Abstract
Background
Obesity represents a growing threat to health with multiple negative impacts including urinary incontinence. Pelvic floor muscle training (PFMT) is the first line of treatment for urinary incontinence. Both surgical and conservative weight loss results in improvement of urinary incontinence reports in obese women and we hypothesize that a low-calorie diet in combination with PFMT would result in additional beneficial effects to urinary symptoms in women with UI compared would with weight loss alone.
Objective
To assess the effect of a low-calorie diet plus PFMT protocol in obese women’s urinary incontinence reports.
Methods
This is a protocol for a randomized controlled trial that will include obese women reporting UI and being able to contract their pelvic floor muscles. The participants will be randomly allocated in two groups: group 1 will participate in a 12-week protocol of low-calorie diet delivered by a multi-professional team at a tertiary hospital; group II will receive the same low-calorie diet protocol during 12 weeks and will additionally participate in 6 group sessions of supervised PFMT delivered by a physiotherapist. The primary outcome of the study is self-reported UI, and severity and impact of UI on women’s quality of life will be assessed by the ICIQ-SF score. The secondary outcomes will be adherence to the protocols assessed using a home diary, pelvic floor muscle function assessed by bidigital vaginal palpation and the modified Oxford grading scale, and women’s self-perception of their PFM contraction using a questionnaire. Satisfaction with treatments will be assessed using a visual analog scale. The statistical analysis will be performed by intention to treat and multivariate analysis of mixed effects will be used to compare outcomes. The complier average causal effects (CACE) method will be used to assess adherence. There is an urgent need for a high-quality RCT to investigate if the association of a low-calorie diet and PFMT can provide a larger effect in the improvement of urinary incontinence reports in women with obesity.
Trial registration
Clinical Trials NCT04159467. Registered on 08/28/2021.
Similar content being viewed by others
Introduction
Currently, the number of obese people in the world represents a growing threat to the health of populations, both in developed and developing countries [1]. According to the World Health Organization (WHO), in 2016, more than 1.9 billion adults aged 18 and over were overweight. Of these, more than 650 million adults were obese. In 2016, 39% of adults aged 18 and over (39% of men and 40% of women) were overweight. Overall, about 13% of the world’s adult population (11% of men and 15% of women) was obese in 2016 [2]. In addition to metabolic diseases, obesity can cause musculoskeletal disorders, including pelvic floor muscle disorders, the most prevalent of which is urinary incontinence (UI) [3,4,5].
Pelvic floor muscle training (PFMT) is considered the first-line treatment of all types of non-neurogenic urinary incontinence (UI) in women [6]. Studies have shown the positive effect of weight loss, mediated by a low-calorie diet on UI symptoms in women [7,8,9] but few current randomized controlled trials (RCT) have been found comparing the improvement in UI symptoms in women who have just undergone a low-calorie diet for weight loss compared to a low-calorie diet associated with PFMT.
Considering that obesity is currently among the most worrying health problems in the world, contributing to PFM dysfunctions such as UI, it is urgent to investigate in high-quality RCTs new low-risk interventions capable to optimize the results obtained only with weight loss, in the reduction of reports of UI in obese women.
Methods
Study design
We will conduct an assessor blind randomized, controlled, two-arm clinical trial to assess whether the combination of a low-calorie diet and PFMT will optimize the results obtained with diet therapy as a single intervention to decrease UI prevalence reports and severity in obese women (primary outcome). The secondary outcomes of this study are the impact of the protocol on PFM function, women’s self-perception of their PFM, adherence, and satisfaction with the treatment. This protocol will be reported according to the Protocol Items Standard: Recommendations for Intervention Trials checklist (SPIRIT) 2013: items recommended for a clinical trial protocol and related documents. It is a superiority trial.
Ethic
The study was approved by the Human Research Ethics Committee of the University of São Paulo—Hospital das Clínicas of the Ribeirão Preto Medical School (HCFMRP / USP) No. 16379919.5.0000.5440 on July 9, 2019, and registered in the Clinical Trials—NCT04159467.
