, et al. In vivo imaging of microglial activation with [11 C](R)-PK11195 PET in idiopathic Parkinson’s disease. Neurobiol Dis. 2006;21:404–12.
Höllerhage M. Secondary parkinsonism due to drugs, vascular lesions, tumors, trauma, and other insults. Int Rev Neurobiol. 2019;149:377–418.
Brigo F, Erro R, Marangi A, Bhatia K, Tinazzi M. Differentiating drug-induced parkinsonism from Parkinson’s disease: an update on non-motor symptoms and investigations. Parkinsonism Relat Disord. 2014;20:808–14.
López-Sendón J, Mena MA, de Yébenes JG. Drug-induced parkinsonism. Expert Opin Drug Saf. 2013;12:487–96.
Carlsson A, Lindqvist M, Magnusson T. 3,4-Dihydroxyphenylalanine and 5-hydroxytryptophan as reserpine antagonists. Nature. 1957;180:1200.
Bernstein AI, Stout KA, Miller GW. The vesicular monoamine transporter 2: an underexplored pharmacological target. Neurochem Int. 2014;73:89–97.
Freis ED. Mental depression in hypertensive patients treated for long periods with large doses of reserpine. N Engl J Med. 1954;251:1006–8.
Freis ED, Ari R. Clinical and experimental effects of reserpine in patients with essential hypertension. Ann N Y Acad Sci. 1954;59:45–53.
Kane JM, Smith JM. Tardive dyskinesia: prevalence and risk factors, 1959 to 1979. Arch Gen Psychiatry. 1982;39:473–81.
Fernandes VS, Santos JR, Leão AHFF, Medeiros AM, Melo TG, Izídio GS, et al. Repeated treatment with a low dose of reserpine as a progressive model of Parkinson’s disease. Behav Brain Res. 2012;231:154–63.
Santos JR, Cunha JAS, Dierschnabel AL, Campêlo CLC, Leão AHFF, Silva AF, et al. Cognitive, motor and tyrosine hydroxylase temporal impairment in a model of parkinsonism induced by reserpine. Behav Brain Res. 2013;253:68–77.
Bispo JMM, Melo JEC, Gois AM, Leal PC, Lins LCRF, Souza MF, et al. Sex differences in the progressive model of parkinsonism induced by reserpine in rats. Behav Brain Res. 2019;363:23–9.
Leão AHFF, Meurer YSR, da Silva AF, Medeiros AM, Campêlo CLC, Abílio VC, et al. Spontaneously hypertensive rats (SHR) are resistant to a reserpine-induced progressive model of Parkinson’s disease: differences in motor behavior, tyrosine hydroxylase and α-synuclein expression. Front Aging Neurosci. 2017;9:78.
Leão AHFF, Sarmento-Silva AJ, Santos JR, Ribeiro AM, Silva RH. Molecular, neurochemical, and behavioral hallmarks of reserpine as a model for Parkinson’s disease: new perspectives to a long-standing model: reserpine as a model of Parkinson’s disease. Brain Pathol. 2015;25:377–90.
Lama J, Buhidma Y, Fletcher EJR, Duty S. Animal models of Parkinson’s disease: a guide to selecting the optimal model for your research. Neuronal Signal. 2021;5:NS20210026.
Leal PC, Lins LCRF, de Gois AM, Marchioro M, Santos JR. Commentary: evaluation of models of Parkinson’s disease. Front Neurosci. 2016;10:283.
Gardner DM. Modern antipsychotic drugs: a critical overview. Can Med Assoc J. 2005;172:1703–11.
Ezrin-Waters C, Muller P, Seeman P. Catalepsy induced by morphine or haloperidol: effects of apomorphine and anticholinergic drugs. Can J Physiol Pharmacol. 1976;54:516–9.
Sanberg PR. Haloperidol-induced catalepsy is mediated by postsynaptic dopamine receptors. Nature. 1980;284:472–3.
Kulkarni SK, Bishnoi M, Chopra K. In vivo microdialysis studies of striatal level of neurotransmitters after haloperidol and chlorpromazine administration. Indian J Exp Biol. 2009;47:91–7.
Balijepalli S, Kenchappa RS, Boyd MR, Ravindranath V. Protein thiol oxidation by haloperidol results in inhibition of mitochondrial complex I in brain regions: comparison with atypical antipsychotics. Neurochem Int. 2001;38:425–35.
Ionov ID, Severtsev NN. Somatostatin antagonist potentiates haloperidol-induced catalepsy in the aged rat. Pharmacol Biochem Behav. 2012;103:295–8.
Ionov ID, Severtsev NN. Histamine- and haloperidol-induced catalepsy in aged mice: differential responsiveness to L-DOPA. Psychopharmacology. 2012;223:191–7.
Sharma AK, Gupta S, Patel RK, Wardhan N. Haloperidol-induced parkinsonism is attenuated by varenicline in mice. J Basic Clin Physiol Pharmacol. 2018;29:395–401.
Waku I, Magalhães MS, Alves CO, de Oliveira AR. Haloperidol-induced catalepsy as an animal model for parkinsonism: a systematic review of experimental studies. Eur J Neurosci. 2021;53:3743–67.
Blanchet PJ, Parent M-T, Rompré PH, Lévesque D. Relevance of animal models to human tardive dyskinesia. Behav Brain Funct BBF. 2012;8:12.
Gunne LM, Bárány S. Haloperidol-induced tardive dyskinesia in monkeys. Psychopharmacology. 1976;50:237–40.
Mahmoudi S, Blanchet PJ, Lévesque D. Haloperidol-induced striatal Nur77 expression in a non-human primate model of tardive dyskinesia. Eur J Neurosci. 2013;38:2192–8.
Varty GB, Hodgson RA, Pond AJ, Grzelak ME, Parker EM, Hunter JC. The effects of adenosine A2A receptor antagonists on haloperidol-induced movement disorders in primates. Psychopharmacology. 2008;200:393–401.
Thakur KS, Prakash A, Bisht R, Bansal PK. Beneficial effect of candesartan and lisinopril against haloperidol-induced tardive dyskinesia in rat. J Renin-Angiotensin-Aldosterone Syst JRAAS. 2015;16:917–29.
Senoh S, Witkop B. Non-enzymatic conversions of dopamine to norepinephrine and trihydroxyphenethylamines. J Am Chem Soc. 1959;81:6222–31.
Blandini F, Armentero M-T, Martignoni E. The 6-hydroxydopamine model: news from the past. Parkinsonism Relat Disord. 2008;14(Suppl 2):124–9.
Hernandez-Baltazar D, Zavala-Flores LM, Villanueva-Olivo A. The 6-hydroxydopamine model and parkinsonian pathophysiology: novel findings in an older model. Neurol Engl Ed Elsevier. 2017;32:533–9.
Ungerstedt U. 6-hydroxy-dopamine induced degeneration of central monoamine neurons. Eur J Pharmacol. 1968;5:107–10.
Blum D, Torch S, Lambeng N, Nissou M, Benabid AL, Sadoul R, et al. Molecular pathways involved in the neurotoxicity of 6-OHDA, dopamine and MPTP: contribution to the apoptotic theory in Parkinson’s disease. Prog Neurobiol. 2001;65:135–72.
Schober A. Classic toxin-induced animal models of Parkinson’s disease: 6-OHDA and MPTP. Cell Tissue Res. 2004;318:215–24.
Walsh S, Finn DP, Dowd E. Time-course of nigrostriatal neurodegeneration and neuroinflammation in the 6-hydroxydopamine-induced axonal and terminal lesion models of Parkinson’s disease in the rat. Neuroscience. 2011;175:251–61.
Hernandez-Baltazar D, Zavala-Flores LM, Villanueva-Olivo A. The 6-hydroxydopamine model and parkinsonian pathophysiology: novel findings in an older model. Neurol Barc Spain. 2017;32:533–9.
Kirik D, Rosenblad C, Björklund A. Characterization of behavioral and neurodegenerative changes following partial lesions of the nigrostriatal dopamine system induced by intrastriatal 6-hydroxydopamine in the rat. Exp Neurol. 1998;152:259–77.
Deumens R, Blokland A, Prickaerts J. Modeling Parkinson’s disease in rats: an evaluation of 6-OHDA lesions of the nigrostriatal pathway. Exp Neurol. 2002;175:303–17.
Stott SRW, Barker RA. Time course of dopamine neuron loss and glial response in the 6-OHDA striatal mouse model of Parkinson’s disease. Eur J Neurosci. 2014;39:1042–56.
Sauer H, Oertel WH. Progressive degeneration of nigrostriatal dopamine neurons following intrastriatal terminal lesions with 6-hydroxydopamine: a combined retrograde tracing and immunocytochemical study in the rat. Neuroscience. 1994;59:401–15.
Branchi I, D’Andrea I, Armida M, Cassano T, Pèzzola A, Potenza RL, et al. Nonmotor symptoms in Parkinson’s disease: investigating early-phase onset of behavioral dysfunction in the 6-hydroxydopamine-lesioned rat model. J Neurosci Res. 2008;86:2050–61.
Colucci M, Cervio M, Faniglione M, De Angelis S, Pajoro M, Levandis G, et al. Intestinal dysmotility and enteric neurochemical changes in a Parkinson’s disease rat model. Auton Neurosci Basic Clin. 2012;169:77–86.
