Abstract
Background
The REVISE (Re-Evaluating the Inhibition of Stress Erosions in the ICU) trial will evaluate the impact of the proton pump inhibitor pantoprazole compared to placebo in invasively ventilated critically ill patients.
Objective
To outline the statistical analysis plan for the REVISE trial.
Methods
REVISE is a randomized clinical trial ongoing in intensive care units (ICUs) internationally. Patients ≥ 18 years old, receiving invasive mechanical ventilation, and expected to remain ventilated beyond the calendar day after randomization are allocated to either 40 mg pantoprazole intravenously or placebo while mechanically ventilated.
Results
The primary efficacy outcome is clinically important upper GI bleeding; the primary safety outcome is 90-day mortality. Secondary outcomes are ventilator-associated pneumonia, Clostridioides difficile infection, new renal replacement therapy, ICU and hospital mortality, and patient-important GI bleeding. Tertiary outcomes are total red blood cells transfused, peak serum creatinine concentration, and duration of mechanical ventilation, ICU, and hospital length of stay. Following an interim analysis of results from 2400 patients (50% of 4800 target sample size), the data monitoring committee recommended continuing enrolment.
Conclusions
This statistical analysis plan outlines the statistical analyses of all outcomes, sensitivity analyses, and subgroup analyses. REVISE will inform clinical practice and guidelines worldwide.
Trial registration
www.ClinicalTrials.gov NCT03374800. November 21, 2017.
Similar content being viewed by others
Introduction
Approximately 2–4% of adults acutely admitted to an intensive care unit (ICU) develop upper gastrointestinal (GI) bleeding [1,2,3,4]. For bleeding prevention, approximately 70% of critically ill patients are prescribed stress ulcer prophylaxis [3], most commonly proton pump inhibitors (PPIs). In a recent European, multicenter, blinded trial, intravenous pantoprazole (PPI) was associated with a reduction in clinically important upper GI bleeding compared with placebo following an unplanned ICU admission of adults who were at risk for gastrointestinal bleeding [4]. Similarly, in PEPTIC, a large cluster-crossover trial, upper GI bleeding rates were lower during treatment periods when ICUs preferentially used PPIs for stress ulcer prophylaxis rather than histamine-2 receptor blockers (H2RAs) [5]. In both of these trials, upper GI bleeding was a secondary outcome; lack of adjustment for multiplicity, and high rates of non-adherence with study treatment respectively limited inferences from these observations. Additionally, among patients with high acuity of illness in both trials, there was a trend toward higher mortality in those receiving PPI. These findings highlight the need for further research to establish the efficacy and safety of PPIs for stress ulcer prophylaxis in contemporary ICU practice.
REVISE (Re-Evaluating the Inhibition of Stress Erosions) is an ongoing international randomized trial, the objective of which is to determine the effect of pantoprazole versus placebo on the primary efficacy outcome of clinically important upper GI bleeding and the primary safety outcome of 90-day mortality [[6]: NCT03374800]. Secondary outcomes are ventilator associated pneumonia (VAP), Clostridioides difficile (C. difficile) infection, renal replacement therapy, ICU and hospital mortality, and patient-important GI bleeding.
This document outlines the statistical analysis plan (SAP) for REVISE, reported using current guidelines [7].
Methods
REVISE is a multicenter, randomized, stratified, concealed, blinded parallel group trial in patients ≥ 18 years old in the intensive care unit (ICU), designed in collaboration with the Canadian Critical Care Trials Group (CCCTG) [[8]:www.ccctg.ca], the Australian and New Zealand Intensive Care Society Clinical Trials Group (ANZICS-CTG) [[9]:www.anzics.com.au/clinical-trials-group], and other international colleagues. Inclusion and exclusion criteria are summarized in Table 1. In brief, eligible patients are adults who are admitted to the ICU, receiving invasive mechanical ventilation and expected to remain ventilated beyond the calendar day after randomization, and without a clear indication or contraindication to PPI. Eligible patients are enrolled by either a priori informed consent or by informed consent to continue or deferred consent, or opt out, in alignment with local approvals [10].
When notified by research staff or investigators about eligible patients, research pharmacists or other blinded study personnel use a password-protected website to access the automated central randomization program to ensure concealed 1:1 allocation, stratified by center and pre-hospital acid suppression (i.e., PPI or H2RA or neither). Randomized patients receive either 40 mg pantoprazole intravenously or an identical placebo while mechanically ventilated in the ICU up to 90 days after randomization or until death, discontinuation of mechanical ventilation, or clinically important GI bleeding. All patients, families, clinical, and research staff are blinded to allocation.