Any major deviation or modification of the original protocol will be reported in the Clinical Trials website and the trial records will be continuously updated as necessary.
The risks of this research basically include the possible embarrassment of the participant in answering questions related to symptoms of urinary incontinence, intestinal and vaginal pain, and embarrassment during the physical examination (vaginal palpation), in addition to feeling some discomfort during the examination and of the possible breach of confidentiality during the research.
The benefits of this research are that the participant will receive information about the anatomy of the pelvic floor, its functions, and dysfunctions, she will learn to contract this musculature and know if she is doing it correctly, contributing to prevent and/or treat its dysfunctions, in addition to also receiving a program of training for 12 weeks (if selected for group II) to strengthen the pelvic floor muscles. If you are selected for group I, you will be invited after 12 weeks to receive the same treatment as in group II.
For ethical reasons, we did not plan to prohibit any concomitant treatment. We included in the methods section our plan to monitor any concomitant treatment for pelvic floor disorders including urinary incontinence, but we expect to have homogeneous groups in relation to these variables provided by an adequate randomization and sample size.
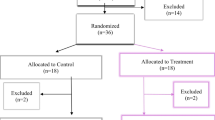
Figure 1 shows the CONSORT (Consolidated Standards of Reporting Trials) flowchart, enrollment schedule, interventions, and study evaluations. Figure 2 shows the checklist using the SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) used in the study.
Participants
Obese women with UI who are about to start a low-calorie diet program for weight loss will be recruited in the bariatric surgery sector at the Clinics Hospital of Ribeirão Preto Medical School (HCFMRP-USP).
Inclusion criteria
Women over 18 years, with a body mass index (BMI) > 30 kg/m2; reporting stress urinary incontinence, urgent urinary incontinence, or mixed urinary incontinence in the past 4 weeks assessed by the ICIQ-SF; who are able to contract the pelvic floor muscles (assessed using vaginal palpation with a PFM contraction ≥ 2 according to the modified Oxford grading scale); and without any cognitive impairment.
Exclusion criteria
The participants will be excluded of the study if they withdraw their consent to participate in the study or if they become pregnant.
Criteria of discontinuing
The criteria of discontinuing the trial for a given participant include withdrawal of consent to participate and becoming pregnant during the study.
Sample size calculation
The sample calculation was estimated considering a significance level of 5%, power of 20%, and difference of 4 points on the final score of the primary outcome, ICIQ-SF, between groups at the end of treatment [10]. The value of 4 points is equivalent to the minimum value for change in the questionnaire score. Thus, the sample will be composed of 22 participants.
Statistical analysis
Data will be de-identified, encoded, and stored in the database using the Excel Program. The software SPSS 22.0 will be used for the analysis of data. The description of quantitative variables will be expressed in mean, standard deviation, minimum value, median and maximum value. Qualitative variables will be described in absolute and relative values (%). A 95% confidence interval and 0.05 significance will be considered for all tests. Both per-protocol and intention-to-treat analyses will be performed.
A linear mixed-effect model will be used to analyze the ICIQ-SF score. In the reassessment, individuals’ values will be considered random effects, and the groups, the times, and the interaction between them will be regarded as fixed effects. In addition, the McNemar test will verify changes in categories variables before and after the intervention. Both per-protocol analysis [11,12,13] and an intention-to-treat analysis will be also conducted.
Randomization and blinding process
An assistant researcher specially trained will be responsible only for recruiting the participants to enter the study and will give them all the information about the study, obtaining their written consent in case they agree to participate.
An assistant researcher not involved with the recruitment, intervention and assessment will generate the allocation sequence. The participants will be allocated in a group that will receive a low-calorie diet for weight loss (group I) or in another group that will receive diet + PFMT (group II). Randomization will be carried out using a computational list of random numbers and will be concealed (by means of a sealed brown envelope). Women’s data will be kept only with the assistant researcher not involved with other parts of the research process to process to protect confidentiality before, during, and after the intervention. The trial is an assessor blinded in relation to the pelvic floor muscle assessment.
