Abstract
Objectives
Mucosal healing (MH) is an important goal in the treatment of patients with Crohn’s disease (CD). Noninvasive assessment of MH with normalized iodine concentration (NIC) is unknown.
Methods
In this retrospective study, 94 patients with diagnosed CD underwent endoscopy and dual-energy CT enterography (DECTE) at the post-infliximab treatment review. Two radiologists reviewed DECTE images by consensus for assessing diseased bowel segments of the colon or terminal ileum, and the NIC was measured. Patients were divided into transmural healing (TH), MH and non-MH groups. The diagnostic performance of the MH and non-MH groups with clinical factors and NIC was assessed utilizing receiver operating characteristic (ROC) curve analysis.
Results
Of the 94 patients included in our study, 8 patients achieved TH, 34 patients achieved MH, and 52 patients did not achieve MH at the post-IFX treatment review. The area under the ROC curve (AUC), sensitivity, specificity, and accuracy values were 0.929 (95% confidence interval [CI] 0.883–0.967), 0.853, 0.827, and 0.837, respectively, for differentiating MHs from non-MHs, and the optimal NIC threshold was 0.448. The AUC of the combined model for distinguishing MHs from non-MHs in CD patients, which was based on the NIC and calprotectin, was 0.964 (95% CI 0.935–0.987).
Conclusions
The normalized iodine concentration measurement in DECTE has good performance in assessment MH in patients with CD. Iodine concentration from DECTE can be used as a radiologic marker for MH.
Key points
-
1.
IFX treatment has 45% efficiency for achieving MH in our study.
-
2.
The AUC of the NIC model for assessment of MH was 0.929.
-
3.
NIC from DECTE can be used as a radiologic marker for MH.
Similar content being viewed by others
Introduction
Mucosal healing (MH) is currently the long-term treatment goal for Crohn's disease (CD) [1,2,3]. Achieving transmural healing (TH) and MH in patients with CD can reduce hospitalization and surgery rates and maintain long-term remission of clinical symptoms [4,5,6]. Accurate determination of TH and MH can help to assess the prognosis of patients with CD and to personalize treatment [7, 8]. Currently, the evaluation of MH relies on endoscopy, but it is invasive and unsuitable for patients with intestinal strictures, perforated bowel walls, or intestinal fistulas. It is reported that endoscopy can miss affected segments reportedly in 30.6% [9]. Consequently, non-invasive assessment of MH is of increasing interest to scholars and clinicians [10].
Cross-sectional imaging is crucial in the assessment of CD [11]. However, some of the bowel segments that have achieved MH endoscopically continue to show wall thickening (> 3 mm) on cross-sectional images such as magnetic resonance enterography (MRE) or computed tomography enterography (CTE) images. This suggests that there may be ongoing inflammation of the intestinal wall [12, 13]. Dual-energy CT enterography (DECTE) allows quantitative studies of the iodine concentration of diseased tissue, which has been shown to be a substitute marker for perfusion in various abdominal imaging applications [14, 15]. Iodine concentration obtained from specific intestinal regions identified by DECTE has been suggested as a marker of CD activity and histopathologic analysis [16, 17]. However, to our knowledge, there are no reports on DECTE-based assessment of MH in CD patients. The aim of this study was to assess whether the normalized iodine concentration (NIC) of the thickened wall of the terminal ileal or colonic segment could be used to diagnose endoscopic MH in CD patients.
Materials and methods
Study design and patients
This retrospective study received approval from the Clinical Medical Research Ethics Committee of our hospital. The informed consent requirement was waived.
The inclusion criteria were as follows: (1) patients with confirmed active CD at baseline; (2) patients with ulcerative inflammation in the colon or terminal ileum at baseline.
The exclusion criteria were as follows: (1) no DECTE and endoscopy examination after infliximab (IFX) treatment; and (2) poor quality of DECTE images for analysis.
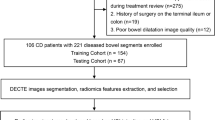
The study flow diagram is shown in Fig. 1. The diagnosis of CD is based on a combination of clinical, endoscopic, stool, biochemical, and histological investigations [18]. The following data were collected at the post-IFX treatment review: age, sex, disease duration, calprotectin, C-reactive protein (CRP) level, serum albumin level, white blood cell (WBC) count, simple endoscopic score for CD, and Harvey Bradshaw Index (HBI).