Research staff upload daily data from hospital charts to a secure web-based electronic data capture system (iDataFax, Seattle, Washington) including baseline data, study drug administration, daily data in ICU up to 90 days post randomization, relevant laboratory values, cointerventions, trial outcomes, reports for adjudication, duration of mechanical ventilation, ICU and hospital stay, and mortality. Patients discharged alive from hospital before 90 days are followed for 90 days to obtain vital status. Further details are reported elsewhere [[6]: NCT03374800] and in our protocol [10].
Ethics
REVISE is approved by the Research Ethics Boards (REBs) and Human Research Ethics Committees (HRECs) of all participating regions and hospitals. REVISE is also approved by Health Canada [HC6-24-c210404], Clinical Trials Ontario Research Ethics Project ID: 1360, the Northern Sydney Local Health District Human Research Ethics Committee (HREC) [2019/ETH08405], and Comissão Nacional de Ética em Pesquisa (CONEP) [5.734.590]. Regulatory oversight in Canada is by Health Canada [HC6-24-c210404].
Outcomes
The primary efficacy outcome is clinically important upper GI bleeding occurring in the ICU or resulting in ICU readmission during the index hospital stay [10]. Research staff prospectively collect data related to GI bleeding, allowing blinded central duplicate adjudication as described elsewhere [1, 2, 10].
The primary safety outcome is all-cause mortality at 90 days after randomization.
Secondary outcomes include VAP in the ICU, C. difficile infection in the hospital, new renal replacement therapy in the ICU, ICU and hospital mortality, and patient-important GI bleeding as defined through interviews and focus groups with ICU survivors and family members [11].
Tertiary outcomes include total red blood cells transfused in the ICU, peak serum creatinine concentration in the ICU, and duration of mechanical ventilation and duration of stay in the ICU and hospital, measured in days [10].
Adverse events and serious adverse events are as follows: key adverse events (AEs) and serious adverse events (SAEs) relevant to REVISE are already pre-defined primary or secondary trial outcomes. REVISE follows 5 published recommendations for rational reporting of SAEs in investigator-initiated ICU trials of drugs in common use [12].
Sample size
The sample size of 4800 patients was chosen on the basis of plausible baseline risks of GI bleeding and plausible effect sizes of pantoprazole versus placebo and a target of 85% power [10]. Also, across the range of higher baseline risks of death due to high illness severity, 4800 patients will provide at least 70% power to detect an increase in risk of death associated with pantoprazole that would deter its use in such patients [4]. Further details are found elsewhere [[6]: NCT03374800] and in the REVISE protocol [10].
Statistical analysis
All analyses will be conducted blinded to treatment allocation; the randomization code will only be broken when the analyses are complete, unless serious safety concerns arise. We will describe baseline characteristics of enrolled patients using descriptive statistics (count and percentage for categorical variables and mean or median with standard deviation or interquartile range for continuous variables, as appropriate).
Details regarding the main analysis plan, sensitivity analyses, and subgroup analyses are found in Table 2. The main analyses will be conducted per the intention-to-treat principle by analyzing patients according to their randomized group, regardless of protocol compliance. We will compare the time to the primary and secondary binary outcomes in the two groups using Cox proportional hazards regression. We will adjust for the stratification variable of pre-hospital acid suppression in the analyses [13, 14]. As the APACHE II score is strongly associated with mortality, to maximize statistical efficiency, we will also adjust for baseline APACHE II score for the mortality outcomes. For the primary efficacy and primary safety outcomes, we will present Kaplan-Meier curves. We will report hazard ratios with 95% confidence intervals (CIs) as well as the absolute risk differences and their respective 95% CIs. For the outcome of total red blood cells transfused in the ICU, we will compare the two groups using Poisson regression, adjusting for pre-hospital acid suppression. For all other continuous outcomes, we will compare the two groups using linear regression on the original scale or on the log-scale (to normalize the distribution, if needed), adjusting for pre-hospital acid suppression. If the distribution remains non-normal after transformation, we will employ a nonparametric approach. We will use graphics and other relevant methods to examine the assumption of proportional hazards for Cox regression analyses [15,16,17].
