Abstract
Background
Chronic heart disease affects millions of people worldwide and the prevalence is increasing. By now, there is an extensive literature on outpatient care of people with chronic heart disease. We aimed to systematically identify and map models of outpatient care for people with chronic heart disease in terms of the interventions included and the outcomes measured and reported to determine areas in need of further research.
Methods
We created an evidence map of published systematic reviews. PubMed, Cochrane Library (Wiley), Web of Science, and Scopus were searched to identify all relevant articles from January 2000 to June 2021 published in English or German language. From each included systematic review, we abstracted search dates, number and type of included studies, objectives, populations, interventions, and outcomes. Models of care were categorised into six approaches: cardiac rehabilitation, chronic disease management, home-based care, outpatient clinic, telemedicine, and transitional care. Intervention categories were developed inductively. Outcomes were mapped onto the taxonomy developed by the COMET initiative.
Results
The systematic literature search identified 8043 potentially relevant publications on models of outpatient care for patients with chronic heart diseases. Finally, 47 systematic reviews met the inclusion criteria, covering 1206 primary studies (including double counting). We identified six different models of care and described which interventions were used and what outcomes were included to measure their effectiveness. Education-related and telemedicine interventions were described in more than 50% of the models of outpatient care. The most frequently used outcome domains were death and life impact.
Conclusion
Evidence on outpatient care for people with chronic heart diseases is broad. However, comparability is limited due to differences in interventions and outcome measures. Outpatient care for people with coronary heart disease and atrial fibrillation is a less well-studied area compared to heart failure. Our evidence mapping demonstrates the need for a core outcome set and further studies to examine the effects of models of outpatient care or different interventions with adjusted outcome parameters.
Systematic review registration
PROSPERO (CRD42020166330).
Similar content being viewed by others
Background
Chronic heart diseases (we consider heart failure, coronary heart disease, and atrial fibrillation) are complex clinical conditions associated with various symptoms and comorbidities such as dyspnea, fatigue, peripheral edema, and depression [1, 2]. Coronary heart disease (CHD), heart valve disease, arrhythmias, familial cardiomyopathy, toxin‐induced cardiomyopathy, and hypertension are all linked to heart failure (HF) [1]. Reported estimates of heart failure incidence in European countries and the USA ranges widely from100/100,000 person-years, in French to 4300/100,000 person-years in a US study and strongly depends, on the population studied and the diagnostic criteria used [3]. Incidence increases with age and with ageing populations this means that prevalence is also on the increase [3]. At least 26 million people are affected worldwide [4]. Coronary heart disease is the leading cause of death in both developed and developing countries. Considering current lifestyles, the incidence of CHD will continue to rise [5]. Atrial fibrillation (AF) is the most prevalent arrhythmia managed in clinical practice and one of the leading causes of HF. The 2019 Global Burden of Disease Study showed that there were about 59.7 million individuals with atrial fibrillation/flutter worldwide [6]. The majority of patients with heart failure exhibit multi‐morbidity and the number of patients with three or more chronic comorbidities increased [7]. Comorbidity is associated with increased severity of HF symptoms and corresponds to a poor quality of life and a worse prognosis [8].
Patients with chronic HF increasingly receive outpatient care. However, they are frequently hospitalised for acute decompensated as well as non‐cardiovascular causes. Assessment of prognosis of heart failure is particularly challenging. The clinical course depends on the underlying pathomechanisms and varies depending on the severity of the disease. Outcomes are difficult to predict in individual patients. Even late in heart failure, patients still have periods of “good days” and apparent stability, which can lead them and their care providers into postponing vital decisions [9]. Therapeutic interventions in each disease stage aim to modify risk factors, treat risk and structural heart disease to prevent HF, and reduce symptoms, morbidity, and mortality [10]. Holistic management approaches must foster the implementation of multidisciplinary approaches to address major contributors to the persisting burden of HF including multimorbidity, ageing, and social determinants of health [11]. Heart failure treatment constitutes challenges related to both self-care and emotional burden. Many patients are struggling emotionally due to a lack of information and education, inadequate care coordination and troublesome medication and self-monitoring of symptoms. Doing so affects their self-care ability and their well-being as well as their quality of life [12].
There is a large body of literature on the care provided to people with chronic heart diseases. However, previous systematic reviews (SRs) have mainly focused on the effects of specific health services.
Model of care is an overarching design for the provision of a particular type of health care service that is shaped by a theoretical basis, evidence-based practice, and defined standards. It consists of defined core elements and principles and has a framework that provides the structure for the implementation and subsequent evaluation of care. Clearly defined models of care help to ensure that all health professionals are working towards common goals and, most importantly, to evaluate service on agreed outcome measures [13].
This evidence map [14, 15] thus has an important purpose. We aimed to identify models of outpatient care (MoC) associated with chronic heart diseases in published systematic reviews (SRs), and to map which interventions built these models of care as well as the outcomes measured and reported. This will help to identify gaps and future research needs. A broad systematic review of primary studies was not feasible within a reasonable timescale. Hence, we decided to conduct an overview (evidence map) of systematic reviews. This approach [16,17,18] is increasingly used in research areas where the literature has already been summarised in several systematic reviews.
Objectives
-
1.
To identify any specific models of outpatient care for patients with chronic heart diseases, in systematic reviews, published in the English or German language.
-
2.
Create a comprehensive overview (evidence map) of identified interventions and outcomes.
