Abstract
Background
While tailored information might have the potential to motivate stroke survivors to make essential lifestyle changes and improve long-term outcomes, how this varies among different stroke populations is not yet fully understood.
Method
From November 2022 to May 2023, stroke survivors in the UK, who were clinically stable, participated in a community-based, descriptive cross-sectional study. Participants rated several information themes on a Likert scale from one to five, indicating the relevance of each information group to them. Data were analysed using Wilcoxon and chi-squared tests on SPSS. Descriptive statistics were employed for examining the preferred information delivery method, timing, personnel, and frequency.
Results
Seventy survivors, with an average age of 67 ± 19 (61% males), were recruited. Survivors emphasised the importance of symptoms, risk factors, and recovery information during hospital stay, while medication and lifestyle change information were more significant in the community. Subgroup analysis revealed distinct patterns: First-time stroke survivors highlighted the importance of social and financial support (acute phase median Likert score 3, chronic phase median Likert score 4; p < 0.01), while those with prior strokes emphasised information on driving and working after stroke (acute phase median Likert score 4, chronic phase median Likert score 3; p < 0.05). Survivors recruited after six months of stroke prioritised knowledge of carer support in the community (acute phase median Likert score 3.5, chronic phase median Likert score 4; p < 0.01).
Conclusion
Survivors’ information needs differ depending on factors such as the recovery phase, type of stroke, time since diagnosis, and the presence of a previous stroke. Considering these factors is essential when developing or providing information to stroke survivors.
Similar content being viewed by others
Text box 1: Contributions to the literature |
|---|
• This report uncovers new insights into how different groups of stroke survivors have unique information needs. |
• We noticed a pattern in how survivors seek information about strokes, which is in line with theories on how individuals adapt socially following life-threatening events. |
• When providing information to stroke survivors, it’s important to consider five key factors: the type of information, how it’s delivered, when it’s delivered, how often it’s delivered, and who delivers it. |
Introduction
It is estimated that adhering to necessary long-term management and healthy behaviour changes could prevent more than 50% of strokes [1]. However, the patient’s willpower and beliefs, together with their personal, social, and economic status would often influence these modifications [2, 3]. Providing relevant information about the benefits of leading a healthy lifestyle and the consequences of not making changes is essential [4]. Hence, the concept of patients’ information needs emerged to deliver pertinent information, motivating patients to adopt necessary healthy behaviour [5].
In stroke, the needed information vary with time due to the fluctuating emotional status experienced postdiagnosis [6, 7]. Therefore, considering the variation in stroke survivors’ information needs throughout their recovery is important. Some studies have shown differences in what survivors’ information prioritises, such as rehabilitation and preventing recurrence in the acute phase, while focusing on financial support in the long term [8,9,10,11]. However, the literature lacks a thorough exploration of the impact of time on stroke information needs and how this differs across various stroke populations. This study aims to investigate stroke survivors’ information needs during different recovery stages and evaluate appropriate approaches to deliver them.
Methods
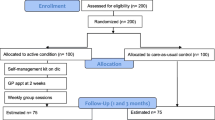
This study was descriptive, cross-sectional, observational research utilising a semistructured questionnaire (online supplement 1) and was approved by the University Ethics Committee (1901-22-AH-CMS) in October 2022. Recruitment took place from November 2022 to May 2023.
The questionnaire’s development began with a literature search to collect survivor-expressed information needs. Fourteen publications were reviewed, identifying 85 distinct information needs (online supplement 2). Using a pile-sorting method [12], these needs were categorised into ten groups. The categories were incorporated into our questionnaire, where participants rated these ten groups on a Likert scale from 1 to 5 based on the relevance of each group to them, covering two recovery phases: during hospital stay and in the community. Additionally, the questionnaire explored participants’ preferences for information delivery methods, desired healthcare professionals (HCPs) responsible for providing information, timing of delivery, and frequency of information dissemination. Open-ended questions were included to further explore participants’ views.
The first draft of the questionnaire underwent review by a stroke consultant and a stroke survivor focus group comprising 30 stroke survivors and carers. Their feedback was used to refine the questionnaire. Subsequently, pilot testing was conducted, involving nine stroke survivors identified from online stroke support groups in the UK, resulting in slight changes in the final version.
The study recruited participants who had experienced either a stroke (ischaemic or haemorrhagic) or a transient ischaemic attack (TIA), were currently living in the UK, and were clinically stable. Exclusions comprised individuals under 18 years old, those unable to communicate effectively in English, and those lacking mental capacity.