Since all data are collected in hospital, except 90-day mortality for those discharged alive from hospital prior to 90 days, we anticipate very few missing data. For continuous outcomes with data missing for more than 2% of patients, we will perform multiple imputation analysis using multiple imputation by chained equations and will combine using Rubin’s rule [18]. Evidence has shown that multiple imputation is one of the optimal methods for handling data that is assumed missing at random [19]. For the time-to-event analyses, patients with incomplete follow-up will be censored at time of last follow-up.
All estimates of effect will be reported to two decimal places. p-values will be reported to three decimal places with those less than 0.001 reported as p < 0.001. The criterion for statistical significance will be set at alpha = 0.05, using 2-sided tests. Separately applied to secondary and tertiary outcomes, and to subgroup analyses, the sequential Holm-Šidák approach will be used to adjust for multiple significance testing [20, 21]. The sequential Holm-Šidák approach consists of ordering all p-values from smallest to largest, and then comparing them to an adjusted level of significance calculated as 1-(1-0.05)1/C, where C indicates the number of comparisons that remain. In the case of 11 outcomes, the smallest p-value would be compared to 1-(1-0.05)1/11, the second p-value to 1-(1-0.05)1/10, and so on, with the last one being compared to 1-(1-0.05) (i.e., 0.05). The sequential testing procedure stops as soon as a p-value fails to reach the corrected significance level [20, 21]. Analyses will be performed using SAS 9.4 (Cary, NC).
Sensitivity analyses
We will perform sensitivity analyses as follows (Table 2).
-
1) For both the primary efficacy outcome (clinically important upper GI bleeding) and the primary safety outcome (90-day mortality), we will conduct a sensitivity analysis which is not adjusted for pre-hospital acid suppression.
-
2) For both the primary efficacy outcome (clinically important upper GI bleeding) and the primary safety outcome (90-day mortality), we will conduct a sensitivity analysis which includes center in the model as a random effect [22]. To avoid possible problems with model convergence due to a small number of events in some centers, we will not adjust for the stratification variable of center in the main models.
-
3) For our primary efficacy outcome (clinically important upper GI bleeding), we will conduct a sensitivity analysis using a competing risk analysis approach [23] with death as the competing risk using the Fine and Gray proportional sub-distribution hazards model [24, 25].
-
4) For both the primary efficacy outcome (clinically important upper GI bleeding) and the primary safety outcome (90-day mortality), we will conduct a sensitivity analysis restricted to patients receiving study drug on ≥ 80% of study days while mechanically ventilated, to investigate the effect of pantoprazole under conditions of optimal protocol adherence as clinically appropriate.
Subgroup analyses
We will conduct analyses of both the primary efficacy outcome of clinically important upper GI bleeding and the primary safety outcome of 90-day mortality in five a priori subgroup pairs. Analyses will be adjusted for pre-hospital acid suppression. In Table 2, we pre-specify the hypothesized direction of effect, or lack thereof, also described here. For the overall trial, we hypothesize that pantoprazole will reduce the risk of clinically important upper GI bleeding and that pantoprazole will increase the risk of death within 90 days.
-
1) Pre-hospital use of acid suppression (PPIs or H2RAs) vs. none: We hypothesize that pantoprazole is more effective at preventing clinically important upper GI bleeding among patients with versus without pre-hospital acid suppression, given concerns about hypergastrinemia upon discontinuation of acid suppression [26, 27]. We hypothesize no modification of the effect of pantoprazole on 90-day mortality.
-
2) Illness severity measured by APACHE II score of ≥ 25 or < 25: We hypothesize no modification of the effect of pantoprazole on clinically important upper GI bleeding. We hypothesize that pantoprazole is more harmful in terms of increased risk of 90-day mortality among patients with higher versus lower illness severity, given the high illness severity subgroup finding in the SUPICU trial [4].
-
3) Medical vs. surgical/trauma ICU admitting diagnosis: We hypothesize no modification of the effect of pantoprazole on preventing clinically important upper GI bleeding. We hypothesize no modification of the effect of pantoprazole on 90-day mortality.
-
4) SARS-CoV-2 positive vs. negative status: We hypothesize no modification of the effect of pantoprazole on clinically important upper GI bleeding. We hypothesize that pantoprazole is more harmful in patients with versus without SARS-CoV-2 in terms of increased risk of 90-day mortality, given findings of prolonged course and worse outcomes of infected patients exposed to PPIs [28]. Patients with SARS-CoV-2 positive status will be considered those with active COVID-19 infection, not those with an incidental SARS-CoV-2 positive test result.