Pellegrini C, Ippolito C, Segnani C, Dolfi A, Errede M, Virgintino D, et al. Pathological remodelling of colonic wall following dopaminergic nigrostriatal neurodegeneration. Neurobiol Dis. 2020;139:104821.
Domenici RA, Campos ACP, Maciel ST, Berzuino MB, Hernandes MS, Fonoff ET, et al. Parkinson’s disease and pain: modulation of nociceptive circuitry in a rat model of nigrostriatal lesion. Exp Neurol. 2019;315:72–81.
He X, Yuan W, Li Z, Hou Y, Liu F, Feng J. 6-Hydroxydopamine induces autophagic flux dysfunction by impairing transcription factor EB activation and lysosomal function in dopaminergic neurons and SH-SY5Y cells. Toxicol Lett. 2018;283:58–68.
Nass R, Hall DH, Miller DM, Blakely RD. Neurotoxin-induced degeneration of dopamine neurons in Caenorhabditis elegans. Proc Natl Acad Sci U S A. 2002;99:3264–9.
Hernandez-Baltazar D, Mendoza-Garrido ME, Martinez-Fong D. Activation of GSK-3β and caspase-3 occurs in Nigral dopamine neurons during the development of apoptosis activated by a striatal injection of 6-hydroxydopamine. PLoS ONE. 2013;8:e70951.
Lee Mosley R, Benner EJ, Kadiu I, Thomas M, Boska MD, Hasan K, et al. Neuroinflammation, oxidative stress, and the pathogenesis of Parkinson’s disease. Clin Neurosci Res. 2006;6:261–81.
Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219:979–80.
Nicklas WJ, Youngster SK, Kindt MV, Heikkila RE. IV. MPTP, MPP + and mitochondrial function. Life Sci. 1987;40:721–9.
Przedborski S, Vila M. The 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model: a tool to explore the pathogenesis of Parkinson’s disease. Ann N Y Acad Sci. 2006;991:189–98.
Lofrumento DD, Saponaro C, Cianciulli A, De Nuccio F, Mitolo V, Nicolardi G, et al. MPTP-induced neuroinflammation increases the expression of pro-inflammatory cytokines and their receptors in mouse brain. Neuroimmunomodulation. 2011;18:79–88.
Przedborski S, Jackson-Lewis V, Naini AB, Jakowec M, Petzinger G, Miller R, et al. The parkinsonian toxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP): a technical review of its utility and safety: the parkinsonian toxin MPTP. J Neurochem. 2001;76:1265–74.
Ding F, Luan L, Ai Y, Walton A, Gerhardt GA, Gash DM, et al. Development of a stable, early stage unilateral model of Parkinson’s disease in middle-aged rhesus monkeys. Exp Neurol. 2008;212:431–9.
Schmidt N, Ferger B. Neurochemical findings in the MPTP model of Parkinson’s disease. J Neural Transm. 2001;108:1263–82.
Hu S, Hu M, Liu J, Zhang B, Zhang Z, Zhou FH, et al. Phosphorylation of tau and α-synuclein induced neurodegeneration in MPTP mouse model of Parkinson’s disease. Neuropsychiatr Dis Treat. 2020;16:651–63.
Gelders G, Baekelandt V, Van der Perren A. Linking neuroinflammation and neurodegeneration in Parkinson’s disease. J Immunol Res. 2018;2018:1–12.
Liu M, Bing G. Lipopolysaccharide animal models for Parkinson’s disease. Park Dis. 2011;2011:327089.
Bertani B, Ruiz N. Function and biogenesis of lipopolysaccharides. EcoSal Plus. 2018;8.
Seemann S, Zohles F, Lupp A. Comprehensive comparison of three different animal models for systemic inflammation. J Biomed Sci. 2017;24:60.
Niehaus I. Endotoxin: is it an environmental factor in the cause of Parkinson’s disease? Occup Environ Med. 2003;60:378–8.
Castaño A, Herrera AJ, Cano J, Machado A. Lipopolysaccharide intranigral injection induces inflammatory reaction and damage in nigrostriatal dopaminergic system. J Neurochem. 1998;70:1584–92.
Bing GY, Lu X, Zheng NY, Jin L, Floyd RA, Kim HC. Microglia mediated dopaminergic cell death in the substantia nigra: a new animal model for Parkinson’s disease. Free Radic Biol Med. 1998;25:S44–4.
Herrera AJ, Castaño A, Venero JL, Cano J, Machado A. The single intranigral injection of LPS as a new model for studying the selective effects of inflammatory reactions on dopaminergic system. Neurobiol Dis. 2000;7:429–47.
Deng I, Corrigan F, Zhai G, Zhou X-F, Bobrovskaya L. Lipopolysaccharide animal models of Parkinson’s disease: recent progress and relevance to clinical disease. Brain Behav Immun. 2020;4:100060.
Hunter RL, Cheng B, Choi DY, Liu M, Liu S, Cass WA, et al. Intrastriatal lipopolysaccharide injection induces parkinsonism in C57/B6 mice. J Neurosci Res. 2009;87:1913–21.
Gao HM, Kotzbauer PT, Uryu K, Leight S, Trojanowski JQ, Lee VM-Y. Neuroinflammation and oxidation/nitration of alpha-synuclein linked to dopaminergic neurodegeneration. J Neurosci. 2008;28:7687–98.
Qin L, Liu Y, Wang T, Wei S-J, Block ML, Wilson B, et al. NADPH oxidase mediates lipopolysaccharide-induced neurotoxicity and proinflammatory gene expression in activated microglia. J Biol Chem. 2004;279:1415–21.
Bao LH, Zhang YN, Zhang JN, Gu L, Yang HM, Huang YY, et al. Urate inhibits microglia activation to protect neurons in an LPS-induced model of Parkinson’s disease. J Neuroinflammation. 2018;15:131.
Chen G, Liu J, Jiang L, Ran X, He D, Li Y, et al. Galangin reduces the loss of dopaminergic neurons in an LPS-evoked model of Parkinson’s disease in rats. Int J Mol Sci. 2017;19:12.
Choi DY, Liu M, Hunter RL, Cass WA, Pandya JD, Sullivan PG, et al. Striatal neuroinflammation promotes parkinsonism in rats. PLoS ONE. 2009;4:e5482.
Fu SP, Wang JF, Xue WJ, Liu HM, Liu B, Zeng YL, et al. Anti-inflammatory effects of BHBA in both in vivo and in vitro Parkinson’s disease models are mediated by GPR109A-dependent mechanisms. J Neuroinflammation. 2015;12:9.
He H, Guo WW, Xu RR, Chen XQ, Zhang N, Wu X, et al. Alkaloids from piper longum protect dopaminergic neurons against inflammation-mediated damage induced by intranigral injection of lipopolysaccharide. BMC Complement Altern Med. 2016;16:412.
Hunter R, Ojha U, Bhurtel S, Bing G, Choi DY. Lipopolysaccharide-induced functional and structural injury of the mitochondria in the nigrostriatal pathway. Neurosci Res. 2017;114:62–9.
Hunter RL, Dragicevic N, Seifert K, Choi DY, Liu M, Kim HC, et al. Inflammation induces mitochondrial dysfunction and dopaminergic neurodegeneration in the nigrostriatal system. J Neurochem. 2007;100:1375–86.
Wang J, He C, Wu WY, Chen F, Wu YY, Li WZ, et al. Biochanin A protects dopaminergic neurons against lipopolysaccharide-induced damage and oxidative stress in a rat model of Parkinson’s disease. Pharmacol Biochem Behav. 2015;138:96–103.
Zhang J, Stanton DM, Nguyen XV, Liu M, Zhang Z, Gash D, et al. Intrapallidal lipopolysaccharide injection increases iron and ferritin levels in glia of the rat substantia nigra and induces locomotor deficits. Neuroscience. 2005;135:829–38.
Zhang FX, Xu RS. Juglanin ameliorates LPS-induced neuroinflammation in animal models of Parkinson’s disease and cell culture via inactivating TLR4/NF-κB pathway. Biomed Pharmacother. 2018;97:1011–9.
Choi DY, Zhang J, Bing G. Aging enhances the neuroinflammatory response and alpha-synuclein nitration in rats. Neurobiol Aging. 2010;31:1649–53.
Liu Y, Qin L, Wilson B, Wu X, Qian L, Granholm AC, et al. Endotoxin induces a delayed loss of TH-IR neurons in substantia nigra and motor behavioral deficits. Neurotoxicology. 2008;29:864–70.
Qin L, Wu X, Block ML, Liu Y, Breese GR, Hong JS, et al. Systemic LPS causes chronic neuroinflammation and progressive neurodegeneration. Glia. 2007;55:453–62.
Zheng HF, Yang YP, Hu LF, Wang MX, Wang F, Cao LD, et al. Autophagic impairment contributes to systemic inflammation-induced dopaminergic neuron loss in the midbrain. PLoS ONE. 2013;8:e70472.
Li YH, He Q, Yu J, Liu C, Feng L, Chai Z, et al. Lipoic acid protects dopaminergic neurons in LPS-induced Parkinson’s disease model. Metab Brain Dis. 2015;30:1217–26.
Zhao YF, Qiong-Zhang, Zhang JF, Lou ZY, Zu HB, Wang ZG, et al. The synergy of aging and LPS exposure in a mouse model of Parkinson’s disease. Aging Dis. 2018;9:785.
Nazem A, Sankowski R, Bacher M, Al-Abed Y. Rodent models of neuroinflammation for Alzheimer’s disease. J Neuroinflammation. 2015;12:74.
