Abstract
Background
Tracheal intubation and invasive mechanical ventilation initiation is a procedure at high risk for arterial hypotension in intensive care unit. However, little is known about the relationship between pre-existing peripheral microvascular alteration and post-intubation hemodynamic instability (PIHI).
Methods
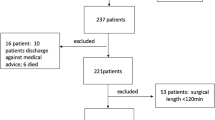
Prospective observational monocenter study conducted in an 18-bed medical ICU. Consecutive patients requiring tracheal intubation were eligible for the study. Global hemodynamic parameters (blood pressure, heart rate, cardiac function) and tissue perfusion parameters (arterial lactate, mottling score, capillary refill time [CRT], toe-to-room gradient temperature) were recorded before, 5 min and 2 h after tracheal intubation (TI). Post intubation hemodynamic instability (PIHI) was defined as any hemodynamic event requiring therapeutic intervention.
Results
During 1 year, 120 patients were included, mainly male (59%) with a median age of 68 [57–77]. The median SOFA score and SAPS II were 6 [4–9] and 47 [37–63], respectively. The main indications for tracheal intubation were hypoxemia (51%), hypercapnia (13%), and coma (29%). In addition, 48% of patients had sepsis and 16% septic shock. Fifty-one (42%) patients develop PIHI. Univariate analysis identified several baseline factors associated with PIHI, including norepinephrine prior to TI, sepsis, tachycardia, fever, higher SOFA and high SAPSII score, mottling score ≥ 3, high lactate level and prolonged knee CRT. By contrast, mean arterial pressure, baseline cardiac index, and ejection fraction were not different between PIHI and No-PIHI groups. After adjustment on potential confounders, the mottling score was associated with a higher risk for PIHI (adjusted OR: 1.84 [1.21–2.82] per 1 point increased; p = 0.005). Among both global haemodynamics and tissue perfusion parameters, baseline mottling score was the best predictor of PIHI (AUC: 0.72 (CI 95% [0.62–0.81]).
Conclusions
In non-selected critically ill patients requiring invasive mechanical ventilation, tissue hypoperfusion parameters, especially the mottling score, could be helpful to predict PIHI.
Similar content being viewed by others
Introduction
Mechanical ventilation is a central support organ therapy in critically ill patients helpful in case of coma and acute respiratory failure. However, tracheal intubation as well as invasive mechanical ventilation initiation, can induce per se post-intubation hemodynamic instability (PIHI) related to several mechanism including vascular tone alteration related to sedative drugs and impaired venous return consecutive to increased intra-thoracic pressure [1]. The engagement of the sympathetic–renin–angiotensin axis limits the deleterious circulatory impact of MV initiation, promoting vasoconstriction and tachycardia [2]. However, such compensatory mechanisms are altered by general anesthesia, especially in critically ill patients suffering from hypovolemia, hypercapnia or sepsis-related microvascular dysfunction. Arterial hypotension following emergency tracheal intubation has been reported in 10–50% of ICU patients [3,4,5]. Given that PIHI occurrence worsens the prognosis of critically ill patients [6, 7], the identification of high-risk patients is a major challenge. Several risk factors for PIHI have been reported, including age, high shock index, pH < 7.20, intubation for acute respiratory failure, non-depolarizing agents used for the neuromuscular blockade, and propofol administration [8, 9]. However, the predictive value of tissue perfusion parameters on PIHI has never been evaluated. During the last decade, several bedside “easy to use” tools have been developed to analyze peripheral tissue perfusion including skin mottling, capillary refill time, and toe-to-room temperature gradient [10]. These tissue perfusion parameters are related to organ failure severity and have emerged as strong predictors of unfavorable outcomes in ICU [11,12,13]. Our group recently found that peripheral tissue hypoperfusion markers predic hemodynamic instability following hemodialysis initiation [14].
In this prospective observational study, we aimed to assess the predictive value of tissue perfusion parameters on PIHI occurrence.
