Abstract
Background
For patients with varicose veins, the goal is to relieve pain and swelling, reduce the severity of edema, improve skin changes, and heal ulcers associated with venous disease. Compression therapy is the cornerstone of their management. Several studies have shown that wearing an elastic bandage for the first 24 h and then a compression stocking for a week can effectively reduce the pain after thermal ablation. However, in clinical practice, patient compliance with this treatment could be better, considering difficulties in pulling up and removing the compression stocking, tightness, and skin irritation because these must be worn for a prolonged period. A potential solution to battling these barriers is short-term compression therapy. Besides, the effect and necessity of wearing compression stockings after thermal ablation have been questioned. Based on current clinical experience and limited evidence, although some scholars have suggested that compression therapy may be an unnecessary adjunctive therapy after thermal ablation, there is still a great deal of uncertainty in the absence of compression therapy after thermal ablation compared to compression therapy. Therefore, we advocate further research to evaluate the clinical effect of short-term postoperative compression therapy. Furthermore, well-designed randomized controlled trials are needed.
Methods
A prospective, multicenter, non-inferiority randomized controlled trial is designed to evaluate the non-inferiority of target vein occlusion rate at 3 months. Three hundred and sixty patients will be randomly assigned in a 1:1 ratio to one of the following treatments: (A) 3 M™ Coban™ elastic bandage for 48 h or (B) 3 M™ Coban™ elastic bandage for the first 24 h and then a class II compression full-length stocking (23–32 mm Hg) for 1 week. The two groups will be compared on several variables, including target vein occlusion rate at 3 months (primary outcome indicator), pain, quality of life, clinical severity of varicose veins, postoperative complications, time to return to regular work, and compliance.
Discussion
Suppose the effect of the 3 M™ Coban™ elastic bandage for 48 h proves to be non-inferior to long-term compression therapy. In that case, this short-term treatment may contribute to a future update of clinical guidelines for compression therapy after thermal ablation of varicose veins, resulting in higher patient compliance and better postoperative quality of life.
Trial registration
Clinical Trials NCT05840991. Registered on May 2023.
Similar content being viewed by others
Introduction
Background
Varicose veins are a disease/syndrome in which the subcutaneous veins of the lower extremities are dilated, prolonged, and tortuous, reaching at least 3 mm in diameter[1]. Varicose veins are present in 10–30% of the general population; this percentage increases with age [2]. The conventional treatment for varicose veins is high ligating/stripping (HL/S) of the great saphenous vein [3]. Since the 1990s, radiofrequency ablation (RFA), endovenous laser ablation (EVLA), and ultrasound-guided foam sclerotherapy (UGFS) have been widely used in the treatment of varicose veins [4]. Among them, RFA and EVLA have primarily replaced traditional surgery with shorter operative time, lower postoperative complication rates, and shorter recovery times [5,6,7,8,9,10,11,12,13]. Compression therapy is commonly used after invasive treatment of varicose veins in the lower extremities, a strategy inherited from post-surgical varicose vein care. It aims to maintain occlusion of the treated veins and prevent bruising and recanalization [14]. Elastic bandages and compression stockings are the most popular form of compression devices.