Methods
Protocol and registration
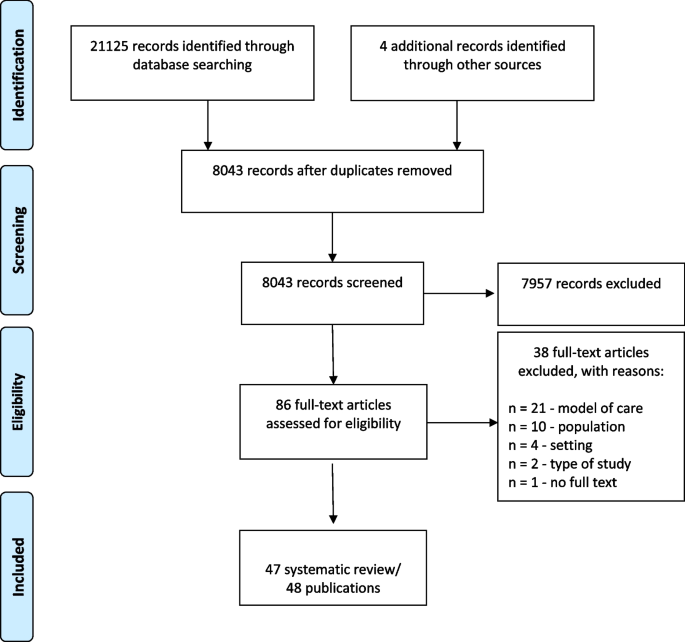
Our approach was guided by accepted methodological and reporting standards for overviews and mapping reviews [19,20,21] including PRISMA flow-chart (Fig. 1). We registered the review protocol on PROSPERO (CRD42020166330). We have not made any amendments to the information provided at registration. Our systematic mapping review focused on models of outpatient care.
Inclusion and exclusion criteria
In the protocol, we decided to include only published systematic reviews. We searched for English- and German-language human studies published since 2000. However, for pragmatic reasons we did not choose a larger period. We only included systematic reviews of models of care for people with chronic heart diseases (coronary heart disease, heart failure, and atrial fibrillation) in outpatient care that met the criteria of the Centre for Reviews and Dissemination (Database of Abstracts of Reviews of Effects, DARE) [22]. Initiation and delivery of interventions (models of care) were required to be linked to outpatient/primary care. Reviews with interventions for specific vulnerable groups (e.g. pregnant woman and palliative care) and infants (0–3 age) were excluded. All other study designs were excluded (Table 1).
Data sources and searches
The National Library of Medicine through PubMed, Cochrane Library (Wiley), Web of Science and Scopus were searched for systematic reviews published between January 1, 2000, and June, 30 2021. We used a combination of MeSH and text terms that included terms related to chronic heart diseases, models of care and outpatient care settings. A full search strategy is available in Additional file 1: Search strategy at Pubmed. We used Citavi 6, a reference management software to manage our records and remove duplicates.
Eligibility screening process
Two groups of reviewers MH, HH and AS, TR—initial search until December 2019; MH, SE and HH, SE—search update, each screening 50% of total) independently screened titles and abstracts for eligibility based on the above selection criteria. All studies reviewed as “yes” or “unsure” by either reviewer team were included in full-text screening. Agreement between both reviewers was required to exclude a study. Where consensus of eligibility was not reached a third reviewer (CA) was consulted. We obtained full texts for all selected systematic reviews, and if study eligibility remained unclear, we discussed again with a third reviewer (CA).
Data extraction
Two groups of reviewers (MH, CD and HH, SE, each 100% of total) extracted data independently and subsequently reconciled. An Excel spreadsheet for data extraction was developed and piloted by the review team. From each systematic review search dates, objectives, populations, number and types of included studies, number of included participants, components of interventions, and outcomes reported were extracted and summarised.
Data analysis
We analysed the extracted data from the included SRs with descriptive statistics for reporting frequencies where appropriate. Temporal data were represented in visual graphs to illustrate trends. All other data were presented in tabular form. We inductively categorised MoC based on the titles and summaries of the included SRs. Intervention categories were formed by inductively coding the characteristics of the interventions in the SRs (content analysis) and jointly consented by the review group. We mapped the outcomes onto the taxonomy developed by the COMET initiative [23]. The COMET initiative encourage the development and uptake of core outcome sets: an agreed standard set of outcomes that should be measured and reported, as a minimum, in all clinical trials in specific areas of health or healthcare setting [24]. We categorised by the core areas: death, physiological or clinical, life impact, resource use and adverse events [23]. If an outcome was composite and addressed several core areas, we classified it within each of the relevant domains. All authors reached final consensus on findings, interpretation and text. We did not perform an assessment of the methodological quality of the included SRs.
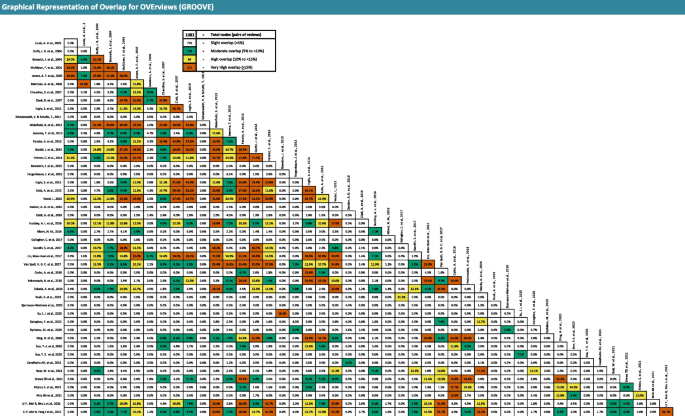
To perform a comprehensive analysis of the overlap of the included SRs, we used the GROOVE tool and included all primary studies [25]. Besides the calculation of overall Corrected Covered Areas (CCA), GROOVE provides a graphical representation of the overlap among each pair of possible SRs (nodes). A CCA value lower than 5 can be considered as a slight overlap, whereas values greater than or equal to 15 can be considered as a very high overlap (0–5; slight, 6–10; moderate, 11–15; high, and > 15; very high overlap) [26].
Results
Studies and study characteristics
After the removing of duplicates, 86 potentially eligible records were identified and screened according to the protocol. We excluded thirty-eight articles after full-text screening, because they did not meet the inclusion criteria; no model of care—21 articles [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47], no eligible population—ten articles [48,49,50,51,52,53,54,55,56,57], no eligible setting—4 articles [58,59,60,61], no SR—2 articles [62, 63], no full text available—1 article [64]. Fourty-seven systematic reviews/48 publications, covering 1154 primary studies (including double counting) were included in this review (Fig. 1). Most systematic reviews included models of care for heart failure (42 SRs), in addition to coronary heart disease (4 SRs), and atrial fibrillation (1 SR).