-
5) Female vs. male: We hypothesize no modification of the effect of pantoprazole on clinically important upper GI bleeding. We hypothesize no modification of the effect of pantoprazole on 90-day mortality. Sex is recorded for all patients, ascertained per medical chart documentation, and will also be analyzed and reported at baseline by randomized group. The sociocultural, environmental, and behavioral factors influencing a person’s self-identity according to gender are beyond the scope of this ICU trial.
We will include an interaction term between each subgroup variable and treatment group to test for subgroup effects. For any interaction p-value below 0.10, we will conduct a formal assessment of subgroup credibility using the only structured 4-category (high to very low credibility) instrument for assessing subgroup effects developed by an international expert panel, rigorously tested by multiple stakeholders with detailed guidance for each judgment [29].
Interim analyses
The independent REVISE data monitoring committee (DMC) includes professor Roberts (Oxford), Dr. McAuley (Queen’s University of Belfast), and Dr. Thomlinson (Chair, University of Toronto). When 1200 patients were enrolled, the DMC reviewed 90-day mortality data and recommended continuing REVISE.
When 2400 patients (50% recruitment) had 90-day mortality ascertained, we conducted a single interim analysis of all outcomes. To maintain the overall type-I error rate (i.e., α), for the interim analysis, we used a conservative Haybittle-Peto stopping rule with a critical value of three standard deviations with a fixed conservative α = 0.001 [30, 31]. The DMC also examined reports regarding the following: (1) recruitment (center and patient), screening, consent, and coenrolment rates; (2) protocol procedures (randomization, stratification, study drug, and other adherence issues); and (3) trial outcomes.
Guided by their charter [32, 33], the DMC considered the balance of benefits and harms when reviewing the blinded interim analysis data. On December 5, 2022, the DMC advised the REVISE steering committee to continue enrolment to trial completion.
Publication
The results manuscript will be submitted to a general clinical journal regardless of the results. Authorship will follow ICMJE guidelines. All trial sites, investigators, and research coordinators will be cited. Funders will have no influence on data handling, analysis, or writing of the manuscript. Our final report will follow guidance from CONSORT (Consolidated Standards of Reporting Trials) 2010 [34, 35] and CONSERVE (CONSORT and SPIRIT Extension for RCTs Revised in Extenuating Circumstances) [36]. The scientific protocol of REVISE was not modified due to the pandemic.
Discussion
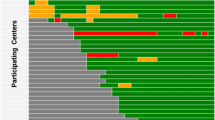
Ongoing uncertainty about the consequences of daily PPIs in critically ill patients have raised concerns about the risk-benefit ratio being shifted towards a neutral effect or harm. REVISE will provide low risk of bias estimates and more than double trial evidence on the impact of PPIs on health outcomes that will markedly increase the strength of inferences regarding clinically important bleeding, mortality, VAP, and C. difficile infection. Results will not necessarily be generalizable to patients who are breathing spontaneously or are receiving no enteral nutrition. Recruitment started on July 9, 2019. As of May 1, 2023, 4124 patients have been recruited in 63 centers internationally in Canada, Australia, the UK, USA, Saudi Arabia, Kuwait, and Pakistan.
Despite the low cost of pantoprazole per dose, acid suppression costs worldwide are sizable, given nearly universal daily prescribing in the ICU. Furthermore, integrating healthcare resources consumed for bleeding and infectious outcomes is necessary to inform policy. A parallel externally funded economic evaluation (E-REVISE) will address the cost-effectiveness of acid suppression in the ICU for healthcare systems. If acid suppression causes more harm than good or consumes resources without sufficient benefit, pantoprazole will be a candidate for de-adoption.
In this SAP, we have presented plans for using an intention-to-treat approach for analyses of all outcomes, including assessment of the robustness of the findings using a series of sensitivity analyses and subgroup analyses. We have followed the guidance for SAP for clinical trials to outline the analysis details of the trial [7]. Aligned with the World Health Organization's Joint Statement on Public Disclosure of Results from Clinical Trials, requiring timely public disclosure of results [37]:https://www.who.int/news/item/18-05-2017-joint-statement-on-registration, data will be analyzed and disseminated as soon as possible to inform bedside care and practice guidelines worldwide.
Availability of data and materials
Not applicable for this statistical analysis plan.
References
Cook DJ, Fuller H, Guyatt GH, for the Canadian Critical Care Trials Group. Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med. 1994;330:377–81.