The American Venous Forum suggests starting with an elastic bandage a few days after the procedure, and the pressure should be over 20 mmHg [15]. Based on the experience of generations of clinicians and relevant evidence-based medical evidence, the National Institute of Health and Care Excellence recommends using compression (bandaging or hosiery) for no more than 7 days after interventional treatment for varicose veins [16]. Several studies have shown that wearing an elastic bandage for the first 24 h and then a compression stocking for a week can effectively reduce the pain after thermal ablation. Elderman [17] compared the difference in pain between those who wore elastic bandages for the first 24 h and then a class II compression stocking for 2 weeks and those who only used elastic bandages for 24 h. It was found that compression stocking was significant for pain relief during the first week postoperatively. Ye [18] also compared the above compression therapies and found that wearing compression stockings reduced the severity of pain during the first postoperative week in C2 varicose veins patients. However, there was no significant benefit after wearing the stockings for more than 1 week. Based on this, Bootun [19] compared the outcomes of patients treated with compression stockings for 1 week after an elastic bandage for the first 24 h with those who only wore an elastic bandage for 24 h. They found that patients in the compression stockings group had significantly lower pain scores than others at 2–5 days; it suggests that wearing compression stockings for a week after venous thermal ablation may be sufficient to relieve pain. However, poor patient compliance is a frequent problem in clinical practice with wearing compression stockings, with considerations related to difficulties in pulling up and removing the compression stockings, concerns with tightness, and skin irritation because these must be worn for a prolonged period [20]. In addition, subsequent clinical trials have questioned the necessity and effect of wearing compression stockings after thermal ablation. AYO [21], who evaluated whether wearing stockings for 1 week after endovenous thermal ablation could improve clinical outcomes in patients, showed that compression therapy had no significant effect on the outcome after thermal ablation in patients with non-ulcerated varicose veins. Pihlaja [22] found that patients without compression therapy after RFA had a 100% vein occlusion rate at 6 months compared to those wearing compression stockings for 2 weeks. The study results of Onwudike [23] also showed that the clinical effect of not wearing compression socks after thermal ablation was not worse than that of wearing compression socks for 2 weeks, which supported the conclusion that the extensive use of compression socks for compression therapy after thermal ablation had no clinical benefits for patients. Besides, a meta-analysis suggested that 48 h may be an ideal short-term compression therapy for patients with varicose veins treated with thermal ablation only [24].
Based on current clinical experience and limited evidence, although some scholars have suggested that compression therapy may be an unnecessary adjunctive therapy after thermal ablation, there is still a great deal of uncertainty in the absence of compression therapy after thermal ablation compared to compression therapy. Therefore, we advocate further research to evaluate the clinical effect of short-term postoperative compression therapy. In summary, the quality of current published studies must be improved due to the small sample size, lack of detailed data on compression therapy, and inconsistent findings. Moreover, most existing studies focus on postoperative pain, with less attention to the target vein occlusion rate; further well-structured randomized controlled trials are needed. In this study protocol, we propose to evaluate the non-inferiority of the target vein occlusion rate at 3 months. We expect to provide a basis for simplifying the compression therapy after thermal ablation.
Objectives
The study’s primary objective is determining the target vein occlusion rate at 3 months, assessed with a Duplex ultrasound scan. Recanalization will be defined by a segment of the vein ≥ 5 cm. Secondary objectives are to compare the two treatment groups for pain scores at baseline, 1 week, and 3 months using a visual analog scale (VAS); quality of life scores at baseline, 1 week, and 3 months using the AVVQ (Aberdeen Varicose Vein Questionnaire); clinical change using the VCSS (Venous Clinical Severity Score) at baseline, 1 week, and 3 months; postoperative complications including edema, ecchymosis, paresthesia, skin burn/discoloration, phlebitis, hematoma, infection, deep vein thrombosis, and pulmonary embolism; time is taken to return to routine work; patient compliance with the intervention assessed with a questionnaire.
Methods
The following information follows the SPIRIT reporting guidelines [25].
Study design
The study design is a prospective, multicenter, non-inferiority, randomized controlled trial.
Study setting
The current study will take place in nine hospitals in six provinces in China. The centers of this study are as follows:
-
The Fourth Affiliated Hospital of Zhejiang University School of Medicine
-
Sir Run Run Shaw Hospital of Zhejiang University School of Medicine
-
The Second Affiliated Hospital of Zhejiang University School of Medicine
-
Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan
-
China-Japan Union Hospital of Jilin University
-
Yantai Yuhuangding Hospital
-
The First Affiliated Hospital of Dalian Medical University
-
Affiliated Hospital of Shaoxing University
-
Jiangsu Province Hospital of Traditional Chinese Medicine
Participants
This trial was conducted in patients with primary varicose great saphenous veins of lower extremities diagnosed in nine target hospitals from April 2023 to August 2023. All participants included in the trial signed an informed consent form.