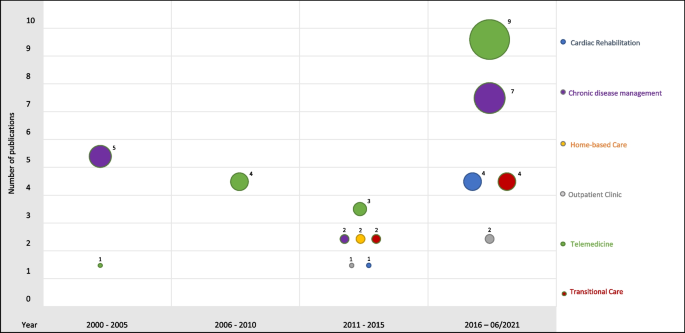
The number of publications on interventions for patients with chronic heart diseases in outpatient care has increased. While only 21.3% of the systematic reviews included here were published in 2000–2010, 55.3% were published since January 2016 (Fig. 2). The studies included in the SRs were conducted between 1967 and 2021.
The authors of the included SRs performed a systematic search of at least two to a maximum of 16 databases to identify randomised controlled trials, non-randomised controlled trials or other relevant research articles to answer the research question. Twenty-one different databases were used for literature search in the included SRs. The number of included participants ranged from 867 to 28,455. The number of included studies ranged from 6 to 70 studies per systematic review (Additional file 2: Characteristics of the included SRs).
The CCA in our overlap analysis was 3.08% (slight overlap) for all included systematic reviews. However, we measured a very high overlap (≥ 15%) at 111 of 1081 nodes and a high overlap (10–15%) at further 84 nodes. This means that a large number of studies appeared several times across the systematic reviews (Fig. 3). Five primary studies were included in 15 or more SRs (Table 2).
Evidence map on models of outpatient care
In our evidence mapping, we identified six models of outpatient care: (a) cardiac rehabilitation, (b) chronic disease management, (c) home-based care, (d) outpatient clinics, (e) telemedicine, and (f) transitional care.
We categorised MoCs interventions according to the following characteristics: remote monitoring of daily biometric data, structured telephone support, video conference, information/education program, symptom monitoring (by staff or patients), regular consultation (e.g. outpatient, hospital), home visits, pharmacologic management, nutrition, coordination, behavioural or psychosocial support, planning for discharge, and exercise, which has been visualised in Additional file 3: Mapping of the single interventions of the included SRs. In addition, we mapped the primary outcomes of the included SRs onto the taxonomy developed by the COMET initiative [23] (Additional file 4: Mapping of the primary outcomes of the included SRs). Outcomes from all core areas were used: in 30 SRs outcomes from the core areas death (65.2%) were included. Physical/clinical outcomes were included in 11 SRs (23.9%), life impact in 25 SRs (54.3%), resource use in 30 SRs (65.2%) and adverse events in 6 SRs (13%).
Cardiac rehabilitation
Cardiac rehabilitation (CR) was designed to optimise secondary prevention of chronic heart failure. It has evolved from an exercise-focused program to a comprehensive, multi-component model of care to address risk factors. Indeed, CR societies have published and internationally agreed so-called “core components” of CR, namely, nutritional counselling, risk factor modification, psychosocial management, patient education, and exercise training [65].
We included five SRs with heart failure and CHD indications for the MoC cardiac rehabilitation [66,67,68,69,70]. All included SRs on MoC reported exercise programs. In addition, four out of five included at least one telemonitoring intervention (remote monitoring of daily biometric data, structured telephone support, or video conference). Information/education programs and behavioural or psychosocial support were provided in 60% of the included SRs. One SR each described nutrition and home visits as interventions. Death and life impact are relevant outcomes for cardiac rehabilitation. All systematic reviews used outcomes of these core areas to evaluate interventions. Thus, four SRs employed psychological/clinical outcomes (80%), three SRs resource use outcomes (60%) and one SR adverse events outcomes (20%).
Chronic disease management
Definitions of chronic disease management (programs) vary substantially. We therefore included a wider range of approaches, which we considered as “chronic disease management”, e.g. case management [71], chronic care model [72], coordinated care and integrated care [73], and disease management programs [74]. Chronic disease management does not normally involve general coordination of care and preventive services such as flu vaccination [75].
The MoC chronic disease management included only SRs for people with heart failure [39, 76,77,78,79,80,81,82,83,84,85,86,87,88]. The included SRs demonstrated three core elements: telemonitoring, coordination and information/education program. Telemonitoring interventions (at least one intervention) were part in 12 SRs (85.7%). Coordination and information/education programs were each included in 71% of SRs (n = 10). In addition behavioural or psychosocial support (7; 50%), regular consultation (6; 43%), symptom monitoring (4; 29%), pharmacological management (4; 29%), and home visits (21%) were reported. Outcomes of the core areas death and resource use were reported in seven of the SRs (50%). Life impact outcomes were included in seven SRs (50%), psychological/clinical outcomes in three (21%) and adverse events outcomes in only two systematic reviews (14%).
Home-based care
Home-based care aims to improve health and prevent the need for long-term care or immediate care. It includes a variety of home services such as health promotion and teaching, clinical care, end-of-life care, rehabilitation, social adaptation and integration, and support for informal caregivers [89].
The MoC home-based care included only two SRs for people with heart failure [89, 90]. One SR was based only on home visits. The second SR included also information/education, behavioural or psychosocial support, pharmacological management, and coordination interventions. All SRs included outcomes from the core area death. Further outcomes from the core areas life impact and resource use were used in one of the two SRs.
Outpatient clinic
Outpatient clinics (often located at hospitals) provide a collaborative, multidisciplinary approach for treatment with cardiologists, nurses, pharmacists, dieticians, psychologists, and social workers. These clinics not only provide optimisation of drug therapy, but also education regarding lifestyle such as diet and exercise, medication compliance and diuretic titration strategies; they serve as a crucial link for patients who develop worsening symptoms and require earlier follow-up or medication adjustment [91].