After completing the pilot testing phase, recruitment primarily occurred through in-person methods, utilising a paper-based questionnaire. Participants eligibility was determined by the stroke consultant from the stroke outpatient clinic at the Countess of Chester Hospital and the stroke rehabilitation centre at Ellesmere Port Hospital in northwest England, who provided information about the questionnaire, along with a poster featuring a quick response code for accessing the consent form and the questionnaire. Interested participants filled out the questionnaire anonymously. Additionally, suitable participants were invited to participate in the study through online UK-based stroke survivors’ support groups. The questionnaire included screening questions at the beginning to assess the eligibility of individuals identified online.
SPSS 26 was utilised for quantitative analysis. Initially, descriptive statistics were conducted. Subsequently, the normality of the independent variables distribution (the information needs Likert scale) guided the selection of statistical tests. The median of the Likert scale, ranging from one to five, was calculated and compared for each information group. For subgroup analysis, data was divided using SPSS into the relevant subgroups and the Likert scale median was compared before and after discharge using the Wilcoxon test. P values below 0.05 were deemed significant. The relative importance index (RII) for each IN category was calculated. The RII is used to weigh the different factors based on their Likert score value [13], and it is calculated using the equation: Σ𝑤/𝐴𝑁 = 5𝑛5 + 4𝑛4 + 3𝑛3 + 2𝑛2 + 1𝑛1 / 5𝑁, where n5 represents the number of participants who chose “extremely important” for one option (n4, n3, n2, n1 follow the same pattern) and N represents the total number of participants [14]. The RII has a range from 0 to 1, and a rank could be generated based on each category value. Missing data were excluded from the analysis.
Content analysis was conducted to analyse the qualitative data [15]. Responses were reviewed multiple times, coded, and organised into themes. The first author (A.H) and the third author (L.D) independently followed the same procedure to perform the analysis. A consensus meeting was held in June 2023 to finalise the outcomes.
Results
The study included 70 participants with a median age of 67 ± 19 years, among whom 61.4% were male. Ischaemic stroke cases comprised 54.3% of the sample, with the majority (74.3%) being first-time stroke survivors. Additionally, 62.9% of participants had experienced their stroke within the last six months. Table 1 presents an overview of the baseline characteristics.
Statistically significant differences were noted between recovery phases in terms of Information needs. During the hospital stay, the emphasis was on understanding risk factors and the anticipated recovery. However, upon transitioning to the community, the focus shifted to knowledge about medications, access to carer and social support, financial aid, and insurance with a p value < 0.05, as depicted in Table 2.
The ranking of the information needs based on the RII values showed that knowledge of risk factors, recovery, and symptoms were the top three information needs during hospitalisation, respectively. However, knowledge of medications, lifestyle modifications, and risk factors became the top three in the community, as shown in Fig. 1.
Subgroup analysis was conducted by dividing the dataset based on the underlying diagnosis (stroke or TIA), time since diagnosis (< 6 months or > 6 months), and recurrence (first time or previous stroke). The median of the Likert scale (ranging from one to five) for each category was compared in both the chronic and acute phases. Statistically significant differences among subgroups were summarised in Table 3. Significant differences were found based on the underlying diagnosis. Stroke survivors prioritised knowledge about recovery during hospitalisation, whereas medication and social support information took precedence in the community setting. Those recruited six months postdiagnosis emphasised the importance of understanding social, financial, and carer support after discharge. Additionally, individuals with a history of stroke highlighted the significance of information regarding driving and working poststroke in acute settings.
Participants reported that in-person discussions were the most preferred method of information delivery (74% of the sample), followed by written materials (50%) and the Internet (24%). Surprisingly, only 41.4% of respondents reported being offered take-home written materials before discharge. The most preferred timing for information delivery was during the rehabilitation phase, selected by 53% of the sample. Specialist neurologists were the top choice for discussing stroke-related information (58.5%), followed by general practitioners (GPs) and nursing staff (preferred by 43% and 30%, respectively). Interestingly, respondents indicated in open-ended questions the important role of physiotherapists in answering their questions about the different aspects of stroke during physiotherapy sessions. A majority of stroke survivors (61.4%) expressed the desire for multiple discussions about stroke information, whether it occurs every three, six, or twelve months.
Finally, in open-ended questions regarding the design of written materials, participants most frequently suggested including rehabilitation techniques and exercises. Other suggestions involved adding pictures, using larger font sizes, and presenting the content in an optimistic way, as outlined in Table 4.