Roe AD, Staup MA, Serrats J, Sawchenko PE, Rissman RA. Lipopolysaccharide-induced tau phosphorylation and kinase activity - modulation, but not mediation, by corticotropin-releasing factor receptors: LPS-induced tau-P. Eur J Neurosci. 2011;34:448–56.
Valero J, Mastrella G, Neiva I, Sánchez S, Malva JO. Long-term effects of an acute and systemic administration of LPS on adult neurogenesis and spatial memory. Front Neurosci. 2014;8.
Wang LM, Wu Q, Kirk RA, Horn KP, Ebada Salem AH, Hoffman JM, et al. Lipopolysaccharide endotoxemia induces amyloid-β and p-tau formation in the rat brain. Am J Nucl Med Mol Imaging. 2018;8:86–99.
Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 2016;15:1257–72.
Baldi I, Cantagrel A, Lebailly P, Tison F, Dubroca B, Chrysostome V, et al. Association between Parkinson’s disease and exposure to pesticides in southwestern France. Neuroepidemiology. 2003;22:305–10.
Petrovitch H, Ross GW, Abbott RD, Sanderson WT, Sharp DS, Tanner CM, et al. Plantation work and risk of Parkinson disease in a population-based longitudinal study. Arch Neurol. 2002;59:1787–92.
Costello S, Cockburn M, Bronstein J, Zhang X, Ritz B. Parkinson’s disease and residential exposure to maneb and paraquat from agricultural applications in the central valley of California. Am J Epidemiol. 2009;169:919–26.
Tanner CM, Kamel F, Ross GW, Hoppin JA, Goldman SM, Korell M, et al. Rotenone, paraquat, and Parkinson’s disease. Environ Health Perspect. 2011;119:866–72.
Betarbet R, Sherer TB, MacKenzie G, Garcia-Osuna M, Panov AV, Greenamyre JT. Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci. 2000;3:1301–6.
Mader BJ, Pivtoraiko VN, Flippo HM, Klocke BJ, Roth KA, Mangieri LR, et al. Rotenone inhibits autophagic flux prior to inducing cell death. ACS Chem Neurosci. 2012;3:1063–72.
Yuan YH, Yan WF, Sun JD, Huang JY, Mu Z, Chen NH. The molecular mechanism of rotenone-induced α-synuclein aggregation: emphasizing the role of the calcium/GSK3β pathway. Toxicol Lett. 2015;233:163–71.
Fleming S. Behavioral and immunohistochemical effects of chronic intravenous and subcutaneous infusions of varying doses of rotenone. Exp Neurol. 2004;187:418–29.
Inden M, Kitamura Y, Takeuchi H, Yanagida T, Takata K, Kobayashi Y, et al. Neurodegeneration of mouse nigrostriatal dopaminergic system induced by repeated oral administration of rotenone is prevented by 4-phenylbutyrate, a chemical chaperone. J Neurochem. 2007;101:1491–504.
Whitton PS. Inflammation as a causative factor in the aetiology of Parkinson’s disease. Br J Pharmacol. 2007;150:963–76.
Tansey MG, Goldberg MS. Neuroinflammation in Parkinson’s disease: its role in neuronal death and implications for therapeutic intervention. Neurobiol Dis. 2010;37:510–8.
Xiong N, Xiong J, Jia M, Liu L, Zhang X, Chen Z, et al. The role of autophagy in Parkinson’s disease: rotenone-based modeling. Behav Brain Funct. 2013;9:13.
Johnson ME, Bobrovskaya L. An update on the rotenone models of Parkinson’s disease: their ability to reproduce the features of clinical disease and model gene-environment interactions. Neurotoxicology. 2015;46:101–16.
Cicchetti F, Drouin-Ouellet J, Gross RE. Viability of the rotenone model in question. Trends Pharmacol Sci. 2010;31:142–3.
Greenamyre JT, Cannon JR, Drolet R, Mastroberardino PG. Lessons from the rotenone model of Parkinson’s disease. Trends Pharmacol Sci. 2010;31:141–2. author reply 142–143.
Soderstrom K, O’Malley J, Steece-Collier K, Kordower JH. Neural repair strategies for Parkinson’s disease: insights from primate models. Cell Transpl. 2006;15:251–65.
Berry C, La Vecchia C, Nicotera P. Paraquat and Parkinson’s disease. Cell Death Differ. 2010;17:1115–25.
Rappold PM, Cui M, Chesser AS, Tibbett J, Grima JC, Duan L, et al. Paraquat neurotoxicity is mediated by the dopamine transporter and organic cation transporter-3. Proc Natl Acad Sci U S A. 2011;108:20766–71.
Cicchetti F, Lapointe N, Roberge-Tremblay A, Saint-Pierre M, Jimenez L, Ficke BW, et al. Systemic exposure to paraquat and maneb models early Parkinson’s disease in young adult rats. Neurobiol Dis. 2005;20:360–71.
McCormack AL, Thiruchelvam M, Manning-Bog AB, Thiffault C, Langston JW, Cory-Slechta DA, et al. Environmental risk factors and Parkinson’s disease: selective degeneration of nigral dopaminergic neurons caused by the herbicide paraquat. Neurobiol Dis. 2002;10:119–27.
Thiruchelvam M, Brockel BJ, Richfield EK, Baggs RB, Cory-Slechta DA. Potentiated and preferential effects of combined paraquat and maneb on nigrostriatal dopamine systems: environmental risk factors for Parkinson’s disease? Brain Res. 2000;873:225–34.
Thiruchelvam M, McCormack A, Richfield EK, Baggs RB, Tank AW, Di Monte DA, et al. Age-related irreversible progressive nigrostriatal dopaminergic neurotoxicity in the paraquat and maneb model of the Parkinson’s disease phenotype. Eur J Neurosci. 2003;18:589–600.
Manning-Bog AB, McCormack AL, Li J, Uversky VN, Fink AL, Di Monte DA. The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem. 2002;277:1641–4.
Manning-Bog AB, McCormack AL, Purisai MG, Bolin LM. Di Monte DA. α-Synuclein overexpression protects against paraquat-induced neurodegeneration. J Neurosci. 2003;23:3095–9.
Mitra S, Chakrabarti N, Bhattacharyya A. Differential regional expression patterns of α-synuclein, TNF-α, and IL-1β; and variable status of dopaminergic neurotoxicity in mouse brain after paraquat treatment. J Neuroinflammation. 2011;8:163.
Hemmati AA, Hicks R. Increased myofibroblast contractile sensitivity in paraquat pretreated rat lung tissue. Life Sci. 1999;65:2325–32.
Saint-Pierre M, Tremblay M-E, Sik A, Gross RE, Cicchetti F. Temporal effects of paraquat/maneb on microglial activation and dopamine neuronal loss in older rats. J Neurochem. 2006;98:760–72.
Thiruchelvam M, Richfield EK, Baggs RB, Tank AW, Cory-Slechta DA. The nigrostriatal dopaminergic system as a preferential target of repeated exposures to combined paraquat and maneb: implications for Parkinson’s disease. J Neurosci Off J Soc Neurosci. 2000;20:9207–14.
Soares JJ, Rodrigues DT, Gonçalves MB, Lemos MC, Gallarreta MS, Bianchini MC, et al. Paraquat exposure-induced Parkinson’s disease-like symptoms and oxidative stress in Drosophila melanogaster: neuroprotective effect of Bougainvillea glabra Choisy. Biomed Pharmacother Biomedecine Pharmacother. 2017;95:245–51.
Cooper JF, Van Raamsdonk JM. Modeling Parkinson’s disease in C. elegans. J Park Dis. 2018;8:17–32.
Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015;386:896–912.
Blauwendraat C, Nalls MA, Singleton AB. The genetic architecture of Parkinson’s disease. Lancet Neurol Elsevier. 2020;19:170–8.
Pickrell AM, Youle RJ. The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron. 2015;85:257–73.
Schneider SA, Alcalay RN. Neuropathology of genetic synucleinopathies with parkinsonism: review of the literature. Mov Disord. 2017;32:1504–23.
Cooper JF, Machiela E, Dues DJ, Spielbauer KK, Senchuk MM, Van Raamsdonk JM. Activation of the mitochondrial unfolded protein response promotes longevity and dopamine neuron survival in Parkinson’s disease models. Sci Rep. 2017;7:16441.
Cooper JF, Van Raamsdonk JM. Modeling Parkinson’s disease in C. elegans. J Park Dis. 2018;8:17–32.
Park J, Lee SB, Lee S, Kim Y, Song S, Kim S, et al. Mitochondrial dysfunction in Drosophila PINK1 mutants is complemented by parkin. Nature. 2006;441:1157–61.
Greene JC, Whitworth AJ, Kuo I, Andrews LA, Feany MB, Pallanck LJ. Mitochondrial pathology and apoptotic muscle degeneration in Drosophila parkin mutants. Proc Natl Acad Sci U S A. 2003;100:4078–83.
Ge P, Dawson VL, Dawson TM. PINK1 and parkin mitochondrial quality control: a source of regional vulnerability in Parkinson’s disease. Mol Neurodegener. 2020;15:20.
Dawson TM, Ko HS, Dawson VL. Genetic animal models of Parkinson’s disease. Neuron. 2010;66:646–61.