Each endoscopy was performed by two gastroenterologists with more than 15 years of colonoscopy experience. One of the primary operators performed the colonoscopy and the other assisted the primary operator in viewing the colonoscopy images, and evaluated each patient for ulcerative inflammation at baseline and for MH at the post-IFX treatment review. The MH was evaluated using the Simple Endoscopic Score for CD (SES-CD) in colonic and terminal ileum lesions. MH was characterized as an SES-CD < 3 with the absence of mucosal ulcers after IFX treatment in CD patients who had ulcerative inflammation at baseline [19,20,21].
CT scanning
DECTE was performed on all included individuals at the post-IFX treatment review. Before the examination, all patients received standardized intestinal preparation. Patients were given a light diet and bowel preparation the day before the examination. Approximately 45 min before the CT examination, each patient drank 1500–2000 ml of 2.5% isotonic mannitol solution. DECTE was performed using a GE Revolution CT scanner equipped with spectral imaging mode (GSI Assist, GE Healthcare). The scan protocol for DECTE was as follows: fast tube voltage switching between 80 and 140 kVp; tube current, 350 mA; pitch, 0.984:1; rotation time, 0.75 s; and reconstructed layer thickness, 1.25 mm. A contrast agent (iohexol, 320 mg/mL) was administered using a high-pressure syringe at 1.5 mL/kg bodyweight via peripheral veins at a rate of 3.0 mL/s. The enteric and venous phases of DECTE were collected at 45 s and 70 s after contrast injection, respectively. On a Gemstone Spectral Imaging (GSI) viewer workstation (AW4.7, GE Healthcare), the dual-energy image sets were rebuilt. The GSI viewer quantified iodine concentration by reviewing images of the decomposition spectra of water and iodine-based materials.
Quantitative iodine concentration analysis
Two radiologists with more than 6 and 20 years of expertise in diagnostic abdominal imaging reviewed DECTE enteric phase images by consensus for assessment of the diseased bowel segment of the colon or terminal ileum. TH was defined as wall thickness < 3 mm with the absence of ulcers, edema, enhancement, and complications for all ileocolonic segments [1].
The selection of the diseased bowel segment for quantitative iodine concentration analysis was based on the following criteria: (1) a segment of the colon or terminal ileum; (2) for MH patients, selection of the diseased bowel segment achieved MH; (3) for non-MH patients, selection of the diseased bowel segment with the ulcerative inflammation; (4) thickening (> 3 mm) of the diseased bowel segment wall with the highest enhancement [17]. On the GSI viewer workstation, a circular region of interest (ROI) (area, 5 mm × 5 mm) was placed on the thickened wall in the area of the highest iodine concentration for quantitative analysis. Areas of intraluminal air or fluid and perienteric fat were carefully avoided. All measurements were performed three times at various image levels of the same bowel segment to ensure consistency, and the average values were computed. The iodine concentration in the diseased intestinal wall was derived from the iodine-based material decomposition images. To reduce patient and scan time variations, the iodine concentration measurement of the lesion was normalized to that of the aorta or iliac artery by a circular ROI (area, 5 mm × 5 mm) at the same level on the iodine map to obtain a normalized iodine concentration (NIC) [22].
Construction of the combined model
Univariate analysis was used to compare the differences in clinical factors and NIC collected at the post-IFX treatment between the with and without MH patient groups. The significant variables (p < 0.05) acquired in the univariate analysis were employed as inputs. Multivariate logistic regression analysis (p < 0.05) and variance inflation factors were used to build a combined model. A combined model was constructed by combining the significant variables of clinical factors and the NIC. A receiver operating characteristic (ROC) curve analysis was used to assess the diagnostic performance for discriminating between the MH and non-MH groups.