Patients and methods
Study subjects and intubation procedure
The study was conducted in an 18-bed medical intensive care unit at a tertiary university hospital. During 1 year, patients requiring intubation were eligible for the study, regardless of the indication for mechanical ventilation. Patients were not included during the night and the weekend, because protocol parameters were recorded by a physician who was not in charge of the patient. The operating physician chose the modalities of anesthesia induction in accordance with the local standard procedure. Briefly, patients received intravenously etomidate (0.3 mg/kg) followed by suxamethonium chloride (1 mg/kg). When etomidate was not used, patients received either propofol or ketamine (2 mg/kg). Curarization in patients with contraindication to suxamethonium was obtained with 1.2 mg/kg rocuronium. Oral tracheal intubation was performed using either a curved blade laryngoscope or a McGrath videolaryngoscope. After tracheal intubation, sedation was maintained using combined sufentanil, midazolam and propofol, according to local standard procedure, with a targeted score of − 2 on the Richmond Agitation–Sedation Scale.
Data collection and definition of hemodynamic instability
Data were recorded by a physician not in charge of patient care. Data collection included general demographic characteristics and comorbidities, SOFA score on the day of endotracheal intubation, SAPS II score, indication for tracheal intubation, and presence of sepsis. Respiratory and hemodynamic parameters were collected during the hour preceding TI, 5 min and 2 h after tracheal intubation. The difficulty of tracheal intubation was assessed using the Intubation Difficulty Scale [15]. The cardiac index was calculated [16] using transthoracic echocardiography. Mottling score, index and knee capillary refill time (CRT) and toe-to-room gradient temperature were serially measured as previously described [11, 17, 18]. In patients with dark skin, mottling score and knee capillary refill time were not evaluated (n = 11 in the study). Arterial blood gas and arterial lactate level were measured routinely using point-of-care testing on a GEM Premier 4000 analyzer. Vasopressor dosage and volume of intravenous fluid administered during the 2 h following intubation were recorded. Hemodynamic instability requiring intervention (PIHI) was defined as any hemodynamic worsening requiring unplanned intravenous fluid resuscitation (≥ 500 ml) or the introduction of vasoactive drugs or an increase in vasoactive drug dose by at least 0.1 µg/kg/min [19, 20]. To limit confounding factors for hemodynamic variations, we only included patients hemodynamically stable before intubation, defined as no increase or introduction of vasoactive support in the hour before intubation.
The ethical committee of the French Intensive Care Society (FICS) approved the protocol (CE SRLF 20-66).
Statistical analysis
The primary outcome was PIHI as a binary variable. Continuous variables are described as median and interquartile range (IQR) and compared using Wilcoxon’s rank-sum test or Kruskal Wallis; categorical variables are summarized by counts (percents) and compared using exact Fisher test. To evaluate the relationship between microcirculatory parameters and outcome, we used multivariable logistic regression. To avoid overfitting and collinearity, we ran separated models for each parameter. Confounders entered in the models have been selected a priori: sepsis, MAP, drugs used for TI procedure. Log-linearity assumption was checked and variables were tested for collinearity before inclusion in the multivariate model. Goodness of fit was evaluated using Le Cessie–van Houwelingen’s method and discrimination with AUC statistic.
Area under ROC curves (AUROC) was computed using the trapezoidal rule, confidence intervals were determined by the bootstrap technique, and comparison was made as described in DeLong.
The measures of associations are presented with odds ratios and 95% confidence intervals. All tests were two-sided and p values lower than 5% were considered to indicate significant associations. Analyses were performed using R statistical platform, version 3.0.2 (https://cran.r-project.org/).
Results
Characteristics of included patients
During the study period, 120 patients were included; 41% were female (n = 49) with a median age of 68 [57–77] years. Their baseline characteristics are presented in Table 1. The main indications for tracheal intubation were acute respiratory distress with hypoxemia (n = 61, 51%) or hypercapnia (n = 16, 13%) and coma from non-respiratory cause (n = 35, 29%). Most of the patients had sepsis without (n = 58, 48%) or with shock (n = 18, 16%). Median SOFA score on the day of trachea intubation was 6 [4–9] and SAPS II score was 47 [37–63]. Overall, median score on the Intubation Difficulty Scale was 1 [0–3]. Most of the patients had preserved left ventricular ejection function without right heart failure. Desaturation with a nadir < 90% occurred during the procedure in 36 patients (30%) without any difference between patients with PIHI and patients without (31 vs. 30%). One cardiac arrest occurred following TI for a septic shock patient with severe hypoxia.