Cook DJ, Guyatt GH, Marshall J, for the Canadian Critical Care Trials Group, et al. A comparison of sucralfate and ranitidine for prevention of upper gastrointestinal bleeding in patients requiring mechanical ventilation. N Engl J Med. 1998;338(12):791–7.
Krag M, Perner A, Wetterslev J, for the SUP-ICU co-authors, et al. Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med. 2015;41(5):833–45. https://doi.org/10.1007/s00134-015-3725-1. Epub 2015 Apr 10. PMID: 25860444.
Krag M, Marker S, Perner A, et al. for the SUP-ICU Trial Group. Pantoprazole in patients at risk for gastrointestinal bleeding in the ICU. N Engl J Med. 2018;379(23):2199–208. https://doi.org/10.1056/NEJMoa1714919.
Young PJ, Bagshaw SM, Forbes AB, for the PEPTIC Investigators for the Australian and New Zealand Intensive Care Society Clinical Trials Group, Alberta Health Services Critical Care Strategic Clinical Network, and the Irish Critical Care Trials Group, et al. Effect of stress ulcer prophylaxis with proton pump inhibitors vs histamine-2 receptor blockers on in-hospital mortality among ICU patients receiving invasive mechanical ventilation: the PEPTIC trial. JAMA. 2020;323(7):616–26. https://doi.org/10.1001/jama.2019.22190. PMID: 31950977.
NCT03374800. Accessed 1 May 2023.
Gamble C, Krishan A, Stocken D, et al. Guidelines for the content of statistical analysis plans in clinical trials. JAMA. 2017;318(23):2337–43. https://doi.org/10.1001/jama.2017.18556.
www.ccctg.ca. Accessed May 1, 2023.
www.anzics.com.au. Assessed May 1, 2023.
Deane AM, Alhazzani W (co-first authors), Guyatt G, et al. for the REVISE Investigators, the Canadian Critical Care Trials Group, the Australian and New Zealand Intensive Care Society Clinical Trials Group. REVISE: Re-Evaluating the Inhibition of Stress Erosions in the ICU: a randomised trial protocol. BMJ Open. 2023;13:e075588. https://doi.org/10.1136/bmjopen-2023-075588.
Cook DJ, Swinton M, Krewulak K, Fiest K, Dionne J, Debigare S, Guyatt GH, Taneja S, Alhazzani W, Burns KEA, Marshall J, Muscedere J, Gouskos A, Finfer S, Deane A, Myburgh J, Rochwerg B, Ball I, Mele T, Niven D, English S, Verhovsek M, Vanstone M for the Canadian Critical Care Trials Group. What counts as patient-important upper gastrointestinal bleeding in the ICU? A mixed-methods study protocol of patient and family perspectives. BMJ Open 2023;0:e070966. Published online 2023 May 18. https://doi.org/10.1136/bmjopen-2022-070966.
Cook D, Lauzier F, Rocha M, et al. Serious adverse events in academic critical care research. CMAJ. 2008;178:1181.
Kahan BC, Morris TP. Reporting and analysis of trials using stratified randomisation in leading medical journals: review and reanalysis. BMJ. 2012;345: e5840.
Pocock SJ, Assmann SE, Enos LE, Kasten LE. Subgroup analysis, covariate adjustment and baseline comparisons in clinical trial reporting: current practice and problems. Statist Med. 2002;21:2917–30.
Harrell FE, Lee KL. Verifying assumptions of the Cox proportional hazards model. Proceedings of the Eleventh Annual. SAS User's Group International Conference. Cary, N.C.: SAS Institute, Inc.; 1986:823–828.
Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239–41.
Wei LJ. Testing goodness of fit for proportional hazards model with censored observations. J Am Stat Assoc. 1984;79:649–52.
Little R, Rubin D. Statistical analysis with missing data. 2nd edition. Hoboken, NJ: Wiley; 2002; Rubin DB: Multiple imputation for nonresponse in surveys. New York: J Wiley & Sons; 1987.
Zhang Y, Alyass A, Vanniyasingam T, et al. A systematic survey of the methods literature on the reporting quality and optimal methods of handling participants with missing outcome data for continuous outcomes in randomized controlled trials. J Clin Epidemiol. 2017;88:67–80.