We included three SRs for the MoC [91,92,93], one SR each for of the indications heart failure, coronary heart disease and atrial fibrillation. For all indications, information/education and symptom monitoring are listed as interventions. In addition, the following interventions are described for heart failure: regular consultation, pharmacological management, nutrition, coordination, and behavioural or psychosocial support. There were fewer interventions for CHD and AF. In two of the three systematic reviews on outpatient clinics, outcomes from four core areas were used. Outcomes on resource use were included in all three SRs.
Telemedicine
Telemedicine (TM) is delivered by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research, and evaluation. In addition, TM is used for continuing education of health care providers, all in the interests of advancing the health of individuals and their communities [94].
The majority of SRs included in the MoC telemedicine [95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111] refer to heart failure. One SR investigated telemedicine MoC for people with CHD. All SRs (n = 17) offered at least one telemonitoring intervention to their participants: remote monitoring of daily biometric data (16; 94%), structured telephone support (15; 88%) or video conference (2; 12%). In addition, the following interventions were reported in SRs: symptom monitoring (10; 59%), information/education (7; 41%), pharmacological management (5; 29%), behavioural or psychosocial support and home visits (3; 18%), coordination (2; 12%), exercise program and nutrition (1; 6%). Outcomes from four core areas were included in the TM SRs: death (13; 76%), psychological/clinical (2; 6%), life impact (9; 53%), and resource use (12; 71%). The majority of included telemedicine systematic reviews (12; 70.5%) considered outcomes from two core areas (death, ressource use).
Transitional care
Transitional care (TC) encompasses a broad range of services and environments designed to promote the safe and timely passage of patients between levels of health care and across care settings [112].
The MoC transitional care included six SRs for people with heart failure [113,114,115,116,117,118]. Four of the six included SRs reported at least one telemonitoring intervention. In addition, at least 50% of the SRs also described the following interventions: information/education, symptom monitoring, home visits, regular consultation, and coordination. Pharmacological management and behavioural or psychosocial support was only reported in one SR each. Outcomes from the core area death, life impact, and adverse events were included in two of these six SRs each.
Discussion
We used evidence mapping of systematic reviews to summarise the complex and growing literature on outpatient care for people with chronic heart diseases. We identified six different models of outpatient care (cardiac rehabilitation, chronic disease management, home-based care, outpatient clinics, telemedicine, and transitional care) and described which interventions were used and what outcomes were included to measure their effectiveness. We observed heterogeneity in terms of interventions within as well as commonalities between MoCs. In addition, we identified populations that require further investigation and observed variation in how outcomes were measured. The total overlap between the SRs was calculated as slight. It seems that this effect is due to the diversity of the models of care. Nevertheless, a high and very high overlap was measured at a total of 195 of 1081 nodes, especially within the MoCs on chronic disease management, telemedicine and transitional care.
Due to the large inclusion time frame, we were able to give a broad overview. It is apparent that research and thus the number of publications has increased in the period examined. Fourty-two out of 47 included SRs were on heart failure. This also means that AF and CHD populations are significantly less studied.
Despite the observed heterogeneity in populations, our evidence map shows noteworthy trends. Systematic reviews on chronic disease management [39, 76, 78,79,80,81,82,83,84,85,86,87,88] and telemedicine [95,96,97,98,99,100,101,102,103,104,105, 107,108,109,110,111, 119] have been increasingly published. Telemedicine provides an opportunity to improve outpatient healthcare delivery. Inequalities in access to healthcare and in the provision of healthcare services, caused by difficulties in transportation and, in some cases, lack of healthcare workers, are particularly challenging in rural areas [120]. The evidence map show core elements of models of care combined with additional interventions. Especially, education-related and telemedicine interventions were described more than 50% of the MoCs. The details on how the interventions were implemented are described in varying detail. In addition, the interventions in the primary studies varied in terms of design, for example frequency of sessions, duration, and their providers. This has not been analysed in our study and needs further investigation.
It was remarkable that outcomes were used very heterogeneously in the SRs. Only few SRs measured psychological/clinical and adverse events outcomes. Rather, outcomes of the core areas death, life impacts, and resources are used. Up to the best of our knowledge, there is a lack of a core outcome set for studies on outpatient care of chronic heart disease. Defined and agreed upon outcomes and measurement tools would help to increase comparability of the effectiveness of interventions in primary studies and systematic reviews.
As visual representation, this evidence map summarise the evolving research on outpatient care for people with chronic heart diseases: We only used published systematic reviews for our overview and evidence mapping [18]. As not necessarily required for our objectives, we have not provide an assessment of the methodological quality of the reviews by available instruments such as AMSTAR-2 [121] or ROBIS [122], neither calculate effect sizes in a meta-analysis. We included only systematic reviews that met at least four of five DARE criteria for SR [22]—we relied on the skills of the authors of the included systematic reviews in conducting the literature search, conducting and assessing study quality, selecting and presenting results.
Conclusion
In an ever-evolving research environment on outpatient care for people with chronic heart diseases, summarising research evidence on models of outpatient care and interventions is becoming increasingly complex, especially for healthcare stakeholders. Our evidence map can help bridge the gap between the available scientific evidence on outpatient care for people with chronic heart diseases and the adoption of this evidence by health systems with an overview of systematic reviews from January 1, 2000, to June 30, 2021, on models of outpatient care.
In addition, evidence maps are also a useful tool to identify gaps in the literature, and to guide future research. Our results show that the comparability of published SRs on MoC is limited due to differences in interventions and outcome measures. For example, physical/clinical outcomes are less considered in SRs. Outpatient care of CHD and AF is poorly studied compared to HF. Thus our evidence map determines the need for primary or secondary research. First of all, it would be helpful to develop a core outcome set to have a consistent set of clinical endpoints for chronic heart disease outpatient care studies. Further, future studies should examine the effects of models of outpatient care or different interventions with adjusted outcome parameters to determine which interventions in the MoCs described here have the most positive effects for the person concerned. This could provide an impetus for practice and policy to develop renewed or new model of outpatient care for patients with chronic heart diseases.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Falk H, Ekman I, Anderson R, Fu M, Granger B. Older patients’ experiences of heart failure—an integrative literature review. J Nurs Scholarsh. 2013;45(3):247–55.