Predictors of post intubation hemodynamic instability
Baseline characteristics
Fifty-one patients (42%) met the criteria defining PIHI (Table 2) with different interventions: fluid infusion (N = 25), norepinephrine introduction (N = 6) or dose increase (N = 20) (Additional file 1). At baseline, sepsis was more frequently observed in PIHI group (18 vs. 40%; p < 0.0001) as well as septic shock (4 vs. 14%; p = 0.0004). When compared to No-PIHI group, PIHI patients are characterized by higher central body temperature (37.1 [36.7–37.6] vs. 38.1 [37.4–39.2] °C; p = 0.0001), higher SOFA score (5 [4–7] vs. 9 [6–13], p < 0.0001) and higher SAPS II score (41 [29–53] vs. 57 [45–69], p < 0.0001). There was no significant difference in the Intubation Difficulty Scale between the two groups (0.5 [0; 2.0] vs. 0 [0; 2.7]; p = 0.78). Prior to intubation, during resuscitation, patients with PIHI had more often fluid expansion than patients without PIHI (61% vs. 30%; p = 0.002). During TI procedure, induction drugs were etomidate (88%) and suxamethonium chloride (55%) or rocuronium (27%) for curarization (Additional file 2).
Global hemodynamic parameters
When compared to No-PIHI group, patients with PIHI had a higher baseline heart rate (94 [82–108] vs. 112 [95–130] bpm; p < 0.0001) and higher norepinephrine infusion dose. Cardiac index and baseline both right and left ventricle echocardiographic parameters were not different between groups (Table 2).
Peripheral perfusion parameters
Baseline peripheral tissue perfusion parameters were statistically different between No-PIHI and PIHI patients. Patients who developed PIHI had higher arterial lactate level (1.3 [0.9–1.8] vs. 2.3 [1.1–3.5] mmol/L, p = 0.004), higher mottling score and prolonged knee capillary refill time (2.0 [1.3–3.0] vs. 2.9 [1.9; 5.3] s, p = 0.002) (Table 2).
After adjustment on sepsis, MAP before intubation, and type of medication used during induction, mottling score remains associated with a higher risk of PIHI (adjusted OR: 1.84 [1.21–2.82] per 1 point of mottling score increased; p = 0.005) (Table 3). The probability of PIHI according to mottling score and various thresholds of baseline MAP and heart rate is depicted in Fig. 1. In a post-hoc analysis, we re-ran our model with SOFA/SAPS II/vasopressor use instead of MAP and the mottling score remained a strong predictor of PIHI whatever the variable used (Additional file 3).
Interestingly, the mottling score remained a strong predictor of PIHI whether patients were receiving vasopressors or not (p value for interaction: 0.65, Additional file 4).
We then compared the ability of selected tissue perfusion and global hemodynamics’ parameters to predict PIHI. As shown in Fig. 2, mottling score before induction was the best predictor of PIHI with an AUC of 0.72 (CI 95% [0.62–0.81]), similar than shock index 0.70 (CI 95% [0.61–0.80]), higher than knee CRT 0.67 (CI 95% [0.57–0.78]), mean arterial pressure 0.58 (CI 95% [0.47–0.68]) or cardiac output 0.54 (CI 95% [0.43–0.65]).
The best threshold of mottling score to predict PIHI was 1, which yielded a specificity of 72.3% CI95% [63.1–81.5]) and sensitivity of 65.9% [54.5–77.3]. The negative predictive value was 75.8% and the positive predictive value was 62%. Performances of other cut-point values of the score are reported in Additional file 5.
Of note, the combination of both mottling score and baseline MAP or Toe-to-room gradient significantly increased the ability to predict PIHI, suggesting that using these tools together could be of interest (Additional file 6).
Discussion
In this prospective observational study, we found that half of critically ill patients intubated in ICU develop PIHI. We found that disease severity parameters were predictive of PIHI as well as parameters of peripheral tissue hypoperfusion, especially the mottling score.