Statistical analysis
Continuous variables were presented as the mean ± standard deviation when they followed a normal distribution and were compared using the independent sample t test; otherwise, they were presented as the median (P25, P75) and tested using the Mann‒Whitney U test. The Fisher’s exact test or chi-square test was used for categorical variables. Pearson’s correlation test was used to analyze inter-reader agreement for the iodine quantification by two radiologists. A two-sided p < 0.05 was considered significant. The above statistical analyses were performed using R 3.5.1. (R Institute for Statistical Computing).
Results
Patient characteristics
A total of 286 CD patients from November 2016 to December 2021 were enrolled in this study. The study ultimately included 94 patients who met the inclusion and exclusion criteria. Of the 94 patients included in our study (Fig. 1), 8 patients achieved TH, 34 patients achieved MH, and 52 patients did not achieve MH at the post-IFX treatment review. Clinical characteristics of patients with or without MH and TH are shown in Tables 1 and 2. Between the MH and non-MH groups, there was no significant difference in terms of patient age, sex, HBI, or perianal disease (p > 0.05). Calprotectin was significantly lower in the MH group (78.8 ug/g) than in the non-MH group (931.32 ug/g) (p < 0.001). CRP was significantly lower in the MH group (0.73 mg/dL) than in the non-MH group (7.74 mg/dL) (p < 0.001). Serum albumin was significantly higher in the MH group (42.1 g/dL) than in the non-MH group (38.9 g/dL) (p < 0.001). Disease duration and WBC were significantly lower in the MH group than in the non-MH group (p = 0.009, 0.007).
DECTE iodine concentration endoscopic comparison
The correlation coefficient of the inter-reader agreement for the iodine quantification was 0.966 (Fig. 2). Segments of the diseased bowel that achieved MH (n = 34, NIC = 0.337 ± 0.012) had a different NIC than segments that had ulcerative inflammation (n = 52, NIC = 0.556 ± 0.016). The NIC and SES-CD of patients with or without MH are shown in Table 3. The area under the ROC curve (AUC), sensitivity, specificity, and accuracy values were 0.929 (95% confidence interval [CI] 0.883–0.967), 0.853, 0.827, and 0.837, respectively. The optimal NIC threshold was 0.448, which could obtain the best combination of sensitivity and specificity, for differentiating MH from non-MH. Representative examples are shown in Figs. 3 and 4.
A 39-year-old man with Crohn’s disease achieved endoscopic mucosal healing after 6 months of therapy. a Endoscopic images of the terminal ileum show ulcerating inflammation before infliximab treatment. b Posttreatment endoscopic images show mucosal healing. c On the posttreatment enteric phase axial CTE image, the wall of the terminal ileum is thickened. d ROI1 was placed in the thickened wall of the terminal ileum in these iodine-based material decomposition images, and ROI2 was placed in the iliac artery at the same level. The NIC in this thickened wall of the terminal ileum was 0.332
A 52-year-old man with Crohn’s disease did not achieve endoscopic mucosal healing after 8 months of therapy. a Endoscopic images of the terminal ileum show ulcerating inflammation before infliximab treatment. b Posttreatment endoscopic images still show ulcerating inflammation. c On the posttreatment enteric phase axial CTE image, the wall of the terminal ileum is thickened. d ROI1 was placed in the thickened wall of the terminal ileum in these iodine-based material decomposition images, and ROI2 was placed in the artery at the same level. The NIC in this thickened wall of the terminal ileum was 0.671
Establishment of a combined model
Following univariate and multivariate logistic regression evaluation, NIC (p < 0.001) and calprotectin (p = 0.001) remained as the independent predictors for differentiating MH from non-MH. The combined model was established by combining NIC and calprotectin. The AUC of the combined model for distinguishing MH from non-MH in CD patients, which was based on the NIC and calprotectin, was 0.964 (95% CI 0.935–0.987). Table 4 summarizes the discriminatory efficacies of the diagnostic combined model. The ROC curves of the NIC, calprotectin, and combined models are shown in Fig. 5.
Discussion
In the present study, we assessed the use of iodine concentration measurement of the thickened wall of the terminal ileal or colonic segment in DECTE to evaluate endoscopic MH in CD patients and yielded a high AUC of 0.929, indicating a good prediction value for MH in CD patients using iodine concentration measurement in DECTE. To the best of our knowledge, this is the first study to demonstrate the clinical utility of the NIC to predict MH in CD patients, which may provide more information for clinical decision-making.