Discussion
Understanding stroke survivors’ information needs throughout their recovery is vital to ensure active involvement with the management plan, especially since newly diagnosed survivors frequently express their limited understanding of the condition [16]. In our analysis, different information needs emerged across recovery phases. During hospitalisation, participants focused on risk factors and recovery information, while in the community phase, participants prioritised medications, social support, finances, and insurance. There were several differences between the needs during hospitalisation and after discharge for stroke survivors, where knowing the future risk and potential functional restoration was far more important in the hospitalisation phase, shifting to the knowledge of daily medications and available support in the community. A similar pattern was observed in previous studies [7, 8]. This difference is consistent with the theory of cognitive adaptation to life-threatening events [17], where initially there is a focus on understanding the event’s causes, its impact, and the likelihood of recurrence. This emphasis transitions to concerns about self-adjustment and managing daily life during the long-term phase.
Differences based on stroke type (stroke or TIA) may stem from the complexities of stroke recovery, often involving functional complications that necessitate long-term support [18]. Individuals recovering from stroke express concerns about available support, contrasting the potential for full recovery often observed in TIA survivors. Time since stroke diagnosis also influenced survivors’ information needs, as newly diagnosed individuals inquired about risk factors and recovery due to uncertainties surrounding long-term complications [19]. Those with over a 6-month diagnosis focused on themes related to available support, considering the potential decline in function and quality of life in the long term after stroke [20]. Recurrence further shaped concerns, with first-time stroke survivors focusing on preventing future episodes, while those with previous strokes emphasised moving forward, including aspects such as working and driving after stroke. These findings resonate with the theory of psychological adjustment in long-term diseases, progressing from initial stress and uncertainty about illness to eventual acceptance and emotional equilibrium [21].
The preferred method for delivering information involved a combination of verbal and written materials. Verbal communication allows for personalised information sharing, while written materials offer the advantage of revisiting information after discharge. Our sample suggested developing pictorial materials with large prints, which was recommended in the literature to aid information retention in the long term [22, 23]. Additionally, our study indicated an optimistic approach to presenting information, considering that some stroke survivors experienced despair and helplessness with current stroke-related written materials [24]. Participants proposed delaying information delivery until the rehabilitation phase, which acknowledges the challenge of retaining information in the early stages poststroke [25].
Specialist neurologists, GPs, and nurses emerged as the preferred healthcare professionals for discussing stroke-related matters. Although physiotherapists were not among the most frequently selected HCPs, their role in information-sharing is important due to the time they spend facilitating and applying rehabilitation techniques. This suggests a broader involvement in survivors’ education beyond merely performing exercise therapy. Finally, reiterating information was deemed necessary as survivors’ information needs evolve with time.
However, this study had limitations. Firstly, recruitment from a specific area will limit the generalisability of the outcomes, as other local and international facilities have different approaches and contact points from the one shown in our study. Secondly, the exclusion of participants with cognitive impairment. Conducting in-depth interviews might have offered deeper insights into the reasons behind the subgroup differences.
To conclude, post-stroke information-seeking displays two discernible patterns: during the acute phase, the focus is on reducing stroke recurrence and restoring function. However, in the chronic phase, attention shifts towards adapting to the new life poststroke, as outlined in Fig. 2. This could help healthcare professionals identify the most appropriate information based on the recovery phase, type, and time elapsed since diagnosis.
Accordingly, an optimal approach for stroke survivors involves tailoring information delivery based on these distinct patterns while considering the different stroke populations and emphasising suitable delivery methods and timing. Such an approach could enable healthcare providers to empower survivors to manage their condition more effectively. Further research is needed to investigate whether providing this tailored information could improve stroke survivors’ long-term outcomes.
Data availability
The data supporting the findings of this study is available from the corresponding author upon reasonable request.
References
George MG, Fischer L, Koroshetz W, et al. CDC grand rounds: public health strategies to prevent and treat strokes. MMWR Morb Mortal Wkly Rep. 2017;66:479–81.
Amdie FZ, Sawhney M, Woo K. The weakness of will: the role of free will in treatment adherence. Patient Prefer Adherence. 2022;16:1131–9.
Skaar E, Ranhoff AH, Nordrehaug JE et al. Conditions for autonomous choice: a qualitative study of older adults’ experience of decision-making in TAVR. J Geriatr Cardiol; 14. Epub ahead of print 2017. https://doi.org/10.11909/j.issn.1671-5411.2017.01.007.
Leung AWY, Chan RSM, Sea MMM, Woo J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. Int J Environ Res Public Health [Internet]. 2017 [cited 2024 Mar 11];14(8):922. https://doi.org/10.3390/ijerph14080922.
Gesme D, Wiseman M. How to implement change in practice. J Oncol Pract. 2010;6:257–9.
Chohan SA, Venkatesh PK, How CH. Long-term complications of stroke and secondary prevention: an overview for primary care physicians. Singap Med J. 2019;60:616–20.
Lewis KS. Emotional adjustment to a chronic illness. Lippincotts Prim Care Pract; 2, https://pubmed.ncbi.nlm.nih.gov/9451198/ (1998, accessed 14 November 2023).