The senior researcher who is not involved with the recruitment, intervention delivery, and assessment will have access to the trial data. We have planned to submit the manuscript to an open-access journal that makes all data available to readers as an appendix or under request.
Figure 1 shows the flowchart for selecting women for the randomized clinical trial, following the CONSORT.
Intervention
Women randomized to Group 1 will receive counseling from the hospital staff. They will attend 3 meetings (once a month), where a multi-professional team from the bariatric surgery outpatient clinic will address different topics related to nutrition including advice on the quality of food, mindful eating, identification of signs of hunger and satiety, and emotional triggers that lead to emotional eating. In addition, each participant will undergo individual nutritional assistance to assess food consumption, anthropometric measures, and body composition and will receive more specific guidelines on nutrition and an individualized low-calorie diet and monitoring. Outpatient care will last 12 weeks and women in this group will not receive instructions and a supervised PFMT protocol, however for ethical reasons, after the data collection is finished women belonging to this group will be invited to receive six supervised sessions of PFMT and will receive the same booklet of exercises on PFMT delivered to group II.
The participants randomized to group II will also receive the same counseling related to nutrition and also an individualized low-calorie diet given by the hospital staff; additionally, they will participate in six face-to-face physiotherapy sessions supervised by a physiotherapist in groups of a maximum of 10 participants, for 12 weeks in interspersed weeks.
In the weeks when there is no face-to-face supervised session, the same physiotherapist will encourage home PFMT by phone, calling each participant of Group II only. An intensive PFMT will be encouraged by the physiotherapist. The PFMT protocol will consist of 4 sets of ten maximum perceived voluntary contractions sustained for 6 s with a 6-s resting period between the contractions. At the end of a series of 10 contractions, five rapid contractions of the PFM will be performed. Two minutes interval will be given between each set performed.
The sets will be performed only in two positions at the face-to-face supervised sessions at the hospital: sitting and standing (2 sitting sets + 2 standing sets). The participants of this group will be instructed to perform PFMT at home at least three times a week, except on the days of supervised training. They will be instructed to follow the booklet given to them in the first meeting, in addition to the fortnightly adherence diary to the exercises to be filled weekly. Participants will also be instructed on how to perform the “the knack” maneuver, which consists of repeatedly contracting their PFM before any increase in intra-abdominal pressure during daily activities [14]. Women will also be instructed to repeatedly contract their PFM when they feel urgency. Women will fill a diary about their adherence to PFMT, and there will be a place where they are asked about any side effects or bother related to the intervention. At the last assessment, they are asked about again about any unintended effects related to the trial intervention. The type and number of unintended effects will be fully reported as an important result of the trial. Although adverse effects of these type of intervention is not very common or severe, all the participant is assured they can discontinue their participation at any time for any reason, including any adverse effects (Table 1). Table 1 presents detailed information about the protocol of intervention.
Assessment
Primary outcome measures
Self-report of urinary incontinence will be measured by question 3 of the ICIQ-SF. Women will be considered incontinent if they choose options 1, 2, 3, 4, or 5 of question 3. Women will be considered continent if they choose option 0 in question 3.
The severity and impact of urinary incontinence on women’s quality of life will be measured by the ICIQ-SF score.
Other outcome measures
The adherence to home PFMT sessions will be monitored by the physiotherapist from a diary where women will register their adherence to home training. This diary will be attached to the leaflet that will be given to women in the first session. The diary will be collected by the physiotherapist every fortnight.