CTE or MRE findings have been used to assess endoscopic remission. Kim et al. [12] discussed the clinical implications of the CTE findings after endoscopic complete remission of CD in individuals treated with biological treatments. Their results showed that some of the bowel segments that have achieved MH endoscopically continue to show wall thickening of the bowel wall on CTE images. It has been reported that radiologic complete remission (CR) has an edge over endoscopic CR in terms of predicting both clinical and biochemical results in CD patients [13]. TH and radiologic CR have similar definitions, and both indicate complete disappearance of active inflammatory symptoms (< 3 mm) in both mural and extramural areas on cross-sectional images such as CTE or MRE. Of the 94 patients included in our study, 8 patients achieved TH. We found that patients with TH had lower HBI and CRP than those with non-TH, in addition to a return to normal bowel wall thickness. This suggested that patients with TH had better relief in terms of clinical symptoms and laboratory indicators. Our study showed that CTE images can be used to assess TH of CD after IFX treatment, which indicates a fairly favorable prognosis [1, 23].
Iodine concentration measurement in DECTE provides indirect information about blood flow by quantifying the estimated contrast material distribution across the diseased bowel wall at a specific instant in time, and the value of virtual monoenergetic images for the detection of CD has been the subject of numerous reports [22, 24, 25]. Researchers [17] examined qualitative CT features and iodine concentration for the diseased bowel in DECTE images in an effort to correlate quantitative CT characteristics utilizing DECTE with the Crohn's disease activity index (CDAI). The results demonstrated that the iodine concentration measured on the iodine map in DECTE was the only independent variable associated with CDAI. Dane et al. [16] found that iodine concentration from DECTE can be employed as a radiologic measure of histopathologic disease activity in CD. MRE can well reflect the lesion activity and prognosis of CD by means of elastic imaging and changes of different sequence signals. However, MRE examination is time-consuming and expensive. The above articles have shown that the NIC of DECTE is better able to assess Crohn's disease activity and histologic active inflammation grades, and CTE is simple, inexpensive, and suitable for clinical wide development. In clinical practice, we can use NIC to detect MH in patients when they cannot tolerate endoscopy or have intestinal strictures, fistulas, or perforations that prevent them from completing colonoscopy, which also complements endoscopy. Our results demonstrated a relatively high accuracy of 0.837, indicating a good predictive value for MH in CD patients.
In most CD studies, the MH rate for IFX ranged from 30 to 60% [3, 26]. Of the 94 patients included in our study, IFX treatment has 45% efficiency for achieving MH. Following univariate and multivariate logistic regression evaluation, NIC (p < 0.001) and calprotectin (p = 0.001) remained as the independent predictors for differentiating MH from non-MH. The AUC of the combined model for distinguishing MH from non-MH in CD patients, which was based on the NIC and calprotectin, was 0.964 (95% CI 0.935–0.987). Calprotectin has been an important biomarker for the clinical assessment of MH [20, 27]. We observed that the calprotectin level was significantly lower in the MH group (78.8 ug/g) than in the non-MH group (931.32 ug/g). The findings of our research are consistent with those of previous publications [28,29,30].
Our study had several limitations. First, we used a manual method to place the ROI on the thickened wall in the area of the highest iodine concentration. Due to the thinness of the transmural healed bowel wall, the ROI was difficult to place accurately and we did not measure the NIC for TH. To increase the efficacy of iodine quantification, automated segmentation and measurement for diseased and transmural healed bowels should be further improved. Second, as a specific DECT scanner (GE Spectrum CT) was used, the results of the study may need to be validated on other DECT machines. Third, MRE has been demonstrated to be a valuable technique to evaluate MH, further comparative studies with MRE are necessary. Finally, there was a relatively small number of patients and a lack of baseline DECTE. Our future studies will focus on collecting DECTE before and after different drugs treatment in CD patients to expand the applicability of the study.
Conclusion
The DECTE-based assessment of the NIC has good performance in predicting MH in patients with CD. Iodine concentration measurement from DECTE can be used as a radiologic marker of MH in CD patients.