Inclusion criteria
The inclusion criteria are aged 18 to 80, primary unilateral lower limb saphenous varicose veins; clinical grades C2 to C4; diameter of the main trunk of the saphenous vein in the thigh segment ≥ 2 mm to ≤ 15 mm; and agree to participate in this study and voluntarily sign the informed consent form.
Exclusion criteria
The exclusion criteria are known to have difficulty tolerating surgery; the main trunk of the saphenous vein is extremely twisted or tightly attached to the skin; previous history of ipsilateral varicose vein surgery in the lower extremity; combined deep vein thrombosis or previous deep vein thrombosis in the affected lower extremity; uncorrectable coagulation dysfunction or a significant blood abnormalities with significant bleeding tendency (platelets ≤ 30 × 10^9/L); ankle-brachial index (ABI) < 0.6 and/or absolute ankle pressure < 60 mmHg; known allergy to bandage or stocking used in the treatment; pregnancy or breastfeeding; involvement in other clinical trials; and other patients deemed unsuitable for this study by the investigator.
Randomize and blinding
Patients will be randomized (using a random number table generated by the Excel RANDOM function) to group A or B. A fixed data analyst will generate the table of random numbers via computer. The randomization scheme will be hidden from doctors and patients. Since the intervention in this trial could not blind the doctors and patients, only the data analyzers were blinded.
Description of intervention
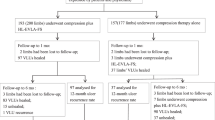
Before compression therapy, all patients will undergo a standard thermal ablation procedure (RFA, Medtronic Closure Fast or EVLA, Eufoton 1470 nm ring laser). Patients will be randomized to groups A or B. Patients randomized to group A will be asked to wear the 3 M™ Coban™ elastic bandage for 48 h after the surgery. Patients randomized to group B will be asked to wear the 3 M™ Coban™ elastic bandage for 24 h and then a class II compression full-length stockings (23–32 mmHg) day and night time for 1 week (Fig. 1). The surgeon will place the bandages on the patient's leg while still lying on the operating table after thermal ablation. By the way, implementing short-term or long-term compression therapy will not require alteration to usual care pathways (including the use of any medication) and these will continue for both trial arms.
Primary outcome
The study’s primary outcome is the target vein occlusion rate at 3 months, assessed with a duplex ultrasound scan. Recanalization will be defined by a segment of the vein ≥ 5 cm.
Target vein occlusion rate = number of target venous closure cases in the group/total number of cases in the group.
Secondary outcomes
The secondary outcomes include the following:
-
Pain
Patients will be asked to record pain scores with VAS, and the scale ranges from 0 (no pain) to 10 (worst pain imaginable) [26].
-
Quality of life
Patients will be asked to fill out the AVVQ to measure the health status of varicose vein patients based on symptoms and impact on daily activities. A total score ranging from 0 to 35, with 35 being the worst quality of life [27].
-
Venous clinical severity
Patients will be asked to fill out the VCSS to evaluate the severity of the hallmarks of venous disease. The questionnaire consisted of ten questions, each of which was answered by 0 (none), 1 (mild), 2 (moderate), and 3 (severe)—a total score ranging from 0 to 30, with 30 being the worst quality of venous disease [28].
-
Postoperative complications
Postoperative complications include postoperative edema, ecchymosis, sensory abnormalities, skin burns/discoloration, phlebitis, hematoma, infection, deep vein thrombosis, and pulmonary embolism.
-
Time to return to regular work
The investigator will use a uniform question to ask the patient how long it takes to return to regular work, life, or both (days), and then record.