Emmons-Bell S, Johnson C, Roth G. Prevalence, incidence and survival of heart failure: a systematic review. Heart. 2022;108(17):1351–60.
Savarese G, Lund LH. Global Public Health Burden of Heart Failure. Card Fail Rev. 2017;3(1):7–11. Available from: https://pubmed.ncbi.nlm.nih.gov/28785469.
Liang F, Wang Y. Coronary heart disease and atrial fibrillation: a vicious cycle. Am J Physiol Heart Circ Physiol. 2021;320(1):H1–12.
Li H, Song X, Liang Y, Bai X, Liu-Huo W-S, Tang C, et al. Global, regional, and national burden of disease study of atrial fibrillation/flutter, 1990–2019: results from a global burden of disease study, 2019. BMC Public Health. 2022;22(1):2015.
Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. The Lancet. 2018;391(10120):572–80.
Baldi I, Azzolina D, Berchialla P, Gregori D, Scotti L, Corrao G. Comorbidity-adjusted relative survival in newly hospitalized heart failure patients: a population-based study. Int J Cardiol. 2017;243:385–8.
Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, et al. Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2012;125(15):1928–52.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–1032.
Roger VL. Epidemiology of heart failure: a contemporary perspective. Circ Res. 2021;128(10):1421–34.
Nordfonn OK, Morken IM, Bru LE, Husebø AML. Patients’ experience with heart failure treatment and self-care-A qualitative study exploring the burden of treatment. J Clin Nurs. 2019;28(9–10):1782–93.
Davidson PM, Elliott D. Managing approaches to nursing care delivery. In: J. Daly (Ed.), Preparing for Professional Nursing Practice. Sydney: Maclennan and Petty; 2001.
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231.
Snilstveit B, Vojtkova M, Bhavsar A, Stevenson J, Gaarder M. Evidence & Gap Maps: A tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol. 2016;79:120–9.
Pollock A, Campbell P, Brunton G, Hunt H, Estcourt L. Selecting and implementing overview methods: implications from five exemplar overviews. Syst Rev. 2017;6(1):145.
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39.
Bragge P, Clavisi O, Turner T, Tavender E, Collie A, Gruen RL. The Global Evidence Mapping Initiative: scoping research in broad topic areas. BMC Med Res Methodol. 2011;11:92.
Cooper ID. What is a “mapping study?” J Med Libr Assoc. 2016;104(1):76–8.
Andrew Booth. EVIDENT Guidance for Reviewing the Evidence: a compendium of methodological literature and websites; 2016.
Miake-Lye IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016;5(1):28.
Centre for Reviews and Dissemination. Welcome to CRD Database: About DARE. https://www.crd.york.ac.uk/CRDWeb/AboutPage.asp; 2015 2015 Jun 3 [cited 2019 Sep 3].
Dodd S, Clarke M, Becker L, Mavergames C, Fish R, Williamson PR. A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J Clin Epidemiol. 2018;96:84–92.
Kirkham JJ, Davis K, Altman DG, Blazeby JM, Clarke M, Tunis S, et al. Core Outcome Set-STAndards for Development: The COS-STAD recommendations. PLoS Med. 2017;14(11):e1002447.
Pérez-Bracchiglione J, Meza N, Bangdiwala SI, Guzmán EN de, Urrútia G, Bonfill X et al. GROOVE - Graphical Representation of Overlap for OVErviews: Open Science Framework; 2022 2022.
Pieper D, Antoine S-L, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Allida S, Du H, Xu X, Prichard R, Chang S, Hickman LD et al. mHealth education interventions in heart failure. Cochrane Database Syst Rev. 2020;7(7):CD011845. Available from: https://pubmed.ncbi.nlm.nih.gov/32613635/.
Palm P, Qvist I, Rasmussen TB, Christensen SW, Håkonsen SJ, Risom SS. Educational interventions to improve outcomes in patients with atrial fibrillation-a systematic review. Int J Clin Pract. 2020;74(11):e13629.
Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006 [cited 2022 Jun 3]; 6:43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1660572/pdf/1471-2261-6-43.pdf.
Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008;168(7):687–94.
van der Meer S, Zwerink M, van Brussel M, van der Valk P, Wajon E, van der Palen J. Effect of outpatient exercise training programmes in patients with chronic heart failure: a systematic review. Eur J Prev Cardiol. 2012;19(4):795–803. Available from: https://pubmed.ncbi.nlm.nih.gov/22988592/.
Labrunée M, Pathak A, Loscos M, Coudeyre E, Casillas J-M, Gremeaux V. Therapeutic education in cardiovascular diseases: state of the art and perspectives. Ann Phys Rehabil Med. 2012;55(5):322–41.
Clarkesmith DE, Pattison HM, Khaing PH, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev. 2017;2017(4):CD008600.
Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review Patient Educ Couns. 2018;101(3):363–74.
Sterling MR, Shaw AL, Leung PB, Safford MM, Jones CD, Tsui EK, et al. Home care workers in heart failure: a systematic review. J Multidiscip Healthc. 2018;11:481–92.
Tse G, Chan C, Gong M, Meng L, Zhang J, Su X-L, et al. Telemonitoring and hemodynamic monitoring to reduce hospitalization rates in heart failure: a systematic review and meta-analysis of randomized controlled trials and real-world studies. J Geriatr Cardiol. 2018;15(4):298–309.
Tse G, Gong M, Meng L, Ng EMC, Tsang NS, Ali-Hasan-Al-Saegh S, et al. Effects of Telemonitoring and Hemodynamic Monitoring on Mortality in Heart Failure: a Systematic Review and Meta-analysis. Curr Emerg Hosp Med Rep. 2019;7(2):36–47.
Cui X, Dong W, Zheng H, Li H. Collaborative care intervention for patients with chronic heart failure: A systematic review and meta-analysis. Medicine (Baltimore). 2019;98(13):e14867.
Duffy JR, Hoskins LM, Chen M-C. Nonpharmacological strategies for improving heart failure outcomes in the community: a systematic review. J Nurs Care Qual. 2004;19(4):349–60.
Schumacher PM, Becker N, Tsuyuki RT, Griese-Mammen N, Koshman SL, McDonald MA, et al. The evidence for pharmacist care in outpatients with heart failure: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(5):3566–76.