Availability of data and materials
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
Abbreviations
- AUC:
-
Area under the ROC curve
- CD:
-
Crohn’s disease
- CPR:
-
C-reactive protein
- CR:
-
Complete remission
- CDAI:
-
Crohn’s disease activity index
- DECTE:
-
Dual-energy CT enterography
- IFX:
-
Infliximab
- MH:
-
Mucosal healing
- MRE:
-
Magnetic resonance enterography
- NIC:
-
Normalized iodine concentration
- ROI:
-
Region of interest
- ROC:
-
Receiver operating characteristic
- SES-CD:
-
Simple endoscopic score for Crohn’s disease
- TH:
-
Transmural healing
- WBC:
-
White blood cell
References
Turner D, Ricciuto A, Lewis A et al (2021) STRIDE-II: an update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology 160:1570–1583
Ben-Horin S, Lahat A, Amitai MM et al (2019) Assessment of small bowel mucosal healing by video capsule endoscopy for the prediction of short-term and long-term risk of Crohn’s disease flare: a prospective cohort study. Lancet Gastroenterol Hepatol 4:519–528
Bertani L, Fornai M, Fornili M et al (2020) Serum oncostatin M at baseline predicts mucosal healing in Crohn’s disease patients treated with infliximab. Aliment Pharmacol Ther 52:284–291
Geyl S, Guillo L, Laurent V, D’Amico F, Danese S, Peyrin-Biroulet L (2021) Transmural healing as a therapeutic goal in Crohn’s disease: a systematic review. Lancet Gastroenterol Hepatol 6:659–667
Ungaro RC, Yzet C, Bossuyt P et al (2020) Deep remission at 1 year prevents progression of early Crohn’s disease. Gastroenterology 159:139–147
Vaughan R, Tjandra D, Patwardhan A et al (2022) Toward transmural healing: sonographic healing is associated with improved long-term outcomes in patients with Crohn’s disease. Aliment Pharmacol Ther 56:84–94
Lafeuille P, Hordonneau C, Vignette J et al (2021) Transmural healing and MRI healing are associated with lower risk of bowel damage progression than endoscopic mucosal healing in Crohn’s disease. Aliment Pharmacol Ther 53:577–586
Zhu C, Hu J, Wang X et al (2022) A novel clinical radiomics nomogram at baseline to predict mucosal healing in Crohn’s disease patients treated with infliximab. Eur Radiol 32:6628–6636
Samuel S, Bruining DH, Loftus EV Jr et al (2012) Endoscopic skipping of the distal terminal ileum in Crohn’s disease can lead to negative results from ileocolonoscopy. Clin Gastroenterol Hepatol 10:1253–1259
Lin X, Qiu Y, Feng R et al (2020) Normalization of C-reactive protein predicts better outcome in patients With Crohn’s disease with mucosal healing and deep remission. Clin Transl Gastroenterol 11:e00135
Bruining DH, Zimmermann EM, Loftus EV Jr, Sandborn WJ, Sauer CG, Strong SA (2018) Consensus recommendations for evaluation, interpretation, and utilization of computed tomography and magnetic resonance enterography in patients with small Bowel Crohn’s disease. Radiology 286:776–799
Kim C, Park SH, Yang SK et al (2016) Endoscopic complete remission of crohn disease after anti-tumor necrosis factor-α therapy: CT enterographic findings and their clinical implications. AJR Am J Roentgenol 206:1208–1216
Kim MC, Kim SH, Koh SJ, Park JH, Yoon H (2022) Clinical implication of radiologic complete remission on Crohn’s disease: compared with endoscopic remission. Eur J Radiol 155:110469
Gordic S, Puippe GD, Krauss B et al (2016) Correlation between dual-energy and perfusion CT in patients with hepatocellular carcinoma. Radiology 280:78–87
Thaiss WM, Haberland U, Kaufmann S et al (2016) Iodine concentration as a perfusion surrogate marker in oncology: further elucidation of the underlying mechanisms using Volume Perfusion CT with 80 kVp. Eur Radiol 26:2929–2936
Dane B, Sarkar S, Nazarian M et al (2021) Crohn disease active inflammation assessment with iodine density from dual-energy CT enterography: comparison with histopathologic analysis. Radiology 301:144–151
Kim YS, Kim SH, Ryu HS, Han JK (2018) Iodine quantification on spectral detector-based dual-energy CT enterography: correlation with Crohn’s disease activity index and external validation. Korean J Radiol 19:1077–1088