-
Compliance
Compliance refers to the extent to which patients follow compression therapy as recommended by their clinicians. Investigators will ask patients whether they have completed compression treatment as recommended by their doctors in the past week or 3 months. The answer to this question involves 1 (none), 2 (occasionally), 3 (mostly), and 4 (entirely). Those who still need to fully follow the study protocol for compression treatment should continue to be asked about their actual compression treatment and recorded.
Trial timescales
At the current rate of patients presenting to the centers, relatively broad inclusion criteria, and experience from previous trials of this nature, this study is expected to be completed within approximately twelve months (Fig. 2, Additional file 1. SPIRIT Checklist for Trials).
Baseline
Each center will have two permanent medical staff to gather information and conduct follow-ups, an investigator to collect information, and a checker to evaluate the quality of questionnaires and patient cooperation. All investigators will be trained before the official follow-up. At baseline, primary demographic data will be collected for each patient. Patients’ contact details will also be collected to enable the scheduling of follow-up appointments. Patients will be asked to record pain scores with VAS, fill out a quality of life questionnaire (AVVQ), and assess their clinical scores (CEAP and VCSS). They will also be asked to attend a follow-up in 1 week and at 3 months.
Follow-up
Patients will be followed up in the outpatient clinic at 1 week and 3 months. At the 1 week follow-up, patients will be asked to record pain scores with VAS, fill out a quality of life questionnaire (AVVQ), and will have their clinical scores assessed (VCSS). They will also be asked how soon they could return to regular work, postoperative complications, and compliance with the intervention. A venous Duplex scan will be held to determine the occlusion of the target vein. Follow-up at 3 months after thermal ablation will be the same as at 1 week follow-up.
Sample size and study duration
According to the literature [29,30,31] and clinical experts’ recommendations, the target vein occlusion rate in the control group (group B) was set to 98%, and a non-inferiority threshold δ of − 6% was taken [17]. With a power of 90% and 2.5% (unilateral) significance equivalence, a minimum of 230 patients (115 per group) will need to be recruited. However, considering a potential drop-out rate of 20%, combined with the low probability of adverse events in this trial, the total sample size was expanded to 360 patients. With 3 months follow-up, the study will run for 12 months.
Recruitment
Recruitment will occur in outpatient clinics at each center; patients who meet the inclusion criteria will be made aware of this study and provided with the appropriate information. Patients expressing an interest in participation will be offered an appointment for a screening visit with a study investigator/ a doctor. After taking a detailed medical history and a detailed duplex ultrasound examination, if the potential participant meets the criteria and is willing to proceed to enrolment in the trial, they will sign informed consent forms. Here the potential participant will be fully briefed on the trial process, the treatments, risks, economic compensation, and follow-up.
Statistical analysis
Continuous data will be compared by the Student t-test or Mann–Whitney U test for parametric and non-parametric data, as appropriate. Categorical data will be compared by the chi-square test or Fisher’s exact test, as appropriate. Considering the participants might crossover or be lost to follow-up, we will test non-inferiority using two analysis sets. One is the intention-to-treat set, considering all patients as randomized regardless of whether they received the randomized treatment, the other is the per-protocol set. We propose declaring short-term compression therapy non-inferior to long-term compression therapy, only if shown to be non-inferior using both the “intention-to-treat” and “per-protocol” analysis sets. P < 0.05 will be considered statistically significant, and all data will be analyzed using SAS 9.2 software.
Data collection and confidentiality
To promote participant retention and complete follow-up, we will add WeChat and record the mobile phone number of each participant, and investigators will phone contact or send a text message to remind the participants to follow up before each study visit. The investigators will contact participants who default a scheduled appointment to re-arrange another appointment within 1 week. In addition, we will ask each participant about their compliance with compression therapy (one of the secondary outcomes) to assess whether participants discontinue or deviate from intervention protocols. Participants will be allocated an individual trial identification number according to the order of inclusion. The anonymized trial data will be shared with other researchers to enable international prospective meta-analyses. Information will be entered by Epidata 3.1 in pairs to ensure its quality.