Noda S, Sato S, Fukuda T, Tada N, Uchiyama Y, Tanaka K, et al. Loss of parkin contributes to mitochondrial turnover and dopaminergic neuronal loss in aged mice. Neurobiol Dis. 2020;136:104717.
Yang W, Li S, Li X-J. A CRISPR monkey model unravels a unique function of PINK1 in primate brains. Mol Neurodegener. 2019;14:17.
Xiong Y, Dawson TM, Dawson VL. Models of LRRK2-associated Parkinson’s disease. Adv Neurobiol. 2017;14:163–91.
Wallings R, Manzoni C, Bandopadhyay R. Cellular processes associated with LRRK2 function and dysfunction. FEBS J. 2015;282:2806–26.
Di Maio R, Hoffman EK, Rocha EM, Keeney MT, Sanders LH, De Miranda BR, et al. LRRK2 activation in idiopathic Parkinson’s disease. Sci Transl Med. 2018;10:eaar5429.
Kalia LV, Lang AE, Hazrati L-N, Fujioka S, Wszolek ZK, Dickson DW, et al. Clinical correlations with Lewy body pathology in LRRK2-related Parkinson disease. JAMA Neurol. 2015;72:100–5.
Poulopoulos M, Levy OA, Alcalay RN. The neuropathology of genetic Parkinson’s disease. Mov Disord. 2012;27:831–42.
Saha S, Guillily MD, Ferree A, Lanceta J, Chan D, Ghosh J, et al. LRRK2 modulates vulnerability to mitochondrial dysfunction in Caenorhabditis elegans. J Neurosci. 2009;29:9210–8.
Yao C, El Khoury R, Wang W, Byrd TA, Pehek EA, Thacker C, et al. LRRK2-mediated neurodegeneration and dysfunction of dopaminergic neurons in a Caenorhabditis elegans model of Parkinson’s disease. Neurobiol Dis. 2010;40:73–81.
Saha S, Ash PEA, Gowda V, Liu L, Shirihai O, Wolozin B. Mutations in LRRK2 potentiate age-related impairment of autophagic flux. Mol Neurodegener. 2015;10:26.
Angeles DC, Ho P, Chua LL, Wang C, Yap YW, Ng C, et al. Thiol peroxidases ameliorate LRRK2 mutant-induced mitochondrial and dopaminergic neuronal degeneration in Drosophila. Hum Mol Genet. 2014;23:3157–65.
Bardai FH, Ordonez DG, Bailey RM, Hamm M, Lewis J, Feany MB. Lrrk promotes tau neurotoxicity through dysregulation of actin and mitochondrial dynamics. PLOS Biol. 2018;16:e2006265.
Dodson MW, Zhang T, Jiang C, Chen S, Guo M. Roles of the Drosophila LRRK2 homolog in Rab7-dependent lysosomal positioning. Hum Mol Genet. 2012;21:1350–63.
Beccano-Kelly DA, Kuhlmann N, Tatarnikov I, Volta M, Munsie LN, Chou P et al. Synaptic function is modulated by LRRK2 and glutamate release is increased in cortical neurons of G2019S LRRK2 knock-in mice. Front Cell Neurosci. 2014;8.
Beccano-Kelly DA, Volta M, Munsie LN, Paschall SA, Tatarnikov I, Co K, et al. LRRK2 overexpression alters glutamatergic presynaptic plasticity, striatal dopamine tone, postsynaptic signal transduction, motor activity and memory. Hum Mol Genet. 2015;24:1336–49.
Li X, Patel JC, Wang J, Avshalumov MV, Nicholson C, Buxbaum JD, et al. Enhanced striatal dopamine transmission and motor performance with LRRK2 overexpression in mice is eliminated by familial Parkinson’s disease mutation G2019S. J Neurosci. 2010;30:1788–97.
Li Y, Liu W, Oo TF, Wang L, Tang Y, Jackson-Lewis V, et al. Mutant LRRK2(R1441G) BAC transgenic mice recapitulate cardinal features of Parkinson’s disease. Nat Neurosci. 2009;12:826–8.
Melrose HL, Dächsel JC, Behrouz B, Lincoln SJ, Yue M, Hinkle KM, et al. Impaired dopaminergic neurotransmission and microtubule-associated protein tau alterations in human LRRK2 transgenic mice. Neurobiol Dis. 2010;40:503–17.
Volta M, Beccano-Kelly DA, Paschall SA, Cataldi S, MacIsaac SE, Kuhlmann N, et al. Initial elevations in glutamate and dopamine neurotransmission decline with age, as does exploratory behavior, in LRRK2 G2019S knock-in mice. eLife. 2017;6:e28377.
Yue M, Hinkle KM, Davies P, Trushina E, Fiesel FC, Christenson TA, et al. Progressive dopaminergic alterations and mitochondrial abnormalities in LRRK2 G2019S knock-in mice. Neurobiol Dis. 2015;78:172–95.
Chen CY, Weng YH, Chien KY, Lin KJ, Yeh TH, Cheng YP, et al. (G2019S) LRRK2 activates MKK4-JNK pathway and causes degeneration of SN dopaminergic neurons in a transgenic mouse model of PD. Cell Death Differ. 2012;19:1623–33.
Ramonet D, Daher JPL, Lin BM, Stafa K, Kim J, Banerjee R, et al. Dopaminergic neuronal loss, reduced neurite complexity and autophagic abnormalities in transgenic mice expressing G2019S mutant LRRK2. PLoS ONE. 2011;6:e18568.
Kozina E, Sadasivan S, Jiao Y, Dou Y, Ma Z, Tan H, et al. Mutant LRRK2 mediates peripheral and central immune responses leading to neurodegeneration in vivo. Brain J Neurol. 2018;141:1753–69.
Xiong Y, Neifert S, Karuppagounder SS, Liu Q, Stankowski JN, Lee BD, et al. Robust kinase- and age-dependent dopaminergic and norepinephrine neurodegeneration in LRRK2 G2019S transgenic mice. Proc Natl Acad Sci U S A. 2018;115:1635–40.
Nagakubo D, Taira T, Kitaura H, Ikeda M, Tamai K, Iguchi-Ariga SMM, et al. DJ-1, a novel oncogene which transforms mouse NIH3T3 cells in cooperation withras. Biochem Biophys Res Commun. 1997;231:509–13.
Ariga H, Takahashi-Niki K, Kato I, Maita H, Niki T, Iguchi-Ariga SMM. Neuroprotective function of DJ-1 in Parkinson’s disease. Oxid Med Cell Longev. 2013;2013:1–9.
Aleyasin H, Rousseaux MWC, Marcogliese PC, Hewitt SJ, Irrcher I, Joselin AP, et al. DJ-1 protects the nigrostriatal axis from the neurotoxin MPTP by modulation of the AKT pathway. Proc Natl Acad Sci U S A. 2010;107:3186–91.
Trempe J-F, Fon EA. Structure and function of parkin, PINK1, and DJ-1, the three musketeers of neuroprotection. Front Neurol. 2013;4.
Kim RH, Smith PD, Aleyasin H, Hayley S, Mount MP, Pownall S, et al. Hypersensitivity of DJ-1-deficient mice to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyrindine (MPTP) and oxidative stress. Proc Natl Acad Sci U S A. 2005;102:5215–20.
Bonifati V, Rizzu P, van Baren MJ, Schaap O, Breedveld GJ, Krieger E, et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science. 2003;299:256–9.
Xu C-Y, Kang W-Y, Chen Y-M, Jiang T-F, Zhang J, Zhang L-N, et al. DJ-1 inhibits α-synuclein aggregation by regulating chaperone-mediated autophagy. Front Aging Neurosci. 2017;9:308.
Lopert P, Patel M. Brain mitochondria from DJ-1 knockout mice show increased respiration-dependent hydrogen peroxide consumption. Redox Biol. 2014;2:667–72.
Chen L, Cagniard B, Mathews T, Jones S, Koh HC, Ding Y, et al. Age-dependent motor deficits and dopaminergic dysfunction in DJ-1 null mice. J Biol Chem. 2005;280:21418–26.
Aryal B, Lee Y. Disease model organism for Parkinson disease: Drosophila melanogaster. BMB Rep. 2019;52:250–8.
Ji Y-J, Wang H-L, Yin B-L, Ren X-Y. Down-regulation of DJ-1 augments neuroinflammation via Nrf2/Trx1/NLRP3 axis in MPTP-induced Parkinson’s disease mouse model. Neuroscience. 2020;442:253–63.
Wilkinson KD, Lee KM, Deshpande S, Duerksen-Hughes P, Boss JM, Pohl J. The neuron-specific protein PGP 9.5 is a ubiquitin carboxyl-terminal hydrolase. Science. 1989;246:670–3.
Leroy E, Boyer R, Auburger G, Leube B, Ulm G, Mezey E, et al. The ubiquitin pathway in Parkinson’s disease. Nature. 1998;395:451–2.
Lowe J, McDermott H, Landon M, Mayer RJ, Wilkinson KD. Ubiquitin carboxyl-terminal hydrolase (PGP 9.5) is selectively present in ubiquitinated inclusion bodies characteristic of human neurodegenerative diseases. J Pathol. 1990;161:153–60.
Yasuda T, Nihira T, Ren Y-R, Cao X-Q, Wada K, Setsuie R, et al. Effects of UCH-L1 on α-synuclein over-expression mouse model of Parkinson’s disease. J Neurochem. 2009;108:932–44.