The PFM function will be assessed using vaginal palpation by a trained physiotherapist who will not be involved with the intervention and will not be aware of women’s allocation in the groups. Before the start of the palpation exam, the woman will receive detailed information about the anatomy, function, and dysfunction of the PFM and how to contract them correctly. The evaluation will be carried out with the participant in the supine position with the hip and knee semi-flexed. The participant will be asked to pull their PFM in and up as hard as possible, and then she will be instructed to relax them completely. Contraction of PFM will be classified as absent or present. The ability to contract the PFM will be considered present when there is occlusion and/or occlusion and elevation of the PFM towards the pubic symphysis and absent when there is no perceived internal movement. Additionally, muscle contraction will be graded according to the Modified Oxford Grading Scale (MOGS) [15, 16]. Contractions of muscles such as gluteus, adductor, and abdominal will be discouraged by the examiner.
Self-perception of women’s PFM contraction will be assessed at the time of the physical evaluation when the examiner will ask the participant if she feels she is able to contract her PFM and she will be asked to estimate the intensity of her PFM according to the MOGS that will be presented to her [17].
Participants’ subjective satisfaction with the treatment will be measured by the visual analog scale (VAS), which is an estimate on a numerical scale where 0 represents no satisfaction at all and 10 means the maximum possible satisfaction with the treatment.
In relation to satisfaction with the interventions, participants will be asked to answer the following questions: “Are you satisfied with the treatment you received for UI?”, “Would you do this treatment again?”, “Would you recommend this treatment?”, “Would you pursue another treatment?”. The options of answers to these questions are yes or no.
In order to identify barriers to treatment, the participants will be asked to answer the following questions: “Do you identify any barriers or difficulties in adhering to the treatment you received for urinary incontinence? If any please list the barriers.”
Descriptive and control variables
The descriptive and control variables were divided into clinical variables (diabetes, hypertension, constipation, number of pregnancies, deliveries, cesarean sections, vaginal delivery; use of contraceptives and previous pelvic surgeries) sociodemographic variables (age, education, marital status, economic, smoking occupation, use of alcoholic beverages, physical exercise and use of caffeine) and anthropometric measures (height and body mass). The descriptive and control variables will be acquired from women’s self-report. The study variables are shown in Fig. 2 and Table 2.
Data collection
The data will be collected in an interview format using a self-reported validated questionnaire and PFM exam. A trained assistant researcher will conduct an interview and a PFM assessment. All assessments will be performed (at baseline) and after 12 weeks for both groups and will be performed by the same researcher that will be blind about women’s group allocation.
Discussion
We presented a protocol of a RCT that will investigate the efficacy of a 12-week pelvic floor muscle training (PFMT) program added to a low-calorie diet on obese women with urinary incontinence (UI) reports. In the literature, the benefits of weight loss to improve UI is established by the literature [6] but it is yet to be evidenced if PFMT could increase the effectiveness of weight loss on UI reports in obese women.
Weight loss, both mediated by surgical and conservative interventions, is effective to improve all types of non-neurological UI (stress, urgency, or mixed) [18, 19]. In fact, a loss of 5 to 10% of weight provides a significant improvement in UI complaints, and weight loss is considered a first-line therapy.
High obesity rates are a current global reality and reports of UI by this population have a high prevalence. When compared to a normal body mass index, overweight was associated with a one-third increase in the risk of UI (relative risk = 1.35, 95% confidence interval = 1.20–1.53), while the risk was doubled in obese women (relative risk = 1.95, 95% confidence interval = 1.58–2.42).
On the other hand, weight loss will not provide an active improvement of PFM function as PFMT, the gold standard physiotherapy intervention to treat non-neurogenic UI in women. The updated Cochrane review on this topic included randomized and quasi-randomized controlled trials investigating the effect of PFMT on UI in women. The search produced 1299 records, from which 94 potentially relevant full-text articles were retrieved. The inclusion of new studies in this updated review reinforced the results showing the effectiveness of PFMT in the treatment of any type of non-neurogenic UI in women [20].
In planning our RCT protocol, we considered what is already known from the literature to optimize the PFMT effectiveness having in mind that is essential to provide a high-quality intervention based on exercise physiology. We will include only women who are able to contract their PFM, providing education to them related to PFM function, dysfunction, and how to contract correctly their PFM as part of our intensive and supervised PFMT protocol.