All information collected for this study, including electronic versions (stored on USB sticks) and paper questionnaires, will be securely stored in password cabinets at each center for at least 10 years. Data collected during the research will be kept strictly confidential and only accessed by members of the trial team (or individuals from the Sponsor organization or center sites where relevant to the trial).
Data monitoring, safety, and quality control
The ethics committee of each center will audit trial conduct as the circumstances may require. Trial Management Group will meet to review trial conduct per month. The Trial Steering Group and the independent Data Monitoring meet to review conduct throughout the trial period.
No significant adverse events are expected. An adverse event (AE) is an untoward medical occurrence in a patient or clinical study subject, which may or may not be caused by the investigational device. All such events, whether expected or not, should be recorded. A severe adverse event (SAE) is an untoward and unexpected medical occurrence or effect that results in death or is life-threatening, explicitly referring to an event in which the subject was at risk of death at the time of the event. It does not refer to an event that hypothetically might have caused death if it were more severe, requires hospitalization or prolongation of existing inpatients’ hospitalization, results in persistent or significant disability or incapacity, or results from a congenital anomaly or congenital disability. All AEs should be reported as following procedures.
An SAE form should be completed and sent by fax or email to the chief investigator within 24 h. All SAEs should be reported to the Research Ethical Committee where, in the opinion of the chief investigator, the event was “related” (i.e., resulted from the administration of any of the research procedures) and “unexpected” (i.e., an event that is not listed in the Protocol as an expected occurrence). Reports of related and unexpected SAEs should be submitted within 15 days of the chief investigator’s awareness of the event, using the NRES SAE form for non-IMP studies. Local investigators should report any SAEs as required by their Local Research Ethics Committee, sponsor, and/or Research and Development Office.
The investigator and sponsor will do their best to prevent possible injury caused by the design of this study. In case of any injury related to this study, the sponsor will bear the corresponding treatment costs and make compensation by national laws and regulations. If an adverse event caused by the investigational compression treatment causes harm, the clinical research institution and the investigator will provide timely and adequate treatment and management according to the routine clinical treatment.
Publication of data and reproducible research
The findings from this study will be presented locally within the hospitals, published in a peer-reviewed journal, and presented at national and international conferences. The datasets analyzed during the current study and statistical code are available from the corresponding author on reasonable request, as is the full protocol.
Availability of data and materials
All data analyses and manuscripts produced will be available on request.
Dropout and discontinuation
Patients may voluntarily withdraw from the study for other treatments or no reason, or if a significant safety event occurs and the investigator deems it necessary to stop the trial, the subject may withdraw. However, participants are not encouraged to withdraw from the study voluntarily, and we will be fully prepared for the possibility of adverse events.
Ethical approval and study registration
The study has been approved by the Ethical Committee of The Fourth Affiliated Hospital Zhejiang University, School of Medicine (Approval NO.: K2023047). Written, informed consent to participate will be obtained from all participants. The study has been registered at the ClinicalTrials.gov website (https://beta.clinicaltrials.gov/study/NCT05840991). The study will follow the recommendations for physicians involved in research on human subjects adopted by the 18th World Medical Assembly, Helsinki 1964, and later revisions.
Protocol amendments
Notifying sponsor and funder first, then the PI will notify the centers, and that a copy of the revised protocol will be sent to the PI to add to the Investigator Site File. Any deviations from the Protocol will be fully documented using a breach report form, and the protocol will be updated in the clinical trial registry.
Discussion
Although elastic bandages and compression stockings have been widely used for compression therapy after thermal ablation of varicose veins, prolonged compression therapy harms patients’ quality of life and finance. With the development of relevant clinical trials, it has been shown that prolonged compression therapy has no significant clinical gain and may be an unnecessary adjunctive treatment after thermal ablation. The target vein occlusion rate is a crucial concern for vascular surgeons, and simplifying the current compression therapy while ensuring the closure of the treated vein will significantly improve the quality of life and compliance of patients after surgery, reduce their economic burden, and help patients return to everyday life as soon as possible. Suppose the effect of short-term compression therapy proves to be non-inferior to long-term compression therapy. In that case, this trial may contribute to future updates of clinical guidelines for compression therapy after thermal ablation of varicose veins.