Schichtel M, Wee B, Perera R, Onakpoya I, Albury C. Effect of behavior change techniques targeting clinicians to improve advance care planning in heart failure: a systematic review and meta-analysis. Ann Behav Med. 2021;55(5):383–98.
Romiti GF, Pastori D, Rivera-Caravaca JM, Ding WY, Gue YX, Menichelli D, et al. Adherence to the “atrial fibrillation better care” pathway in patients with atrial fibrillation: impact on clinical outcomes-a systematic review and meta-analysis of 285,000 patients. Thromb Haemost. 2022;122(3):406–14.
Ogungbe O, Byiringiro S, Adedokun-Afolayan A, Seal SM, Dennison Himmelfarb CR, Davidson PM, et al. Medication adherence interventions for cardiovascular disease in low- and middle-income countries: a systematic review. Patient Prefer Adherence. 2021;15:885–97.
Gebreyohannes EA, Mill D, Salter S, Chalmers L, Bereznicki L, Lee K. Strategies for improving guideline adherence of anticoagulants for patients with atrial fibrillation in primary healthcare: a systematic review. Thromb Res. 2021;205:128–36.
Biersteker TE, Schalij MJ, Treskes RW. Impact of mobile health devices for the detection of atrial fibrillation: systematic review. JMIR MHEALTH UHEALTH. 2021;9(4):e26161.
Austin RC, Schoonhoven L, Clancy M, Richardson A, Kalra PR, May CR. Do chronic heart failure symptoms interact with burden of treatment? Qualitative literature systematic review. BMJ Open. 2021;11(7):e047060.
Al-Arkee S, Mason J, Lane DA, Fabritz L, Chua W, Haque MS, et al. Mobile apps to improve medication adherence in cardiovascular disease: systematic review and meta-analysis. J Med Internet Res. 2021;23(5):e24190.
Wongvibulsin S, Habeos EE, Huynh PP, Xun H, Shan R, Porosnicu Rodriguez KA, et al. Digital health interventions for cardiac rehabilitation: systematic literature review. J Med Internet Res. 2021;23(2):e18773.
Candelaria D, Randall S, Ladak L, Gallagher R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: a systematic review and meta-analysis. Qual Life Res. 2020;29(3):579–92.
Choi JY, Choi H, Seomun G, Kim EJ. Mobile-application-based interventions for patients with hypertension and ischemic heart disease: a systematic review. J Nurs Res. 2020;28(5):e117.
Huang K, Liu W, He D, Huang B, Xiao D, Peng Y et al. Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2015;22(8):959–71.
Han E, Quek RYC, Tan SM, Singh SR, Shiraz F, Gea-Sánchez M, et al. The role of community-based nursing interventions in improving outcomes for individuals with cardiovascular disease: a systematic review. Int J Nurs Stud. 2019;100: 103415.
Kotb A, Hsieh S, Wells GA. The effect of telephone support interventions on coronary artery disease (CAD) patient outcomes during cardiac rehabilitation: a systematic review and meta-analysis. PLoS ONE. 2014;9(5):e96581.
Salzwedel A, Jensen K, Rauch B, Doherty P, Metzendorf M-I, Hackbusch M, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur J Prev Cardiol. 2020;27(16):1756–74.
Sadeghi M, Rahiminam H, Amerizadeh A, Masoumi G, Heidari R, Shahabi J, et al. Prevalence of return to work in cardiovascular patients after cardiac rehabilitation: a systematic review and meta-analysis. Curr Probl Cardiol. 2022;47(7): 100876.
Smigorowsky MJ, Sebastianski M, Sean McMurtry M, Tsuyuki RT, Norris CM. Outcomes of nurse practitioner-led care in patients with cardiovascular disease: a systematic review and meta-analysis. J Adv Nurs. 2020;76(1):81–95. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85074615563&doi=10.1111%2fjan.14229&partnerID=40&md5=ee619a95dbfad56b4bf3e1123c5bfb47.
Meiring RM, Tanimukai K, Bradnam L. The effect of exercise-based cardiac rehabilitation on objectively measured physical activity and sedentary behavior: a systematic review and meta-analysis. J Prim Care Community Health. 2020;11:2150132720935290.
Nishikawa Y, Hiroyama N, Fukahori H, Ota E, Mizuno A, Miyashita M et al. Advance care planning for adults with heart failure. Cochrane Database Syst Rev. 2020; 2(2):CD013022.
Driscoll A, Meagher S, Kennedy R, Hay M, Banerji J, Campbell D, et al. What is the impact of systems of care for heart failure on patients diagnosed with heart failure: a systematic review. BMC Cardiovasc Disord. 2016;16(1):195.
Risom SS, Zwisler A-D, Johansen PP, Sibilitz KL, Lindschou J, Gluud C et al. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev 2017;2:CD011197.
Heckman GA, Shamji AK, Ladha R, Stapleton J, Boscart V, Boxer RS, et al. Heart Failure Management in Nursing Homes: A Scoping Literature Review. Can J Cardiol. 2018;34(7):871–80.
Kruse CS, Soma M, Pulluri D, Nemali NT, Brooks M. The effectiveness of telemedicine in the management of chronic heart disease - a systematic review. JRSM Open. 2017; 8(3):2054270416681747. [cited 2022 Jun 7] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5347273/pdf/10.1177_2054270416681747.pdf.
Case R, Haynes D, Holaday B, Parker VG. Evidence-based nursing: the role of the advanced practice registered nurse in the management of heart failure patients in the outpatient setting. Dimens Crit Care Nurs. 2010;29(2):57–62.
Schadewaldt V, Schultz T. A systematic review on the effectiveness of nurse-led cardiac clinics for adult patients with coronary heart disease. JBI Library Syst Rev. 2010; 8(2):53–89. Available from: https://pubmed.ncbi.nlm.nih.gov/27820168/.
Kabboul NN, Tomlinson G, Francis TA, Grace SL, Chaves G, Rac V et al. Comparative Effectiveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J Clin Med. 2018;7(12):514.