Maaser C, Sturm A, Vavricka SR et al (2019) ECCO-ESGAR guideline for diagnostic assessment in IBD part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 13:144–164
Peyrin-Biroulet L, Reinisch W, Colombel JF et al (2014) Clinical disease activity, C-reactive protein normalisation and mucosal healing in Crohn’s disease in the SONIC trial. Gut 63:88–95
Weinstein-Nakar I, Focht G, Church P et al (2018) Associations among mucosal and transmural healing and fecal level of calprotectin in children with Crohn’s disease. Clin Gastroenterol Hepatol 16:1089-1097.e1084
Daperno M, D’Haens G, Van Assche G et al (2004) Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc 60:505–512
Xu X, Zhu J, Wang X, Zhu C, Wu X (2022) Diagnostic performance of dual-energy CT in nonspecific terminal ileitis. Jpn J Radiol. https://doi.org/10.1007/s11604-022-01288-9
Castiglione F, Imperatore N, Testa A et al (2019) One-year clinical outcomes with biologics in Crohn’s disease: transmural healing compared with mucosal or no healing. Aliment Pharmacol Ther 49:1026–1039
Lee SM, Kim SH, Ahn SJ, Kang HJ, Kang JH, Han JK (2018) Virtual monoenergetic dual-layer, dual-energy CT enterography: optimization of keV settings and its added value for Crohn’s disease. Eur Radiol 28:2525–2534
Guler E, Unal NG, Hekimsoy I et al (2021) Dual-energy CT enterography in evaluation of Crohn’s disease: the role of virtual monochromatic images. Jpn J Radiol 39:341–348
D’Haens G, Vermeire S, Lambrecht G et al (2018) Increasing infliximab dose based on symptoms, biomarkers, and serum drug concentrations does not increase clinical, endoscopic, and corticosteroid-free remission in patients with active luminal Crohn’s disease. Gastroenterology 154:1343-1351.e1341
Dreesen E, Baert F, Laharie D et al (2020) Monitoring a combination of calprotectin and infliximab identifies patients with mucosal healing of Crohn’s disease. Clin Gastroenterol Hepatol 18:637-646.e611
Jessen B, Rodriguez-Sillke Y, Sonnenberg E et al (2021) Level of tumor necrosis factor production by stimulated blood mononuclear cells can be used to predict response of patients with inflammatory bowel diseases to infliximab. Clin Gastroenterol Hepatol 19:721-731.e721
Grover Z, Burgess C, Muir R, Reilly C, Lewindon PJ (2016) Early mucosal healing with exclusive enteral nutrition is associated with improved outcomes in newly diagnosed children with luminal Crohn’s disease. J Crohns Colitis 10:1159–1164
Noh SM, Oh EH, Park SH et al (2020) Association of faecal calprotectin level and combined endoscopic and radiological healing in patients with Crohn’s disease receiving anti-tumour necrosis factor therapy. J Crohns Colitis 14:1231–1240
Funding
This study has received funding from the Research Funds for Academic and Technological Leaders in Anhui Province (No. 2021D299).
Author information
Authors and Affiliations
Contributions
CZ and JH contributed equally to this work. CZ and JH were involved in conceptualization and methodology. CR, JZ and BZ were involved in data curation and visualization. YG and CL were involved in formal analysis. CZ and JH were involved in writing: original draft. XW and JL were involved in writing: review, editing and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study received approval from the Clinical Medical Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University. The informed consent requirement was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. JL is an employee of the CT Research Center, GE Healthcare China.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, C., Hu, J., Rong, C. et al. Mucosal healing assessment in Crohn’s disease with normalized iodine concentration from dual-energy CT enterography: comparison with endoscopy. Insights Imaging 14, 63 (2023). https://doi.org/10.1186/s13244-023-01397-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-023-01397-7