Trial status
Study Protocol Version 1.0, dated March 15, 2023. Recruitment is ongoing, the first patient was enrolled on May 22, 2023, and recruitment is estimated to be completed on August 31, 2023.
Abbreviations
- HL/S:
-
High ligating/stripping
- RFA:
-
Radiofrequency ablation
- EVLA:
-
Endovenous laser ablation
- UGFS:
-
Ultrasound-guided foam sclerotherapy
- ABI:
-
Ankle-brachial index
- CEAP:
-
Clinical–Etiological–Anatomical–Pathophysiology
- VAS:
-
Visual analog scale
- AVVQ:
-
Aberdeen Varicose Vein Questionnaire
- VCSS:
-
Venous Clinical Severity Score
References
Youn YJ, Lee J. Chronic venous insufficiency and varicose veins of the lower extremities. Korean J Intern Med. 2019;34(2):269–83. https://doi.org/10.3904/kjim.2018.230.
Marsden G, Perry M, Kelley K, Davies AH, Guideline Development Group. Guideline Development Group Diagnosis and management of varicose veins in the legs: summary of NICE guidance. BMJ. 2013;347:f4279. https://doi.org/10.1136/bmj.f4279. (Published 2013 Jul 24).
Santler B, Goerge T. Chronic venous insufficiency - a review of pathophysiology, diagnosis, and treatment. J Dtsch Dermatol Ges. 2017;15(5):538–56. https://doi.org/10.1111/ddg.13242.
Whing J, Nandhra S, Nesbitt C, Stansby G. Interventions for great saphenous vein incompetence. Cochrane Database Syst Rev. 2021;8(8):CD005624. https://doi.org/10.1002/14651858.CD005624.pub4. (Published 2021 Aug 11).
Goodyear SJ, Nyamekye IK. Radiofrequency ablation of varicose veins: Best practice techniques and evidence. Phlebology. 2015;30(2 Suppl):9–17. https://doi.org/10.1177/0268355515592771.
Rehman ZU, Moosa MA. Safety and efficacy of radiofrequency ablation for varicose veins: an initial experience from Pakistan. J Coll Physicians Surg Pak. 2019;29(8):746–8. https://doi.org/10.29271/jcpsp.2019.08.746.
Siribumrungwong B, Noorit P, Wilasrusmee C, Attia J, Thakkinstian A. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg. 2012;44(2):214–23. https://doi.org/10.1016/j.ejvs.2012.05.017.
Poder TG, Fisette JF, Bédard SK, Despatis MA. Is radiofrequency ablation of varicose veins a valuable option? A systematic review of the literature with a cost analysis. Can J Surg. 2018;61(2):128–38. https://doi.org/10.1503/cjs.010114.
Lawaetz M, Serup J, Lawaetz B, et al. Comparison of endovenous ablation techniques, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Extended 5-year follow-up of a RCT. Int Angiol. 2017;36(3):281–8. https://doi.org/10.23736/S0392-9590.17.03827-5.
Epstein D, Onida S, Bootun R, Ortega-Ortega M, Davies AH. Cost-effectiveness of current and emerging treatments of varicose veins. Value Health. 2018;21(8):911–20. https://doi.org/10.1016/j.jval.2018.01.012.
Brittenden J, Cotton SC, Elders A, et al. A randomized trial comparing treatments for varicose veins. N Engl J Med. 2014;371(13):1218–27. https://doi.org/10.1056/NEJMoa1400781.
Teter KA, Kabnick LS, Sadek M. Endovenous laser ablation: a comprehensive review. Phlebology. 2020;35(9):656–62. https://doi.org/10.1177/0268355520937619.