Cerqueira FM, von Stockum S, Giacomello M, Goliand I, Kakimoto P, Marchesan E, et al. A new target for an old DUB: UCH-L1 regulates mitofusin-2 levels, altering mitochondrial morphology, function and calcium uptake. Redox Biol. 2020;37:101676.
Miura H, Oda K, Endo C, Yamazaki K, Shibasaki H, Kikuchi T. Progressive degeneration of motor nerve terminals in GAD mutant mouse with hereditary sensory axonopathy. Neuropathol Appl Neurobiol. 1993;19:41–51.
Oda K, Yamazakit K, Miura H, Shibasaki H, Kikuchi T. Dying back type axonal degeneration of sensory nerve terminals in muscle spindles of the gracile axonal dystrophy (GAD) mutant mouse. Neuropathol Appl Neurobiol. 1992;18:265–81.
Saigoh K, Wang YL, Suh JG, Yamanishi T, Sakai Y, Kiyosawa H, et al. Intragenic deletion in the gene encoding ubiquitin carboxy-terminal hydrolase in gad mice. Nat Genet. 1999;23:47–51.
Setsuie R, Wang Y-L, Mochizuki H, Osaka H, Hayakawa H, Ichihara N, et al. Dopaminergic neuronal loss in transgenic mice expressing the Parkinson’s disease-associated UCH-L1 I93M mutant. Neurochem Int. 2007;50:119–29.
Tran HH, Dang SNA, Nguyen TT, Huynh AM, Dao LinhM, Kamei K, et al. Drosophila ubiquitin c-terminal hydrolase knockdown model of Parkinson’s disease. Sci Rep. 2018;8:4468.
O’Regan G, deSouza R-M, Balestrino R, Schapira AH. Glucocerebrosidase mutations in Parkinson disease. J Park Dis. 2017;7:411–22.
Gan-Or Z, Liong C, Alcalay RN. GBA-associated Parkinson’s disease and other synucleinopathies. Curr Neurol Neurosci Rep. 2018;18:44.
Winfield SL, Tayebi N, Martin BM, Ginns EI, Sidransky E. Identification of three additional genes contiguous to the glucocerebrosidase locus on chromosome 1q21: implications for Gaucher disease. Genome Res. 1997;7:1020–6.
Taguchi YV, Liu J, Ruan J, Pacheco J, Zhang X, Abbasi J, et al. Glucosylsphingosine promotes α-synuclein pathology in mutant GBA-associated Parkinson’s disease. J Neurosci. 2017;37:9617–31.
Blauwendraat C, Reed X, Krohn L, Heilbron K, Bandres-Ciga S, Tan M, et al. Genetic modifiers of risk and age at onset in GBA associated Parkinson’s disease and Lewy body dementia. Brain J Neurol. 2020;143:234–48.
Avenali M, Blandini F, Cerri S. Glucocerebrosidase defects as a major risk factor for Parkinson’s disease. Front Aging Neurosci. 2020;12:97.
Behl T, Kaur G, Fratila O, Buhas C, Judea-Pusta CT, Negrut N, et al. Cross-talks among GBA mutations, glucocerebrosidase, and α-synuclein in GBA-associated Parkinson’s disease and their targeted therapeutic approaches: a comprehensive review. Transl Neurodegener. 2021;10:4.
Goldin E. Gaucher disease and parkinsonism, a molecular link theory. Mol Genet Metab. 2010;101:307–10.
Migdalska-Richards A, Schapira AHV. The relationship between glucocerebrosidase mutations and Parkinson disease. J Neurochem. 2016;139(Suppl 1):77–90.
Farfel-Becker T, Do J, Tayebi N, Sidransky E. Can GBA1-associated Parkinson disease be modeled in the mouse? Trends Neurosci. 2019;42:631–43.
Ginns EI, Mak SK-K, Ko N, Karlgren J, Akbarian S, Chou VP, et al. Neuroinflammation and α-synuclein accumulation in response to glucocerebrosidase deficiency are accompanied by synaptic dysfunction. Mol Genet Metab. 2014;111:152–62.
Li H, Ham A, Ma TC, Kuo S-H, Kanter E, Kim D, et al. Mitochondrial dysfunction and mitophagy defect triggered by heterozygous GBA mutations. Autophagy. 2019;15:113–30.
Migdalska-Richards A, Wegrzynowicz M, Rusconi R, Deangeli G, Di Monte DA, Spillantini MG, et al. The L444P Gba1 mutation enhances alpha-synuclein induced loss of nigral dopaminergic neurons in mice. Brain J Neurol. 2017;140:2706–21.
Abul Khair SB, Dhanushkodi NR, Ardah MT, Chen W, Yang Y, Haque ME. Silencing of glucocerebrosidase gene in Drosophila enhances the aggregation of Parkinson’s disease associated α-synuclein mutant A53T and affects locomotor activity. Front Neurosci. 2018;12:81.
Maor G, Cabasso O, Krivoruk O, Rodriguez J, Steller H, Segal D, et al. The contribution of mutant GBA to the development of Parkinson disease in Drosophila. Hum Mol Genet. 2016;25:2712–27.
Mazzulli JR, Xu Y-H, Sun Y, Knight AL, McLean PJ, Caldwell GA, et al. Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell. 2011;146:37–52.
Do J, McKinney C, Sharma P, Sidransky E. Glucocerebrosidase and its relevance to Parkinson disease. Mol Neurodegener. 2019;14:36.
Blaess S, Ang S-L. Genetic control of midbrain dopaminergic neuron development. Wiley Interdiscip Rev Dev Biol. 2015;4:113–34.
Brodski C, Blaess S, Partanen J, Prakash N. Crosstalk of intercellular signaling pathways in the generation of midbrain dopaminergic neurons in vivo and from stem cells. J Dev Biol. 2019;7:3.
Alavian KN, Jeddi S, Naghipour SI, Nabili P, Licznerski P, Tierney TS. The lifelong maintenance of mesencephalic dopaminergic neurons by Nurr1 and engrailed. J Biomed Sci. 2014;21:27.
Alavian KN, Scholz C, Simon HH. Transcriptional regulation of mesencephalic dopaminergic neurons: the full circle of life and death. Mov Disord. 2008;23:319–28.
Doucet-Beaupré H, Ang S-L, Lévesque M. Cell fate determination, neuronal maintenance and disease state: the emerging role of transcription factors Lmx1a and Lmx1b. FEBS Lett. 2015;589:3727–38.
Fuchs J, Mueller JC, Lichtner P, Schulte C, Munz M, Berg D, et al. The transcription factor PITX3 is associated with sporadic Parkinson’s disease. Neurobiol Aging. 2009;30:731–8.
Nalls MA, Blauwendraat C, Vallerga CL, Heilbron K, Bandres-Ciga S, Chang D, et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 2019;18:1091–102.
Bergman O, Håkansson A, Westberg L, Belin AC, Sydow O, Olson L, et al. Do polymorphisms in transcription factors LMX1A and LMX1B influence the risk for Parkinson’s disease? J Neural Transm Vienna Austria 1996. 2009;116:333–8.
Bergman O, Westberg L, Nilsson L-G, Adolfsson R, Eriksson E. Preliminary evidence that polymorphisms in dopamine-related transcription factors LMX1A, LMX1B and PITX3 are associated with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:1094–7.
Haubenberger D, Reinthaler E, Mueller JC, Pirker W, Katzenschlager R, Froehlich R, et al. Association of transcription factor polymorphisms PITX3 and EN1 with Parkinson’s disease. Neurobiol Aging. 2011;32:302–7.
Laguna A, Schintu N, Nobre A, Alvarsson A, Volakakis N, Jacobsen JK, et al. Dopaminergic control of autophagic-lysosomal function implicates Lmx1b in Parkinson’s disease. Nat Neurosci. 2015;18:826–35.
Chabrat A, Brisson G, Doucet-Beaupré H, Salesse C, Schaan Profes M, Dovonou A, et al. Transcriptional repression of Plxnc1 by Lmx1a and Lmx1b directs topographic dopaminergic circuit formation. Nat Commun. 2017;8:933.
Deng Q, Andersson E, Hedlund E, Alekseenko Z, Coppola E, Panman L, et al. Specific and integrated roles of Lmx1a, Lmx1b and Phox2a in ventral midbrain development. Dev Camb Engl. 2011;138:3399–408.
Salesse C, Charest J, Doucet-Beaupré H, Castonguay A-M, Labrecque S, De Koninck P, et al. Opposite control of excitatory and inhibitory synapse formation by Slitrk2 and Slitrk5 on dopamine neurons modulates hyperactivity behavior. Cell Rep. 2020;30:2374–2386e5.
Yan CH, Levesque M, Claxton S, Johnson RL, Ang SL. Lmx1a and lmx1b function cooperatively to regulate proliferation, specification, and differentiation of midbrain dopaminergic progenitors. J Neurosci. 2011;31:12413–25.
Asbreuk C. CNS expression pattern of Lmx1b and coexpression with ptx genes suggest functional cooperativity in the development of forebrain motor control systems. Mol Cell Neurosci. 2002;21:410–20.
Dai J-X, Hu Z-L, Shi M, Guo C, Ding Y-Q. Postnatal ontogeny of the transcription factor Lmx1b in the mouse central nervous system. J Comp Neurol. 2008;509:341–55.
Zou HL, Su CJ, Shi M, Zhao GY, Li ZY, Guo C, et al. Expression of the LIM-homeodomain gene Lmx1a in the postnatal mouse central nervous system. Brain Res Bull. 2009;78:306–12.