RCTs investigating a low calory diet associated to PFMT including only obese women are rare in the literature. One small RCT (n= 22) included both overweight and obese women and was different from our RCT compared PFMT + weight loss with a group receiving only PFMT. The study did not show the benefits of adding weight loss to PFMT. However, the limited sample size and the short duration of the protocol (8 weeks) might have importantly contributed to the lack of effect [10].
A recently published study aimed to implement and evaluate the feasibility, acceptability, and effectiveness of a 12-week group exercise and healthy eating program (ATHENA) both for overweight/obese women with UI [21]. The results indicated that ATHENA was feasible to implement, with a high percentage of women (97%) reporting improved UI symptoms and significant improvements in pelvic floor dysfunction and quality of life. No significant weight change was observed although significant improvements were found in body-food choice congruence. Different from the protocol planned for our study, the program investigated included only education about health eating that might have not is enough to provide weight loss. Nevertheless, these results are limited to provide a reliable answer related to the effectiveness of the intervention, as this is not a RCT.
It seems urgent to conduct high-quality RCTs to investigate the efficacy of associating PFMT with weight loss mediated by diet therapy. The protocol of this RCT was carefully planned following the quality criteria to enhance optimal internal e external validity. Additionally, we will investigate the impact of the intervention on women’s adherence to treatment, on their self-perception of their PFM, and satisfaction with the treatment. Brazilian women’s knowledge about PFM function and dysfunction is low [22, 23]. PFMT protocol must include an education component about PFM function not only to increase women’s knowledge about it but also to improve their adherence to treatment [24, 25]. We will also have the chance to identify barriers and facilitators related adherence to the proposed interventions. A recent study has shown that women with worse PFM function tend to overestimate their PFM function [13]. The self-perception of the PFM function is important for women to localize and to exercise their PFM. Another innovation of this RCT will be to analyze the impact of the intervention with and without PFMT in women’s self-perception of their PFMT and our hypothesis is that more women in the group receiving PFMT in addition to low-calorie diet will improve their PFM perception compared to the group receiving only low-calorie diet.
Trials status
Recruitment has not yet started because the patients are in the risk group for COVID-19 and, therefore, the clinic has temporarily suspended the appointments.
References
Ministry of Health (MH). Health Care Secretariat. Primary Care Department. Obesity. Brasília: MS; 2006.
World Health Organization (WHO). Obesity and overweight. Accessed on 21 Sept 2018.
Lamerton TJ, Torquati L, Brown WJ. Overweight and obesity as major, modifiable risk factors for urinary incontinence in young to mid-aged women: a systematic review and meta-analysis. Obes Rev. 2018;19:1735.
Ebbesen MH, Hunskaar S, Rortveit G, Hannestad YS. Prevalence, incidence and remission of urinary incontinence in women: longitudinal data from the Norwegian. BMC Urol. 2013;13:27.
Nygaard CC, Schreiner L, Morsch TP, Saadi RP, Figueiredo MF, Padoin AV. Urinary incontinence and quality of life in female patients with obesity. Braz J of Gynecol and Obst. 2018;40(9):534–9.
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654.
Shih E, Hirsch H, Thacker HL. Medical Management of urinary incontinence in women. Clevel Clin J of Med. 2017;84(2):151–8.
Wing RR, West DS, Grady D, Creasman JM, Richter HE, Myers D. Effect of weight loss on urinary incontinence in overweight and obese women: results at 12 and 18 months. J Urol. 2010;184:1005–10.
Wing RR, Creasman JM, West DS, Richter HE, Myers D, Burgio KL. Improving urinary incontinence in overweight and obese women through modest weight loss. Obstet Gynecol. 2010;116:284–92.
de Oliveira MCE, de Oliveira de Lima VC, Pegado R, Silva-Filho EM, Fayh APT, Micussi MT. Comparison of pelvic floor muscle training isolated and associated with weight loss: a randomized controlled trial. Arch Gynecol Obstet. 2019;300(5):1343–51.