In a large cohort of ICU patients (N = 885), Perbet et al. previously identified independent factors of PIHI, such as high SAPSII score, advanced age, acute respiratory failure as a reason for intubation, first intubation in the ICU, preoxygenation method with noninvasive ventilation and severe hypoxemia [3]. In the emergency department, other risk factors of PIHI have been reported, including chronic obstructive pulmonary disease, sepsis, low body weight and systolic blood pressure lower than 140 mmHg [21]. The shock index, defined as the heart rate divided by the systolic blood pressure [22], is an integrative global hemodynamic tool that has been widely described as a predictor of PIHI in different studies [23, 24].Our study confirmed that SAPS II score, sepsis, need of vasopressors or tachycardia are predictors of PIHI.
In addition, aside from global hemodynamics parameters, we found that peripheral tissue perfusion tools such as mottling score, knee capillary refill are predictive factors for PIHI, with mottling score being the most accurate predictor. Skin mottling has been identified as an independent predictive factor for death in septic shock patients [11, 25]. Mottling that generally develops around the knee area, reflects local decreased microvascular blood flow [26]. In sepsis patients, mottling score correlates with lactate level, urinary output and SOFA suggesting that analysis of skin analysis may be a reliable indicator of global organ perfusion [10]. Using a system combining laser Doppler and iontophoresis [27], our group has shown that endothelial-dependent microvascular reactivity is impaired in the skin knee area suggesting that mottling reflects endothelial dysfunction [28]. The endothelium plays a key role in vasomotor tone and blood pressure regulation in response to acute injury including hypovolemia [29]. Intermittent hemodialysis is a common condition on ICU which could be responsible for acute hypovolemia due to partial redistribution of blood volume from the intravascular compartment to the extracorporeal circuit. In this context, we have previously shown that mottling score is a strong predictor of arterial hypotension following intermittent hemodialysis initiation [14]. Similarly, tracheal intubation and mechanical ventilation initiation also induce acute hypovolemia in ICU due to sedative drug-induced vasoplegia and decreased venous return due to intra-thoracic venous pressure. In this study, we also identified that mottling score predicts PIHI after adjustment to global hemodynamic parameters, such as blood pressure. Such observation suggests that analysis of peripheral perfusion should be helpful before TI to evaluate the risk for PIHI.
An intubation management protocol has been developed to limit the occurrence of life-threatening complications after intubation [30]. This global strategy including pre-intubation fluid infusion provided convincing results. However, two recent randomized controlled trials challenged the benefit of systematic fluid infusion before intubation to prevent PIHI in a non-selected population of critically ill patients [31, 32]. A combination of tissue perfusion parameters and MAP, which increased the prediction of PIHI, may be of interest for tailored intervention and to limit fluid overload, associated with poor outcome in ICU [33]. In addition, the identification of patients at high risk for PIHI may be helpful for the choice of the induction drug. Based on a recent randomized trial showing that ketamine use is associated with reduced cardiovascular collapse after intubation and improved day-7 survival when compared to etomidate, ketamine should be recommended in patients at high risk for PIHI [34]
According to Perbet et al. [3], propofol use was associated with less PIHI, this observation should be taken with caution, whereas etomidate or ketamine are known to be well tolerated [35, 36] and may be the result of the selection of hemodynamically stable patients for propofol induction drugs.
Our study has several limitations. First, itis a monocentric study and results need to be confirmed in a multicenter study including a larger population. However, we analyzed more than one hundred intubations in a non-selected medical ICU population. Protocoled use of sedative drugs was not standardized in our study, but it reflected the actual practice for rapid sequence intubation in ICU, with large use of etomidate, suxamethonium or rocuronium.
Several patients were treated with vasoactive drug before TI but mottling score remains predictive of PIHI whether patient received vasopressor or not. Another issue is the difficulty of analyzing the mottled skin on patients with dark skin. In this case, the toe-to-room temperature gradient could be helpful [10, 18].
Conclusions
In this prospective study on ICU patients requiring invasive mechanical ventilation, half of the patients required fluid resuscitation or vasoactive drugs in the 2 h following TI. Skin perfusion parameters, especially pre-intubation mottling score were the strongest predictor of hemodynamic worsening.
References
Quintard H, l’Her E, Pottecher J, Adnet F, Constantin J-M, De Jong A, et al. Intubation and extubation of the ICU patient. Anaesth Crit Care Pain Med. 2017;36:327–41.