Doucet-Beaupré H, Gilbert C, Profes MS, Chabrat A, Pacelli C, Giguère N, et al. Lmx1a and Lmx1b regulate mitochondrial functions and survival of adult midbrain dopaminergic neurons. Proc Natl Acad Sci U S A. 2016;113:E4387–4396.
Borgkvist A, Puelles E, Carta M, Acampora D, Ang S-L, Wurst W, et al. Altered dopaminergic innervation and amphetamine response in adult Otx2 conditional mutant mice. Mol Cell Neurosci. 2006;31:293–302.
Chung CY, Licznerski P, Alavian KN, Simeone A, Lin Z, Martin E, et al. The transcription factor orthodenticle homeobox 2 influences axonal projections and vulnerability of midbrain dopaminergic neurons. Brain J Neurol. 2010;133:2022–31.
Domanskyi A, Alter H, Vogt MA, Gass P, Vinnikov IA. Transcription factors Foxa1 and Foxa2 are required for adult dopamine neurons maintenance. Front Cell Neurosci. 2014;8:275.
Hwang D-Y, Ardayfio P, Kang UJ, Semina EV, Kim K-S. Selective loss of dopaminergic neurons in the substantia nigra of Pitx3-deficient aphakia mice. Brain Res Mol Brain Res. 2003;114:123–31.
Stott SRW, Metzakopian E, Lin W, Kaestner KH, Hen R, Ang SL. Foxa1 and foxa2 are required for the maintenance of dopaminergic properties in ventral midbrain neurons at late embryonic stages. J Neurosci. 2013;33:8022–34.
van den Munckhof P, Luk KC, Ste-Marie L, Montgomery J, Blanchet PJ, Sadikot AF, et al. Pitx3 is required for motor activity and for survival of a subset of midbrain dopaminergic neurons. Dev Camb Engl. 2003;130:2535–42.
Kadkhodaei B, Ito T, Joodmardi E, Mattsson B, Rouillard C, Carta M, et al. Nurr1 is required for maintenance of maturing and adult midbrain dopamine neurons. J Neurosci. 2009;29:15923–32.
Nordström U, Beauvais G, Ghosh A, Pulikkaparambil Sasidharan BC, Lundblad M, Fuchs J, et al. Progressive nigrostriatal terminal dysfunction and degeneration in the engrailed1 heterozygous mouse model of Parkinson’s disease. Neurobiol Dis. 2015;73:70–82.
Kadkhodaei B, Alvarsson A, Schintu N, Ramsköld D, Volakakis N, Joodmardi E, et al. Transcription factor Nurr1 maintains fiber integrity and nuclear-encoded mitochondrial gene expression in dopamine neurons. Proc Natl Acad Sci U S A. 2013;110:2360–5.
Wurst W, Auerbach AB, Joyner AL. Multiple developmental defects in Engrailed-1 mutant mice: an early mid-hindbrain deletion and patterning defects in forelimbs and sternum. Dev Camb Engl. 1994;120:2065–75.
Baiguera C, Alghisi M, Pinna A, Bellucci A, De Luca MA, Frau L, et al. Late-onset parkinsonism in NFκB/c-Rel-deficient mice. Brain J Neurol. 2012;135:2750–65.
Giguère N, Burke Nanni S, Trudeau LE. On cell loss and selective vulnerability of neuronal populations in Parkinson’s disease. Front Neurol. 2018;9:455.
Surmeier DJ. Determinants of dopaminergic neuron loss in Parkinson’s disease. FEBS J. 2018;285:3657–68.
Haelterman NA, Yoon WH, Sandoval H, Jaiswal M, Shulman JM, Bellen HJ. A mitocentric view of Parkinson’s disease. Annu Rev Neurosci. 2014;37:137–59.
Piccinin E, Sardanelli AM, Seibel P, Moschetta A, Cocco T, Villani G. PGC-1s in the spotlight with Parkinson’s disease. Int J Mol Sci. 2021;22:3487.
Faustini G, Bono F, Valerio A, Pizzi M, Spano P, Bellucci A. Mitochondria and α-synuclein: friends or foes in the pathogenesis of Parkinson’s disease? Genes. 2017;8:E377.
Schapira AHV, Cooper JM, Dexter D, Jenner P, Clark JB, Marsden CD. Mitochondrial complex I deficiency in Parkinson’s disease. Lancet. 1989;333:1269.
Hauser DN, Primiani CT, Langston RG, Kumaran R, Cookson MR. The Polg mutator phenotype does not cause dopaminergic neurodegeneration in DJ-1-deficient mice. eNeuro. 2015;2:ENEURO.0075-14.2015.
Scott L, Karuppagounder SS, Neifert S, Kang BG, Wang H, Dawson VL, et al. The absence of parkin does not promote dopamine or mitochondrial dysfunction in PolgAD257A/D257A mitochondrial mutator mice. J Neurosci. 2022;42:9263–77.
Kim H-W, Choi W-S, Sorscher N, Park HJ, Tronche F, Palmiter RD, et al. Genetic reduction of mitochondrial complex I function does not lead to loss of dopamine neurons in vivo. Neurobiol Aging. 2015;36:2617–27.
González-Rodríguez P, Zampese E, Stout KA, Guzman JN, Ilijic E, Yang B, et al. Disruption of mitochondrial complex I induces progressive parkinsonism. Nature. 2021;599:650–6.
Bartels T, Choi JG, Selkoe DJ. α-Synuclein occurs physiologically as a helically folded tetramer that resists aggregation. Nature. 2011;477:107–10.
Burré J, Sharma M, Südhof TC. Cell biology and pathophysiology of α-synuclein. Cold Spring Harb Perspect Med. 2018;8.
Gómez-Benito M, Granado N, García-Sanz P, Michel A, Dumoulin M, Moratalla R. Modeling Parkinson’s disease with the alpha-synuclein protein. Front Pharmacol. 2020;11:356.
Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M. Alpha-synuclein in filamentous inclusions of Lewy bodies from Parkinson’s disease and dementia with lewy bodies. Proc Natl Acad Sci U S A. 1998;95:6469–73.
Huang M, Wang B, Li X, Fu C, Wang C, Kang X. α-Synuclein: a multifunctional player in exocytosis, endocytosis, and vesicle recycling. Front Neurosci. 2019;13:28.
Liu H, Koros C, Strohäker T, Schulte C, Bozi M, Varvaresos S, et al. A novel SNCA A30G mutation causes familial Parkinsonʼs disease. Mov Disord. 2021;36:1624–33.
Oczkowska A, Kozubski W, Lianeri M, Dorszewska J. Mutations in PRKN and SNCA genes important for the progress of Parkinson’s disease. Curr Genomics. 2013;14:502–17.
Rockenstein E, Mallory M, Hashimoto M, Song D, Shults CW, Lang I, et al. Differential neuropathological alterations in transgenic mice expressing alpha-synuclein from the platelet-derived growth factor and Thy-1 promoters. J Neurosci Res. 2002;68:568–78.
Subramaniam SR, Vergnes L, Franich NR, Reue K, Chesselet M-F. Region specific mitochondrial impairment in mice with widespread overexpression of alpha-synuclein. Neurobiol Dis. 2014;70:204–13.
Watson MB, Richter F, Lee SK, Gabby L, Wu J, Masliah E, et al. Regionally-specific microglial activation in young mice over-expressing human wildtype alpha-synuclein. Exp Neurol. 2012;237:318–34.
Chesselet M-F, Richter F, Zhu C, Magen I, Watson MB, Subramaniam SR. A progressive mouse model of Parkinson’s disease: the Thy1-aSyn (“Line 61”) mice. Neurother J Am Soc Exp Neurother. 2012;9:297–314.
Wegrzynowicz M, Bar-On D, Calo’ L, Anichtchik O, Iovino M, Xia J, et al. Depopulation of dense α-synuclein aggregates is associated with rescue of dopamine neuron dysfunction and death in a new Parkinson’s disease model. Acta Neuropathol (Berl). 2019;138:575–95.
Zarranz JJ, Alegre J, Gómez-Esteban JC, Lezcano E, Ros R, Ampuero I, et al. The new mutation, E46K, of α-synuclein causes parkinson and Lewy body dementia: New α-Synuclein gene mutation. Ann Neurol. 2004;55:164–73.
Emmer KL, Waxman EA, Covy JP, Giasson BI. E46K human α-synuclein transgenic mice develop Lewy-like and Tau pathology associated with age-dependent, detrimental motor impairment. J Biol Chem. 2011;286:35104–18.
Cannon JR, Geghman KD, Tapias V, Sew T, Dail MK, Li C, et al. Expression of human E46K-mutated α-synuclein in BAC-transgenic rats replicates early-stage Parkinson’s disease features and enhances vulnerability to mitochondrial impairment. Exp Neurol. 2013;240:44–56.
Krüger R, Kuhn W, Müller T, Woitalla D, Graeber M, Kösel S, et al. AlaSOPro mutation in the gene encoding α-synuclein in Parkinson’s disease. Nat Genet. 1998;18:106–8.
Piltonen M, Savolainen M, Patrikainen S, Baekelandt V, Myöhänen TT, Männistö PT. Comparison of motor performance, brain biochemistry and histology of two A30P α-synuclein transgenic mouse strains. Neuroscience. 2013;231:157–68.