Bjarnason-Wehrens B, Nebel R, Jensen K, Hackbusch M, Grilli M, Gielen S et al. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): a systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27(9):929–52. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85067856703&doi=10.1177%2f2047487319854140&partnerID=40&md5=52a90d3e7586541bc6c2eadc91375d82.
Cavalheiro AH, Silva Cardoso J, Rocha A, Moreira E, Azevedo LF. Effectiveness of tele-rehabilitation programs in heart failure: a systematic review and meta-analysis. HealthServInsights. 2021;14:11786329211021668.
Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;1:1183–92.
Su JJ, Yu D, Paguio JT. Effect of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: A systematic review and meta-analysis. J Adv Nurs. 2020;76(3):754–72. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85079320766&doi=10.1111%2fjan.14272&partnerID=40&md5=238b94f8ea50a8dacf6d8ae67a66d4c2.
Zwisler A-D, Norton RJ, Dean SG, Dalal H, Tang LH, Wingham J, et al. Home-based cardiac rehabilitation for people with heart failure: A systematic review and meta-analysis. Int J Cardiol. 2016;221:963–9.
Treadwell J, Perez R, Stubbs D, McAllister JW, Stern S, Buzi R. Case management and care coordination: supporting children and families to optimal outcomes. Cham, s.l.: Springer International Publishing; 2015. (SpringerBriefs in Public Health).
Wagner EH, Davis C, Schaefer J, von Korff M, Austin B. A survey of leading chronic disease management programs: are they consistent with the literature? Manag Care Q. 1999;7(3):56–66.
Nies H, Berman, Philip C, editors. Integrating services for older people: a resource book for managers. Dublin: European Health Management Association (EHMA); 2004. (vol 5) [cited 2021 Jul 16]. Available from: https://ehma.org/wp-content/uploads/2016/08/CARMEN_Integrating-Services-for-Older-People-A-Resource-Book-for-Managers.pdf.
Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, et al. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114(13):1432–45.
Nolte E, Knai C, Saltman, Richard B. Assessing chronic disease management in European health systems: Concepts and Approaches; 2014 [cited 2021 Jul 16]. Available from: https://www.euro.who.int/__data/assets/pdf_file/0009/270729/Assessing-chronic-disease-management-in-European-health-systems.pdf.
Clark AM, Wiens KS, Banner D, Kryworuchko J, Thirsk L, McLean L, et al. A systematic review of the main mechanisms of heart failure disease management interventions. Heart. 2016;102(9):707–11.
Gallagher C, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, Mahajan R et al. Integrated care in atrial fibrillation: A systematic review and meta-analysis. Heart. 2017; 103(24):1947–53. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85031688687&doi=10.1136%2fheartjnl-2016-310952&partnerID=40&md5=339bcf8a1c4170dfe2a89b0f7881afe0.
Gonseth J, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25(18):1570–95.
Gorthi J, Hunter CB, Mooss AN, Alla VM, Hilleman DE. Reducing Heart Failure Hospital Readmissions: A Systematic Review of Disease Management Programs. Cardiol Res. 2014;5(5):126–38.
Huntley AL, Johnson R, King A, Morris RW, Purdy S. Does case management for patients with heart failure based in the community reduce unplanned hospital admissions? A systematic review and meta-analysis. BMJ Open. 2016;6(5):e010933.
Jerant AF, Nesbitt TS. Heart failure disease management incorporating telemedicine: a critical review. J Clin Outcomes Manag. 2005;12(4):207–17. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-18744394627&partnerID=40&md5=4a8a9126ac791779d234d9828d045900.
Kalogirou F, Forsyth F, Kyriakou M, Mantle R, Deaton C. Heart failure disease management: a systematic review of effectiveness in heart failure with preserved ejection fraction. ESC Heart Fail. 2020;7(1):195–213. Available from: https://search.proquest.com/docview/2379680851?accountid=12235.
Kyriakou M, Middleton N, Ktisti S, Philippou K, Lambrinou E. Supportive care interventions to promote health-related quality of life in patients living with heart failure: a systematic review and meta-analysis. Heart Lung Circ. 2020;29(11):1633–47.
McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110(5):378–84.
McAlister FA, Stewart S, Ferrua S, McMurray, John J J V. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810–9.
Raat W, Smeets M, Janssens S, Vaes B. Impact of primary care involvement and setting on multidisciplinary heart failure management: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(2):802–18.
Takeda A, Martin N, Taylor RS, Taylor SJ. Disease management interventions for heart failure. Cochrane Database Syst Rev 2019;1:CD002752.
Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28(1):8–19.
Fergenbaum J, Bermingham S, Krahn M, Alter D, Demers C. Care in the home for the management of chronic heart failure: systematic review and cost-effectiveness analysis. J Cardiovasc Nurs. 2015;30(4 Suppl 1):S44-51.
Jaarsma T, Brons M, Kraai I, Luttik ML, Stromberg A. Components of heart failure management in home care; A literature review. Eur J Cardiovasc Nurs. 2013;12(3):230–41. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84878238443&doi=10.1177%2f1474515112449539&partnerID=40&md5=708850e642584420f23b41037204f0f3.
Gandhi S, Mosleh W, Sharma UC, Demers C, Farkouh ME, Schwalm J-D. Multidisciplinary heart failure clinics are associated with lower heart failure hospitalization and mortality: systematic review and meta-analysis. Can J Cardiol. 2017;33(10):1237–44. [cited 2020 May 4] Available from: https://www.onlinecjc.ca/action/showPdf?pii=S0828-282X%2817%2930248-9.
Rush KL, Burton L, Schaab K, Lukey A. The impact of nurse-led atrial fibrillation clinics on patient and healthcare outcomes: a systematic mixed studies review. Eur J Cardiovasc Nurs. 2019;18(7):526–33.
Schadewaldt V, Schultz T. Nurse-led clinics as an effective service for cardiac patients: results from a systematic review. Int J Evid Based Healthc. 2011;9(3):199–214.
World Health Organization. Telemedicine: Opportunities and Developments in Member States. Report on the Second Global Survey on eHealth 2009. Geneva: World Health Organization; 2010. (Global Observatory for Ehealth). Available from: http://gbv.eblib.com/patron/FullRecord.aspx?p=753845.