Abdi H. Holm’s sequential Bonferroni procedure. Encyclopedia of Research Design. Neil Salkind (Ed.), Thousand Oaks, CA: Sage. 2010
Li G, Taljaard M, Van den Heuvel E, et al. An introduction to multiplicity issues in clinical trials: the what, why, when and how. Int J Epidemiol. 2017;46(2):746–55.
Kahan BC. Accounting for centre-effects in multicentre trials with a binary outcome – when, why, and how? BMC Med Res Methodology 2014, 14:20.biomedcentral.com/1471-2288/14/20.
Thabane L, Mbuagbaw L, Zhang S, et al. A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med Res Methodol. 2013;13(1):92.
Bakoyannis G, Touloumi G. Practical methods for competing risks data: a review. Statistical Methods in Medical Research. 2012;21(3):257–72.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 1999;94(446):496–509.
Lødrup AB, Reimer C, Bytzer P. Systematic review: symptoms of rebound acid hypersecretion following PPI treatment. Scand J Gastroenterol. 2013;48(5):515. https://doi.org/10.3109/00365521.2012.746395.
Helgadottir H, Bjornsson ES. Problems associated with deprescribing of proton pump inhibitors. Int J Mol Sci. 2019;20(21):5469. https://doi.org/10.3390/ijms20215469.PMID:31684070;PMCID:PMC6862638.
Lee SW, Ha EK, Yeniova AO, et al. Severe clinical outcomes of COVID-19 associated with PPIs: a nationwide cohort study with propensity score matching. Gut. 2021. https://doi.org/10.1136/gutjnl-2020-322248.
Schandelmaier S, Briel M, Varadhan R, et al. Development of the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) in randomized controlled trials and meta-analyses. CMAJ. 2020;192(32):E901–6. https://doi.org/10.1503/cmaj.200077.
Haybittle JL. Repeated assessment of results in clinical trials of cancer treatment. British J Radiology. 1971;44:793.
Peto R, Pike M, Armitage P, et al. Design and analysis of randomized control trials requiring prolonged observations of each patient. British J Cancer. 1976;34:585.
Calis KA, Archdeacon P, Bain R, et al. Recommendations for data monitoring committees from the Clinical Trials Transformation Initiative. Clinical Trials. 2017;14(4):342–8.
DAMOCLES Study Group. A proposed charter for clinical trials data monitoring committees: helping them to do their job well. Lancet. 2005;365:711–22.
Schulz KF, Altman DG, Moher D, for the CONSORT Group, et al. CONSORT 2010 statement. PLoS Med. 2010;7(3):e1000251.
Schulz KF, Altman DG, Moher D, for the CONSORT Group, et al. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11:32.
Orkin AM, Gill PJ, Ghersi D, for the CONSERVE Group, et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA. 2021;326(3):257. https://doi.org/10.1001/jama.2021.994.
www.who.int/news/item/18-05-2017-joint-statement-on-registration Joint Statement on Public Disclosure of Results from Clinical Trials. Assessed 1 May 2023.
Acknowledgements
The trial was designed by the REVISE steering committee including national and international management committees, the REVISE investigators and research coordinators, the Canadian Critical Care Trials Group, and the Australian and New Zealand Intensive Care Society Clinical Trials Group. We are grateful to others at the Methods Center at McMaster University (Lisa Buckingham, France Clarke, Mary Copland, Karlo Matic, Ashley Sawyer, Alyson Takaoka) and The George Institute (Fatima Butt, Anna Cheng, Conrad Nangla, Fiona Osborne, Tina Schneider, Isabella Schoeler, Anna Tippet) for their expertise. We appreciate the suggestions of Drs. Neill Adhikari, Dean Fergusson, and Mark Borthwick on this report.
Role of the funders
The funders/sponsors have no role in the conception, design, conduct, oversight, analysis, interpretation, write-up, review or approval of the manuscript, or decision to submit the manuscript for publication.
Career award funding
Dr. W Alhazzani holds a Mid-Career Award from the Department of Medicine at McMaster University. Dr. S English holds a National New Investigator Award from the Heart and Stroke Foundation of Canada. Dr S Finfer holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. Dr N Hammond holds an Emerging Leadership Fellowship from the National Health and Medical Research Council of Australia. Dr. F Lauzier is a recipient of a Research Career Award from the Fonds de la recherche du Québec-Santé. Dr. J Marshall holds the Unity Health Chair in Trauma Research. Dr J Myburgh holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. Dr B Venkatesh holds a Leadership Fellowship from the National Health and Medical Research Council of Australia. Dr P Young holds a Clinical Research Practitioner Fellowship from the Health Research Council of New Zealand. Dr. D Cook holds a Research Chair in Knowledge Translation in Critical Care from the Canadian Institutes for Health Research.