Ekmark-Lewén S, Lindström V, Gumucio A, Ihse E, Behere A, Kahle PJ, et al. Early fine motor impairment and behavioral dysfunction in (Thy-1)-h[A30P] alpha-synuclein mice. Brain Behav. 2018;8:e00915.
Poon HF, Frasier M, Shreve N, Calabrese V, Wolozin B, Butterfield DA. Mitochondrial associated metabolic proteins are selectively oxidized in A30P alpha-synuclein transgenic mice–a model of familial Parkinson’s disease. Neurobiol Dis. 2005;18:492–8.
Ruiz R, Biea IA, Tabares L, α-Synuclein A30P decreases neurodegeneration and increases synaptic vesicle release probability in CSPα-null mice. Neuropharmacology. 2014;76:106–17.
Chen AY, Wilburn P, Hao X, Tully T. Walking deficits and centrophobism in an α-synuclein fly model of Parkinson’s disease. Genes Brain Behav. 2014;13:812–20.
Mizuno H, Fujikake N, Wada K, Nagai Y. α-Synuclein transgenic drosophila as a model of Parkinson’s disease and related synucleinopathies. Park Dis. 2010;2011:212706.
Perni M, van der Goot A, Limbocker R, van Ham TJ, Aprile FA, Xu CK et al. Comparative studies in the A30P and A53T α-synuclein C. elegans strains to investigate the molecular origins of Parkinson’s disease. Front Cell Dev Biol. 2021;9.
Kuwahara T, Koyama A, Koyama S, Yoshina S, Ren C-H, Kato T, et al. A systematic RNAi screen reveals involvement of endocytic pathway in neuronal dysfunction in α-synuclein transgenic C. elegans. Hum Mol Genet. 2008;17:2997–3009.
Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, et al. Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science. 1997;276:2045–7.
Giasson BI, Duda JE, Quinn SM, Zhang B, Trojanowski JQ, Lee VM-Y. Neuronal α-synucleinopathy with severe movement disorder in mice expressing A53T human α-synuclein. Neuron. 2002;34:521–33.
Mougenot A-LJ, Bencsik A, Nicot S, Vulin J, Morignat E, Verchère J, et al. Transmission of prion strains in a transgenic mouse model overexpressing human A53T mutated α-synuclein. J Neuropathol Exp Neurol. 2011;70:377–85.
Teravskis PJ, Covelo A, Miller EC, Singh B, Martell-Martínez HA, Benneyworth MA, et al. A53T mutant alpha-synuclein induces tau-dependent postsynaptic impairment independently of neurodegenerative changes. J Neurosci. 2018;38:9754–67.
Golbe LI, Lazzarini AM, Duvoisin RC, Iorio GD, Sanges G, Bonavita V, et al. Clinical genetic analysis of Parkinson’s disease in the contursi kindred. Ann Neurol. 1996;40:767–75.
Ramsey CP, Tsika E, Ischiropoulos H, Giasson BI. DJ-1 deficient mice demonstrate similar vulnerability to pathogenic Ala53Thr human -syn toxicity. Hum Mol Genet. 2010;19:1425–37.
Macdonald JA, Chen JL, Masuda-Suzukake M, Schweighauser M, Jaunmuktane Z, Warner T, et al. Assembly of α-synuclein and neurodegeneration in the central nervous system of heterozygous M83 mice following the peripheral administration of α-synuclein seeds. Acta Neuropathol Commun. 2021;9:189.
Sorrentino ZA, Xia Y, Funk C, Riffe CJ, Rutherford NJ, Ceballos Diaz C, et al. Motor Neuron loss and neuroinflammation in a model of α-Synuclein-induced neurodegeneration. Neurobiol Dis. 2018;120:98–106.
Martin LJ, Pan Y, Price AC, Sterling W, Copeland NG, Jenkins NA, et al. Parkinson’s disease alpha-synuclein transgenic mice develop neuronal mitochondrial degeneration and cell death. J Neurosci. 2006;26:41–50.
Malkus KA, Ischiropoulos H. Regional deficiencies in chaperone-mediated autophagy underlie α-synuclein aggregation and neurodegeneration. Neurobiol Dis. 2012;46:732–44.
Chung HK, Ho H-A, Pérez-Acuña D, Lee S-J. Modeling α-Synuclein propagation with preformed Fibril injections. J Mov Disord. 2019;12:139–51.
Luk KC, Kehm V, Carroll J, Zhang B, O’Brien P, Trojanowski JQ, et al. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science. 2012;338:949–53.
Sargent D, Verchère J, Lazizzera C, Gaillard D, Lakhdar L, Streichenberger N, et al. Prion-like’ propagation of the synucleinopathy of M83 transgenic mice depends on the mouse genotype and type of inoculum. J Neurochem. 2017;143:126–35.
Bétemps D, Verchère J, Brot S, Morignat E, Bousset L, Gaillard D, et al. Alpha-synuclein spreading in M83 mice brain revealed by detection of pathological α-synuclein by enhanced ELISA. Acta Neuropathol Commun. 2014;2:29.
Luk KC, Kehm VM, Zhang B, O’Brien P, Trojanowski JQ, Lee VMY. Intracerebral inoculation of pathological α-synuclein initiates a rapidly progressive neurodegenerative α-synucleinopathy in mice. J Exp Med. 2012;209:975–86.
Sorrentino ZA, Xia Y, Funk C, Riffe CJ, Rutherford NJ, Ceballos Diaz C, et al. Motor neuron loss and neuroinflammation in a model of α-synuclein-induced neurodegeneration. Neurobiol Dis. 2018;120:98–106.
Recasens A, Dehay B, Bové J, Carballo-Carbajal I, Dovero S, Pérez-Villalba A, et al. Lewy body extracts from Parkinson disease brains trigger α-synuclein pathology and neurodegeneration in mice and monkeys. Ann Neurol. 2014;75:351–62.
Okuda S, Uemura N, Sawamura M, Taguchi T, Ikuno M, Uemura MT, et al. Rapid induction of dopaminergic neuron loss accompanied by Lewy body-like inclusions in A53T BAC-SNCA transgenic mice. Neurotherapeutics. 2022;19(1):289–304.
Wang X, Becker K, Levine N, Zhang M, Lieberman AP, Moore DJ, et al. Pathogenic alpha-synuclein aggregates preferentially bind to mitochondria and affect cellular respiration. Acta Neuropathol Commun. 2019;7:41.
Guiney SJ, Adlard PA, Lei P, Mawal CH, Bush AI, Finkelstein DI, et al. Fibrillar α-synuclein toxicity depends on functional lysosomes. J Biol Chem. 2020;295:17497–513.
Masuda-Suzukake M, Nonaka T, Hosokawa M, Oikawa T, Arai T, Akiyama H, et al. Prion-like spreading of pathological α-synuclein in brain. Brain. 2013;136:1128–38.
Polinski NK. A summary of phenotypes observed in the in vivo rodent alpha-synuclein preformed fibril model. J Park Dis. 2021;11:1555–67.
Ahn EH, Kang SS, Liu X, Chen G, Zhang Z, Chandrasekharan B, et al. Initiation of Parkinson’s disease from gut to brain by δ-secretase. Cell Res. 2020;30:70–87.
Challis C, Hori A, Sampson TR, Yoo BB, Challis RC, Hamilton AM, et al. Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice. Nat Neurosci. 2020;23:327–36.
Kim S, Kwon S-H, Kam T-I, Panicker N, Karuppagounder SS, Lee S, et al. Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson’s disease. Neuron. 2019;103:627–641e7.
Earls RH, Menees KB, Chung J, Barber J, Gutekunst C-A, Hazim MG, et al. Intrastriatal injection of preformed alpha-synuclein fibrils alters central and peripheral immune cell profiles in non-transgenic mice. J Neuroinflammation. 2019;16:250.
Mahul-Mellier A-L, Burtscher J, Maharjan N, Weerens L, Croisier M, Kuttler F, et al. The process of Lewy body formation, rather than simply α-synuclein fibrillization, is one of the major drivers of neurodegeneration. Proc Natl Acad Sci U S A. 2020;117:4971–82.
Polinski NK, Volpicelli-Daley LA, Sortwell CE, Luk KC, Cremades N, Gottler LM, et al. Best practices for generating and using alpha-synuclein pre-formed fibrils to model Parkinson’s disease in rodents. J Park Dis. 2018;8:303–22.
van Ham TJ, Thijssen KL, Breitling R, Hofstra RMW, Plasterk RHA, Nollen EAA. C. elegans model identifies genetic modifiers of α-synuclein inclusion formation during aging. PLoS Genet. 2008;4:e1000027.
Cooper AA, Gitler AD, Cashikar A, Haynes CM, Hill KJ, Bhullar B, et al. Alpha-synuclein blocks ER-Golgi traffic and Rab1 rescues neuron loss in Parkinson’s models. Science. 2006;313:324–8.
Cooper JF, Spielbauer KK, Senchuk MM, Nadarajan S, Colaiácovo MP, Van Raamsdonk JM. α-synuclein expression from a single copy transgene increases sensitivity to stress and accelerates neuronal loss in genetic models of Parkinson’s disease. Exp Neurol. 2018;310:58–69.
Feany MB, Bender WW. A Drosophila model of Parkinson’s disease. Nature. 2000;404:394–8.
Auluck PK. Chaperone suppression of alpha -synuclein toxicity in a Drosophila model for Parkinson’s disease. Science. 2002;295:865–8.