Wallace T, El-Sheikha J, Nandhra S, et al. Long-term outcomes of endovenous laser ablation and conventional surgery for great saphenous varicose veins. Br J Surg. 2018;105(13):1759–67. https://doi.org/10.1002/bjs.10961.
Staubesand J, Seydewitz V. Etudes ultra-structurelles des varices sclérosées [An ultrastructural study of sclerosed varices]. Phlebologie. 1991;44(1):16–36.
Lurie F, Lal BK, Antignani PL, et al. Compression therapy after invasive treatment of superficial veins of the lower extremities: clinical practice guidelines of the American Venous Forum, Society for Vascular Surgery, American College of Phlebology, Society for Vascular Medicine, and International Union of Phlebology. J Vasc Surg Venous Lymphat Disord. 2019;7(1):17–28. https://doi.org/10.1016/j.jvsv.2018.10.002.
National Clinical Guideline Centre (UK). Varicose Veins in the Legs: The Diagnosis and Management of Varicose Veins. London: National Institute for Health and Care Excellence (NICE); 2013.
Elderman JH, Krasznai AG, Voogd AC, Hulsewé KW, Sikkink CJ. Role of compression stockings after endovenous laser therapy for primary varicosis. J Vasc Surg Venous Lymphat Disord. 2014;2(3):289–96. https://doi.org/10.1016/j.jvsv.2014.01.003.
Ye K, Wang R, Qin J, et al. Post-operative benefit of compression therapy after endovenous laser ablation for uncomplicated varicose veins: a randomised clinical trial. Eur J Vasc Endovasc Surg. 2016;52(6):847–53. https://doi.org/10.1016/j.ejvs.2016.09.005.
Bootun R, Belramman A, Bolton-Saghdaoui L, Lane TRA, Riga C, Davies AH. Randomized controlled trial of compression after endovenous thermal ablation of varicose veins (COMETA Trial). Ann Surg. 2021;273(2):232–9. https://doi.org/10.1097/SLA.0000000000003626.
Kankam HKN, Lim CS, Fiorentino F, Davies AH, Gohel MS. A summation analysis of compliance and complications of compression hosiery for patients with chronic venous disease or post-thrombotic syndrome. Eur J Vasc Endovasc Surg. 2018;55(3):406–16. https://doi.org/10.1016/j.ejvs.2017.11.025.
Ayo D, Blumberg SN, Rockman CR, et al. Compression versus no compression after endovenous ablation of the great saphenous vein: a randomized controlled trial. Ann Vasc Surg. 2017;38:72–7. https://doi.org/10.1016/j.avsg.2016.08.008.
Pihlaja T, Romsi P, Ohtonen P, Jounila J, Pokela M. Post-procedural compression vs. no compression after radiofrequency ablation and concomitant foam sclerotherapy of varicose veins: a randomised controlled non-inferiority trial. Eur J Vasc Endovasc Surg. 2020;59(1):73–80. https://doi.org/10.1016/j.ejvs.2019.08.020.
Onwudike M, Abbas K, Thompson P, McElvenny DM. Editor’s choice - role of compression after radiofrequency ablation of varicose veins: a randomised controlled trial☆. Eur J Vasc Endovasc Surg. 2020;60(1):108–17. https://doi.org/10.1016/j.ejvs.2020.03.014.
Al Shakarchi J, Wall M, Newman J, et al. The role of compression after endovenous ablation of varicose veins. J Vasc Surg Venous Lymphat Disord. 2018;6(4):546–50. https://doi.org/10.1016/j.jvsv.2018.01.021.
Chan AW, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. https://doi.org/10.1136/bmj.e7586. (Published 2013 Jan 8).
Faiz KW. VAS–visuell analog skala [VAS–visual analog scale]. Tidsskr Nor Laegeforen. 2014;134(3):323. https://doi.org/10.4045/tidsskr.13.1145.
Garratt AM, Macdonald LM, Ruta DA, Russell IT, Buckingham JK, Krukowski ZH. Towards measurement of outcome for patients with varicose veins. Qual Health Care. 1993;2(1):5–10. https://doi.org/10.1136/qshc.2.1.5.