Aneman A, Pontén J, Fändriks L, Eisenhofer G, Friberg P, Biber B. Hemodynamic, sympathetic and angiotensin II responses to PEEP ventilation before and during administration of isoflurane. Acta Anaesthesiol Scand. 1997;41:41–8.
Perbet S, De Jong A, Delmas J, Futier E, Pereira B, Jaber S, et al. Incidence of and risk factors for severe cardiovascular collapse after endotracheal intubation in the ICU: a multicenter observational study. Crit Care. 2015;19:257.
Jabre P, Galinski M, Ricard-Hibon A, Devaud ML, Ruscev M, Kulstad E, et al. Out-of-hospital tracheal intubation with single-use versus reusable metal laryngoscope blades: a multicenter randomized controlled trial. Ann Emerg Med. 2011;57:225–31.
Griesdale DEG, Bosma TL, Kurth T, Isac G, Chittock DR. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008;34:1835–42.
Heffner A, Swords D, Kline J, Jones A. Frequency and significance of post-intubation hypotension during emergency airway management. Crit Care. 2011;15:P154.
Russotto V, Myatra SN, Laffey JG, Tassistro E, Antolini L, Bauer P, et al. Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA. 2021;325:1164–72.
Jaber S, Amraoui J, Lefrant J-Y, Arich C, Cohendy R, Landreau L, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34:2355–61.
Larsen R, Rathgeber J, Bagdahn A, Lange H, Rieke H. Effects of propofol on cardiovascular dynamics and coronary blood flow in geriatric patients. A comparison with etomidate. Anaesthesia. 1988;43(Suppl):25–31.
Hariri G, Joffre J, Leblanc G, Bonsey M, Lavillegrand J-R, Urbina T, et al. Narrative review: clinical assessment of peripheral tissue perfusion in septic shock. Ann Intensive Care. 2019;9:37.
Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, et al. Mottling score predicts survival in septic shock. Intensive Care Med. 2011;37:801–7.
Dumas G, Lavillegrand J-R, Joffre J, Bigé N, de Moura EB, Baudel J-L, et al. Mottling score is a strong predictor of 14-day mortality in septic patients whatever vasopressor doses and other tissue perfusion parameters. Crit Care. 2019;23:211.
van Genderen ME, Paauwe J, de Jonge J, van der Valk RJP, Lima A, Bakker J, et al. Clinical assessment of peripheral perfusion to predict postoperative complications after major abdominal surgery early: a prospective observational study in adults. Crit Care. 2014;18:R114.
Bigé N, Lavillegrand J-R, Dang J, Attias P, Deryckere S, Joffre J, et al. Bedside prediction of intradialytic hemodynamic instability in critically ill patients: the SOCRATE study. Ann Intensive Care. 2020;10:47.
Adnet F, Borron SW, Racine SX, Clemessy J-L, Fournier J-L, Plaisance P, et al. The Intubation Difficulty Scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–7.
McLean AS, Needham A, Stewart D, Parkin R. Estimation of cardiac output by noninvasive echocardiographic techniques in the critically ill subject. Anaesth Intensive Care. 1997;25:250–4.
Ait-Oufella H, Bige N, Boelle PY, Pichereau C, Alves M, Bertinchamp R, et al. Capillary refill time exploration during septic shock. Intensive Care Med. 2014;40:958–64.
Bourcier S, Pichereau C, Boelle P-Y, Nemlaghi S, Dubée V, Lejour G, et al. Toe-to-room temperature gradient correlates with tissue perfusion and predicts outcome in selected critically ill patients with severe infections. Ann Intensive Care. 2016;6:63.
Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–76.
Franklin C, Samuel J, Hu TC. Life-threatening hypotension associated with emergency intubation and the initiation of mechanical ventilation. Am J Emerg Med. 1994;12:425–8.
Lin C-C, Chen KF, Shih C-P, Seak C-J, Hsu K-H. The prognostic factors of hypotension after rapid sequence intubation. Am J Emerg Med. 2008;26:845–51.
Allgöwer M, Burri C. Shock-index. Ger Med Mon. 1968;13:14–9.
Althunayyan SM. Shock index as a predictor of post-intubation hypotension and cardiac arrest; a review of the current evidence. Bull Emerg Trauma. 2019;7:21–7.
Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE. Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care. 2012;27:587–93.
de Moura EB, Amorim FF, da Cruz Santana AN, Kanhouche G, de Souza Godoy LG, de Jesus AL, et al. Skin mottling score as a predictor of 28-day mortality in patients with septic shock. Intensive Care Med. 2016;42:479–80.
Ait-Oufella H, Bourcier S, Alves M, Galbois A, Baudel J-L, Margetis D, et al. Alteration of skin perfusion in mottling area during septic shock. Ann Intensive Care. 2013;3:31.
Debbabi H, Bonnin P, Ducluzeau PH, Lefthériotis G, Levy BI. Noninvasive assessment of endothelial function in the skin microcirculation. Am J Hypertens. 2010;23:541–6.
Bourcier S, Joffre J, Dubée V, Preda G, Baudel J-L, Bigé N, et al. Marked regional endothelial dysfunction in mottled skin area in patients with severe infections. Crit Care. 2017;21:155.
Joffre J, Hellman J, Ince C, Ait-Oufella H. Endothelial responses in sepsis. Am J Respir Crit Care Med. 2020;202:361.
Jaber S, Jung B, Corne P, Sebbane M, Muller L, Chanques G, et al. An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive Care Med. 2010;36:248–55.
Janz DR, Casey JD, Semler MW, Russell DW, Dargin J, Vonderhaar DJ, et al. Effect of a fluid bolus on cardiovascular collapse among critically ill adults undergoing tracheal intubation (PrePARE): a randomised controlled trial. Lancet Respir Med. 2019;7:1039–47.
Russell DW, Casey JD, Gibbs KW, Ghamande S, Dargin JM, Vonderhaar DJ, et al. Effect of fluid bolus administration on cardiovascular collapse among critically ill patients undergoing tracheal intubation: a randomized clinical trial. JAMA. 2022. https://doi.org/10.1001/jama.2022.9792.
Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48:1862–70.
Matchett G, Gasanova I, Riccio CA, Nasir D, Sunna MC, Bravenec BJ, et al. Etomidate versus ketamine for emergency endotracheal intubation: a randomized clinical trial. Intensive Care Med. 2022;48:78–91.
Smith DC, Bergen JM, Smithline H, Kirschner R. A trial of etomidate for rapid sequence intubation in the emergency department. J Emerg Med. 2000;18:13–6.
Walz JM, Zayaruzny M, Heard SO. Airway management in critical illness. Chest. 2007;131:608–20.
Author information
Authors and Affiliations
Contributions
Study concept and design, VD, GH and HAO. Acquisitions of data and VD, GH, JJ, JH, LR, VB, PG, SE, NB, JLB and HAO. Drafting of the manuscript VD, GH, JJ, EM, BG, GD and HAO. Critical revision of manuscript, all the authors. Statistical analysis, VD, GH, GD and HAO. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Hemodynamic and tissue perfusion parameters at different timepoints in patients without (A) or with PIHI (B). Data are expressed as medians [interquartile range] for continuous variables, and No. (%) of patients for categorical variables. ND, not determined. a, Wilcoxon matched paired test; b, comparison of data observed before vs. 5 min after TI; c, comparison of data observed before vs. 2 h after TI; d, comparison of data observed 5 min after TI vs. 2 h after TI;CRT, capillary refill time, MAP, mean arterial pressure.
Additional file 2.
Induction drugs used for patients who developed post-intubation PIHI or not.
Additional file 3.
Effect of mottling score (per point increase) on PIHI incidence adjusted on various hemodynamic/severity parameters.*Each separate model is also adjusted on sepsis and induction drugs.
Additional file 4.
Mottling score effect on post-tracheal intubation hypotension according to vasopressor use before tracheal intubation.
Additional file 5.
Performances of cut-point values of the mottling score to predict PIHI.
Additional file 6.
The delta AUROC column shows the increase in discrimination, as measured by the AUROC, due to addition of mottling score to the variable indicated in the first column (logistic regression model using mottling score together with the variable in the first column).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dubée, V., Hariri, G., Joffre, J. et al. Peripheral tissue hypoperfusion predicts post intubation hemodynamic instability. Ann. Intensive Care 12, 68 (2022). https://doi.org/10.1186/s13613-022-01043-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01043-3