Ordonez DG, Lee MK, Feany MB. α-synuclein induces mitochondrial dysfunction through spectrin and the actin cytoskeleton. Neuron. 2018;97:108–124e6.
Lu J, Sun F, Ma H, Qing H, Deng Y. Comparison between α-synuclein wild-type and A53T mutation in a progressive Parkinson’s disease model. Biochem Biophys Res Commun. 2015;464:988–93.
Lo Bianco C, Ridet J-L, Schneider BL, Deglon N, Aebischer P. Alpha-synucleinopathy and selective dopaminergic neuron loss in a rat lentiviral-based model of Parkinson’s disease. Proc Natl Acad Sci U S A. 2002;99:10813–8.
Kirik D, Rosenblad C, Burger C, Lundberg C, Johansen TE, Muzyczka N, et al. Parkinson-like neurodegeneration induced by targeted overexpression of alpha-synuclein in the nigrostriatal system. J Neurosci. 2002;22:2780–91.
Ip CW, Klaus L-C, Karikari AA, Visanji NP, Brotchie JM, Lang AE, et al. AAV1/2-induced overexpression of A53T-α-synuclein in the substantia nigra results in degeneration of the nigrostriatal system with Lewy-like pathology and motor impairment: a new mouse model for Parkinson’s disease. Acta Neuropathol Commun. 2017;5:11.
Van der Perren A, Van den Haute C, Baekelandt V. Viral vector-based models of Parkinson’s disease. Curr Top Behav Neurosci. 2015;22:271–301.
Recasens A, Dehay B. Alpha-synuclein spreading in Parkinson’s disease. Front Neuroanat. 2014;8:159.
Koprich JB, Johnston TH, Reyes MG, Sun X, Brotchie JM. Expression of human A53T alpha-synuclein in the rat substantia nigra using a novel AAV1/2 vector produces a rapidly evolving pathology with protein aggregation, dystrophic neurite architecture and nigrostriatal degeneration with potential to model the pathology of Parkinson’s disease. Mol Neurodegener. 2010;5:43.
Koprich JB, Johnston TH, Huot P, Reyes MG, Espinosa M, Brotchie JM. Progressive neurodegeneration or endogenous compensation in an animal model of Parkinson’s disease produced by decreasing doses of alpha-synuclein. PLoS ONE. 2011;6:e17698.
Dehay B, Fernagut P-O. Alpha-synuclein-based models of Parkinson’s disease. Rev Neurol (Paris). 2016;172:371–8.
Huntington TE, Srinivasan R. Adeno-associated virus expression of α-synuclein as a tool to model Parkinson’s disease: current understanding and knowledge gaps. Aging Dis. 2021;12:1120–37.
Volpicelli-Daley LA, Kirik D, Stoyka LE, Standaert DG, Harms AS. How can rAAV-α-synuclein and the fibril α-synuclein models advance our understanding of Parkinson’s disease? J Neurochem. 2016;139:131–55.
Decressac M, Mattsson B, Lundblad M, Weikop P, Björklund A. Progressive neurodegenerative and behavioural changes induced by AAV-mediated overexpression of α-synuclein in midbrain dopamine neurons. Neurobiol Dis. 2012;45:939–53.
Kirik D, Annett LE, Burger C, Muzyczka N, Mandel RJ, Björklund A. Nigrostriatal alpha-synucleinopathy induced by viral vector-mediated overexpression of human alpha-synuclein: a new primate model of Parkinson’s disease. Proc Natl Acad Sci U S A. 2003;100:2884–9.
Eslamboli A, Romero-Ramos M, Burger C, Bjorklund T, Muzyczka N, Mandel RJ, et al. Long-term consequences of human alpha-synuclein overexpression in the primate ventral midbrain. Brain. 2007;130:799–815.
Yang W, Wang G, Wang C-E, Guo X, Yin P, Gao J, et al. Mutant alpha-synuclein causes age-dependent neuropathology in monkey brain. J Neurosci. 2015;35:8345–58.
Di Maio R, Barrett PJ, Hoffman EK, Barrett CW, Zharikov A, Borah A, et al. α-Synuclein binds to TOM20 and inhibits mitochondrial protein import in Parkinson’s disease. Sci Transl Med. 2016. https://doi.org/10.1126/scitranslmed.aaf3634.
McKinnon C, De Snoo ML, Gondard E, Neudorfer C, Chau H, Ngana SG, et al. Early-onset impairment of the ubiquitin-proteasome system in dopaminergic neurons caused by α-synuclein. Acta Neuropathol Commun. 2020;8:17.
Yamada M, Iwatsubo T, Mizuno Y, Mochizuki H. Overexpression of alpha-synuclein in rat substantia nigra results in loss of dopaminergic neurons, phosphorylation of alpha-synuclein and activation of caspase-9: resemblance to pathogenetic changes in Parkinson’s disease. J Neurochem. 2004;91:451–61.
Chung CY, Koprich JB, Siddiqi H, Isacson O. Dynamic changes in presynaptic and axonal transport proteins combined with striatal neuroinflammation precede dopaminergic neuronal loss in a rat model of AAV alpha-synucleinopathy. J Neurosci. 2009;29:3365–73.
Sanchez-Guajardo V, Febbraro F, Kirik D, Romero-Ramos M. Microglia acquire distinct activation profiles depending on the degree of alpha-synuclein neuropathology in a rAAV based model of Parkinson’s disease. PLoS ONE. 2010;5:e8784.
Theodore S, Cao S, McLean PJ, Standaert DG. Targeted overexpression of human alpha-synuclein triggers microglial activation and an adaptive immune response in a mouse model of Parkinson disease. J Neuropathol Exp Neurol. 2008;67:1149–58.
Ulusoy A, Decressac M, Kirik D, Björklund A. Viral vector-mediated overexpression of α-synuclein as a progressive model of Parkinson’s disease. Prog Brain Res. 2010;184:89–111.
Bérard M, Sheta R, Malvaut S, Rodriguez-Aller R, Teixeira M, Idi W, et al. A light-inducible protein clustering system for in vivo analysis of α-synuclein aggregation in Parkinson disease. PLOS Biol. 2022;20:e3001578.
Lees AJ, Selikhova M, Andrade LA, Duyckaerts C. The black stuff and Konstantin Nikolaevich Tretiakoff. Mov Disord. 2008;23:777–83.
Zecca L, Fariello R, Riederer P, Sulzer D, Gatti A, Tampellini D. The absolute concentration of nigral neuromelanin, assayed by a new sensitive method, increases throughout the life and is dramatically decreased in Parkinson’s disease. FEBS Lett. 2002;510:216–20.
Nagatsu T, Nakashima A, Watanabe H, Ito S, Wakamatsu K. Neuromelanin in Parkinson’s disease: tyrosine hydroxylase and tyrosinase. Int J Mol Sci. 2022;23:4176.
Zucca FA, Segura-Aguilar J, Ferrari E, Muñoz P, Paris I, Sulzer D, et al. Interactions of iron, dopamine and neuromelanin pathways in brain aging and Parkinson’s disease. Prog Neurobiol. 2017;155:96–119.
Wilms H, Rosenstiel P, Sievers J, Deuschl G, Zecca L, Lucius R. Activation of microglia by human neuromelanin is NF-κB‐dependent and involves p38 mitogen‐activated protein kinase: implications for Parkinson’s disease. FASEB J. 2003;17:1–20.
Zhang W. Human neuromelanin an endogenous microglial activator for dopaminergic neuron death. Front Biosci. 2013;E5:1–11.
Viceconte N, Burguillos MA, Herrera AJ, De Pablos RM, Joseph B, Venero JL. Neuromelanin activates proinflammatory microglia through a caspase-8-dependent mechanism. J Neuroinflammation. 2015;12:5.
Carballo-Carbajal I, Laguna A, Romero-Giménez J, Cuadros T, Bové J, Martinez-Vicente M, et al. Brain tyrosinase overexpression implicates age-dependent neuromelanin production in Parkinson’s disease pathogenesis. Nat Commun. 2019;10:973.
Vila M. Neuromelanin, aging, and neuronal vulnerability in Parkinson’s disease. Mov Disord. 2019;34:1440–51.
Xiong Y, Yu J. Modeling Parkinson’s disease in Drosophila: what have we learned for dominant traits? Front Neurol. 2018;9:228.
Slanzi A, Iannoto G, Rossi B, Zenaro E, Constantin G. In vitro models of neurodegenerative diseases. Front Cell Dev Biol. 2020;8:328.
Smits LM, Schwamborn JC. Midbrain organoids: a new tool to investigate Parkinson’s disease. Front Cell Dev Biol. 2020;8:359.
Acknowledgements
Not applicable.
Funding
This work was supported by a grant to ML. from Canadian Institutes of Health Research. ML. also receives a salary award from the Fonds de recherche du Québec in partnership with Parkinson Quebec.
Author information
Authors and Affiliations
Contributions
AD: writing, review and editing. CB: writing, review and editing. VSL: writing, review and editing. CG: writing, review and editing. MRP 3rd: review and editing. ML: funding acquisition, writing, review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dovonou, A., Bolduc, C., Soto Linan, V. et al. Animal models of Parkinson’s disease: bridging the gap between disease hallmarks and research questions. Transl Neurodegener 12, 36 (2023). https://doi.org/10.1186/s40035-023-00368-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40035-023-00368-8