Davoody N, Koch S, Krakau I, et al. Post-discharge stroke patients’ information needs as input to proposing patient-centred eHealth services. BMC Med Inf Decis Mak. 2016;16:Epubaheadofprint. https://doi.org/10.1186/s12911-016-0307-2.
Garrett D, Cowdell F. Information needs of patients and carers following stroke: stroke is common and a major cause of disability, yet those who experience it, and their carers, are often denied information that could help them. Dawne Garrett and Fiona Cowdell consider the information needs of patients and carers at different intervals post stroke. Nurs Older People. 2005;17:14–6.
Hoffmann T, Mckenna K, Worrall L, et al. Evaluating current practice in the provision of written information to stroke patients and their carers. Int J Ther Rehabil. 2004;11:303–10.
Hanger HC, Walker G, Paterson LA, et al. What do patients and their carers want to know about stroke? A two-year follow-up study. Clin Rehabil. 1998;12:45–52.
Quintiliani LM, Campbell MK, Haines PS, Webber KH. The use of the pile sort method in identifying groups of healthful lifestyle behaviors among female community college students. J Am Diet Assoc. 2008;108(9):1503–7. https://doi.org/10.1016/j.jada.2008.06.428.
Azman NS, Ramli MZ, Razman R, et al. Relative importance index (RII) in ranking of quality factors on industrialised building system (IBS) projects in Malaysia. APPLIED PHYSICS OF CONDENSED MATTER (APCOM 2019). AIP Publishing; 2019.
Tholibon DA, Md Nujid M, Mokhtar H, Rahim JA, Aziz NFA, Tarmizi AAA. Relative importance index (RII) in ranking the factors of employer satisfaction towards industrial training students. Int J Asian Educ. 2021;2(4):493–503. https://doi.org/10.46966/ijae.v2i4.187.
Cavanagh S. Content analysis: concepts, methods and applications: content analysis is a flexible methodology that is particularly useful to nurse researchers, asserts Stephen Cavanagh. Nurse Res. 1997;4:5–16.
Abrahamson V, Wilson PM. How unmet are unmet needs post-stroke? A policy analysis of the six-month review. BMC Health Serv Res; 19. Epub ahead of print 2019. https://doi.org/10.1186/s12913-019-4210-2.
Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol. 1983;38:1161–73.
Hughes AK, Cummings CE. Grief and loss associated with stroke recovery: a qualitative study of stroke survivors and their spousal caregivers. J Patient Exp. 2020;7:1219–26.
Engel K, Homsi M, Suzuki R, et al. Newly diagnosed patients with inflammatory bowel disease: the relationship between perceived psychological support, health-related quality of life, and disease activity. Health Equity. 2021;5:42–8.
Schneider S, Taba N, Saapar M, et al. Determinants of long-term health-related quality of life in young ischemic stroke patients. J Stroke Cerebrovasc Dis. 2021;30:105499.
Carroll S, Moon Z, Hudson J, et al. An evidence-based theory of psychological adjustment to long-term physical health conditions: applications in clinical practice. Psychosom Med. 2022;84:547–59.
Kessels RPC. Patients’ memory for medical information. J R Soc Med. 2003;96:219–22.
Halamish V, Nachman H, Katzir T. The effect of font size on children’s memory and metamemory. Front Psychol. 2018;9. https://doi.org/10.3389/fpsyg.2018.01577. Epub ahead of print.
Finch E, Minchell E, Cameron A, et al. What do stroke survivors want in stroke education and information provision in Australia? Health Soc Care Community. 2022;30. https://doi.org/10.1111/hsc.13896. Epub ahead of print.
Ferro JM, Santos AC. Emotions after stroke: a narrative update. Int J Stroke. 2020;15:256–67.
Acknowledgements
The corresponding author (Allam Harfoush) gratefully acknowledges the support and efforts of the Council for At-Risk Academics (Cara)
Funding
None received.
Author information
Authors and Affiliations
Contributions
AH completed the literature review. AH, KC, and HH were involved in protocol development, and gaining ethical approval. AH and KC were involved in patient recruitment. AH, KC, HH, and ED conducted the data analysis. AH wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Faculty of Health, Medicine, and Society Research Ethics Committee (FREC) at the University of Chester (1901-22-AH-CMS) in October 2022. The ethical principles follow the Declaration of Helsinki and good practice guidelines on the proper conduct of research. Informed consent was obtained from the patient for their anonymised information to be published in this article.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Harfoush, A., Chatterjee, K., Deery, E. et al. Exploring different stroke populations’ information needs: a cross-sectional study in England. Arch Public Health 82, 63 (2024). https://doi.org/10.1186/s13690-024-01289-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13690-024-01289-2