De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs [published correction appears in Eur J Vasc Endovasc Surg. 2022 Aug-Sep;64(2-3):284-285]. Eur J Vasc Endovasc Surg. 2022;63(2):184–267. https://doi.org/10.1016/j.ejvs.2021.12.024.
Morrison N, Gibson K, McEnroe S, et al. Randomized trial comparing cyanoacrylate embolization and radiofrequency ablation for incompetent great saphenous veins (VeClose). J Vasc Surg. 2015;61(4):985–94. https://doi.org/10.1016/j.jvs.2014.11.071.
Morrison N, Gibson K, Vasquez M, et al. VeClose trial 12-month outcomes of cyanoacrylate closure versus radiofrequency ablation for incompetent great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2017;5(3):321–30. https://doi.org/10.1016/j.jvsv.2016.12.005.
Beteli CB, Rossi FH, de Almeida BL, et al. Prospective, double-blind, randomized controlled trial comparing electrocoagulation and radiofrequency in the treatment of patients with great saphenous vein insufficiency and lower limb varicose veins. J Vasc Surg Venous Lymphat Disord. 2018;6(2):212–9. https://doi.org/10.1016/j.jvsv.2017.09.010.
Sponsor
Sponsor: The Fourth Affiliated Hospital of Zhejiang University, School of Medicine and Sir Run Run Shaw Hospital of Zhejiang University School of Medicine. The sponsors played no part in the study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
Contact name: Mr. YZ
Address: N1 Shangcheng Avenue, Yiwu City, Zhejiang Province
Email: srrshzyf@zju.edu.cn.
Organizational structure and responsibilities
Principal Investigator and Research Physician
Preparation of protocol and revisions
Preparation of CRFs [Case Report Forms]
Organizing steering committee meetings
Managing CTO [Clinical Trials Office]
Publication of study reports
Members of TMC [Trial Management Committee]
Steering committee (SC)
All lead investigators will be steering committee members.
Agreement of final protocol
Recruitment of patients and liaising with the principal [sic] investigator
Reviewing the progress of the study and if necessary, agreeing to changes to the protocol and/or investigators’ brochure to facilitate the smooth running of the study.
Trial Management Committee (TMC)
Organization of steering committee meetings
Provide annual risk report MHRA [Medicines and Healthcare Products Regulatory Agency] and ethics committee
SUSAR [Serious unexpected suspected adverse events] reporting to MHRA and Roche
Responsible for trial master file
Advice for lead investigators
Audit 6-month feedback forms and decide when the site visit to occur
Assistance with international review, board/independent ethics committee applications
Data verification
Data Manager
Information will be entered by Epidata 3.1 in pairs
Data verification
Lead Investigators
In each participating center, a lead investigator (vascular surgeon) will be identified as responsible for the identification, recruitment, data collection, and completion of CRFs, along with follow-up of study patients and adherence to study protocol. Lead investigators will be steering committee members
Funding
This study will receive funding from the Zhejiang Medical and Health Technology Project (2022ZH036). The funder played no part in the study design; collection, management, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
Author information
Authors and Affiliations
Contributions
MT, WJ, JH, MJ, and YZ conceived and designed the study. MJ provided statistical expertise in clinical trial design. MT, WJ, JH, MJ, and YZ wrote the manuscript. LL, SD, YZ, ZL, and MQ participated in discussing and modifying the protocol. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mingjun Tang, Weihua Jiang and Jin Hong are co-first authors.
Supplementary Information
Additional file 1.
SPIRIT Checklist for Trials.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tang, M., Jiang, W., Hong, J. et al. Effect of short-term compression therapy after thermal ablation for varicose veins: study protocol for a prospective, multicenter, non-inferiority, randomized controlled trial. Trials 24, 669 (2023). https://doi.org/10.1186/s13063-023-07609-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-023-07609-1