Data sharing
Following the publication of REVISE, the dataset will be used for secondary studies addressing additional hypothesis-driven questions (e.g., predictors of gastrointestinal bleeding). Access by REVISE investigators will follow a submitted rationale, analysis plan, and approval by the management committee. Requests for access to the dataset by external investigators will be considered following a submitted rationale, analysis plan, and approval by the management committee and research ethics boards as relevant. Requirements will be stipulated in a pre-specified data sharing agreement. Only de-identified data will be provided and will be transferred via a secure web portal.
Funding
REVISE is funded by peer-reviewed grants [Canadian Institutes of Health Research 201610PJT-378226-PJT-CEBA-18373; Canadian Institutes of Health Research 202207CL3-492565-CTP-CEBA-19215]. The National Health and Medical Research Council of Australia grant [GNT1124675] funds enrolment in Australia. REVISE was approved by the National Institute for Health Research (NIHR) in the UK as a Portfolio Study [CPMS ID 45782], eligible for support from the NIHR Clinical Research Network. [https://www.nihr.ac.uk/researchers/collaborations-services-and-support-for-your-research/run-your-study/crn-portfolio.htm]. This trial received no support from the commercial or private sector.
Author information
Authors and Affiliations
Contributions
Concept and design: A Al-Fares, W Alhazzani, Y Arabi, L Billot, D Cook, A Deane, S English, S Finfer, G Guyatt, R Hall, N Hammond, M Hardie, D Heels-Ansdell, S Knowles, F Lauzier, J Marshall, J Muscedere, J Myburgh, M Ostermann, A Poole, L Saunders, L Thabane, B Venkatesh, F Xie, P Young, N Zytaruk. Acquisition, analysis, or interpretation of data: A Deane, L Billot, D Cook, S Finfer, G Guyatt, M Hardie, D Heels-Ansdell, S Knowles, L Thabane, N Zytaruk. Drafting of the manuscript: W Alhazzani, Y Arabi, L Billot, D Cook, A Deane, S Finfer, G Guyatt, M Hardie, D Heels-Ansdell, F Lauzier, L Thabane, B Venkatesh, P Young, N Zytaruk. Critical revision of the manuscript for important intellectual content: A Al-Fares, S English, R Hall, N Hammond, S Knowles, Marshall, J Muscedere, J Myburgh, M Ostermann, A Poole, L Saunders, F Xie. Statistical analysis: W Alhazzani, L Billot, D Cook, A Deane, S Finfer, G Guyatt, D Heels-Ansdell, L Thabane. Obtained funding: A Al- Fares, W Alhazzani, Y Arabi, L Billot, D Cook, A Deane, S English, S Finfer, G Guyatt, R Hall, N Hammond, M Hardie, D Heels-Ansdell, S Knowles, F Lauzier, J Marshall, J Muscedere, J Myburgh, M Ostermann, A Poole, L Saunders, L Thabane, B Venkatesh, F Xie, P Young, N Zytaruk. Administrative, technical, or material support: Y Arabi, D Cook, A Deane, S Finfer, G Guyatt, M Hardie, D Heels-Ansdell, S Knowles, J Myburgh, M Ostermann, L Saunders, A Poole, L Thabane, N Zytaruk. Data integrity: D Cook, M Hardie, D Heels-Ansdell, S Knowles, L Saunders, N Zytaruk.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
REVISE is approved by Health Canada [HC6-24-c210404], Clinical Trials Ontario Research Ethics Project ID: 1360, the Northern Sydney Local Health District Human Research Ethics Committee (HREC) [2019/ETH08405], and Comissão Nacional de Ética em Pesquisa (CONEP) [5.734.590]. Regulatory oversight is by Health Canada [HC6-24-c210404]. All participating centers have local ethics approval.
Consent for publication
Not applicable for this statistical analysis plan.
Competing interests
All authors are involved in the REVISE Trial in some capacity. Otherwise, the authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heels-Ansdell, D., Billot, L., Thabane, L. et al. REVISE: re-evaluating the inhibition of stress erosions in the ICU—statistical analysis plan for a randomized trial. Trials 24, 796 (2023). https://doi.org/10.1186/s13063-023-07794-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-023-07794-z