Carbo A, Gupta M, Tamariz L, Palacio A, Levis S, Nemeth Z, et al. Mobile technologies for managing heart failure: a systematic review and meta-analysis. Telemed J E Health. 2018;24(12):958–68.
Chaudhry SI, Phillips CO, Stewart SS, Riegel B, Mattera JA, Jerant AF, et al. Telemonitoring for patients with chronic heart failure: A systematic review. J Card Fail. 2007;13(1):56–62.
Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ (Online). 2007;5:334(7600):942.
Ding H, Chen SH, Edwards I, Jayasena R, Doecke J, Layland J et al. Effects of different telemonitoring strategies on chronic heart failure care: systematic review and subgroup meta-analysis. J Med Internet Research 2020; 22(11). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85096202824&doi=10.2196%2f20032&partnerID=40&md5=240dd208c066cbf51fdd8c8f3a9cf248.
Drews TEI, Laukkanen J, Nieminen T. Non-invasive home telemonitoring in patients with decompensated heart failure: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(5):3696–708.
Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;8:CD007228.
Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JGF. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015;10:CD007228.
Kitsiou S, Vatani H, Paré G, Gerber BS, Buchholz SW, Kansal MM, et al. Effectiveness of mobile health technology interventions for patients with heart failure: systematic review and meta-analysis. Can J Cardiol. 2021;37(8):1248–59.
Kotb A, Cameron C, Hsieh S, Wells G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): a systematic review and network meta-analysis. PLoS ONE. 2015;10(2):e0118681.
Lin M-H, Yuan W-L, Huang T-C, Zhang H-F, Mai J-T, Wang J-F. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med. 2017;65(5):899–911.
Louis AA, Turner T, Gretton M, Baksh A, Cleland JGF. A systematic review of telemonitoring for the management of heart failure. Eur J Heart Fail. 2003;5(5):583–90.
Martinez A, Everss E, Rojo-Alvarez JL, Figal DP, Garcia-Alberola A. A systematic review of the literature on home monitoring for patients with heart failure. J Telemed Telecare. 2006;12(5):234–41.
Nick JM, Roberts LR, Petersen AB. Effectiveness of telemonitoring on self-care behaviors among community-dwelling adults with heart failure: a quantitative systematic review. JBI Evidence Synthesis. 2021;19(10):2659–94.
Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess. 2013;17(32):1–207.
Pekmezaris R, Tortez L, Williams M, Patel V, Makaryus A, Zeltser R et al. Home telemonitoring in heart failure: a systematic review and meta-analysis. Health Aff (Millwood) 2018.
Son Y-J, Lee Y, Lee H-J. Effectiveness of mobile phone-based interventions for improving health outcomes in patients with chronic heart failure: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(5):1749.
Sua YS, Jiang Y, Thompson DR, Wang W. Effectiveness of mobile phone-based self-management interventions for medication adherence and change in blood pressure in patients with coronary heart disease: A systematic review and meta-analysis. European Journal of Cardiovascular Nursing 2020; 19(3):192–200. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85077147001&doi=10.1177%2f1474515119895678&partnerID=40&md5=c9ad2320e9337b672d2627c09fb12ed0.
Naylor M, Keating SA. Transitional care. Am J Nurs. 2008;108(9 Suppl):58–63; quiz 63.
Albert NM. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung. 2016;45(2):100–13.
Feltner C, Jones CD, Cene CW, Zheng Z-J, Sueta CA, Coker-Schwimmer EJL, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774–84.
Li Y, Fu MR, Fang J, Zheng H, Luo B. The effectiveness of transitional care interventions for adult people with heart failure on patient-centered health outcomes: a systematic review and meta-analysis including dose-response relationship. Int J Nurs Stud. 2021;117: 103902.
Li Y, Fu MR, Luo B, Li M, Zheng H, Fang J. The effectiveness of transitional care interventions on health care utilization in patients discharged from the hospital with heart failure: a systematic review and meta-analysis. J Am Med Dir Assoc. 2021;22(3):621–9.
Van Spall, Harriette G C, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail. 2017;19(11):1427–43.
Vedel I, Khanassov V. Transitional care for patients with congestive heart failure: a systematic review and meta-analysis. United States; 2015.
Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JGF. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail. 2011;13(9):1028–40.
Batsis JA, DiMilia PR, Seo LM, Fortuna KL, Kennedy MA, Blunt HB, et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67(8):1737–49.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017:j4008. [cited 2019 Sep 6].
Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016; 69:225–34. [cited 2022 Mar 1] Available from: https://www.bristol.ac.uk/media-library/sites/social-community-medicine/robis/robisjclinepi.pdf.
Acknowledgements
The authors would like to thank Adeline Reinemann for providing helpful comments on the draft manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. The project (ZS/ 2018/ 12/ 96167) belongs to the Research Association “Autonomy in old Age” (AiA) funded by the European Union (ERDF-European Regional Development Fund) and the State of Saxony-Anhalt, Germany.
Author information
Authors and Affiliations
Contributions
CA, MH, HH, EMB, RBD, AS, TR contributed to the design of the study, development of the selection criteria, and previously registered the protocol with PROSPERO. MH and HH developed the search strategy using previously published research. For the evidence map MH, HH, SE, AS, and TR completed the data search and screening. MH, HH, CD, and SE were involved in data extraction and synthesis. CD and MH conducted data visualisation. MH, CD, and HH drafted the original manuscript. All authors read, provided feedback on and approved the final manuscript. RBD acquired funding. CA provided substantial methodological advice and supervised the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors have read the final version of the manuscript and approved its submission for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search strategy at PubMed.
Additional file 2:
Characteristics of the included SRs.
Additional file 3:
Mapping of the single interventions of the included SRs.
Additional file 4:
Mapping of the primary outcomes of the included SRs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hoerold, M., Heytens, H., Debbeler, C.M. et al. An evidence map of systematic reviews on models of outpatient care for patients with chronic heart diseases. Syst Rev 12, 80 (2023). https://doi.org/10.1186/s13643-023-02227-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02227-z