Little R, Yau L. Statistical techniques for analyzing data from prevention trials: treatment of no-shows using Rubin’s causal model. Psychol Methods. 1998;3:147–59.
Jo B. Statistical power in randomized intervention studies with noncompliance. Psychol Methods. 2002;7:178–93.
Little RJ, Rubin DB. Causal effects in clinical and epidemiological studies via potential outcomes: concepts and analytical approaches. Annu Rev Public Health. 2000;21(1):121–45.
Miller JM, Miller JAA, DeLancey JOL. A pelvic muscle precontraction can reduce cough-related urine loss in selected women with Mild SUI. J Am Geriatr Soc. 1998;46:870–4.
Pena CC, Bø K, de la Ossa AMP, Fernandes ACNL, Aleixo DN, de Oliveira FMF, Ferreira CHJ. Are visual inspection and digital palpation reliable methods to assess ability to perform a pelvic floor muscle contraction? An intra-rater study. Neurourol Urodyn. 2021;40(2):680–7.
Laycock J, Jerwood D. Development of the Bradford perineometer. Physiotherapy. 1994;80:139–42.
Uechi N, Fernandes ACNL, Bø K, de Freitas LM, de la Ossa AMP, Bueno SM, Ferreira CHJ. Do women have an accurate perception of their pelvic floor muscle contraction? A cross-sectional study Neurourol Urodyn. 2020;39(1):361–6.
Yazdany T, Jakus-Waldman S, Jeppson PC, et al. for the American Urogynecologic Society American Urogynecologic Society Systematic Review: the impact of weight loss intervention on lower urinary tract symptoms and urinary incontinence in overweight and obese women. Female Pelvic Med Reconstr Surg. 2020;26(1):16–29.
Montenegro M, Slongo H, Juliato CRT, et al. The Impact of bariatric surgery on pelvic floor dysfunction: a systematic review. J Minim Invasive Gynecol. 2019;26:816–25.
Cacciari LP, Dumoulin C, Hay-Smith EJ. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: a cochrane systematic review abridged republication. Braz J Phys Ther. 2019;23(2):93–107.
Howard Z, Ross L, Weir KA, Baker N, Smith L, Nucifora J, Townsend H, Roberts S. A group program for overweight and obese women with urinary incontinence (ATHENA): an implementation-effectiveness hybrid type 3 study. Int Urogynecol J. 2022;33(4):991–1000. https://doi.org/10.1007/s00192-021-04743-9.
Fante JF, Silva TD, Mateus-Vasconcelos ECL, Ferreira CHJ, Brito LGO. Do women have adequate knowledge about pelvic floor dysfunctions? A systematic review. Rev Bras Ginecol Obstet. 2019;41(8):508–19.
de Freitas LM, Bø K, Fernandes ACNL, Uechi N, Duarte TB, Ferreira CHJ. Pelvic floor muscle knowledge and relationship with muscle strength in Brazilian women: a cross-sectional study. Int Urogynecol J. 2019;30(11):1903–9.
de Andrade RL, Bø K, Antonio FI, Driusso P, Mateus-Vasconcelos ECL, Ramos S, Julio MP, Ferreira CHJ. An education program about pelvic floor muscles improved women’s knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: a randomised trial. J Physiother. 2018;64(2):91–6.
Fernandes ACNL, Palacios-Ceña D, Hay-Smith J, Pena CC, Sidou MF, de Alencar AL, Ferreira CHJ. Women report sustained benefits from attending group-based education about pelvic floor muscles: a longitudinal qualitative study. J Physiother. 2021;67(3):210–6.
Acknowledgements
We thank the Hospital of Clinics (HC) and the University of Sao Paulo for assistance and support. We also thank the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) for the student grant.
Funding
Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) (Finance Code 001).
Author information
Authors and Affiliations
Contributions
PCSM conceived the study, initiated the study design, developed the methodology, and commented on the initial drafts of the manuscript. CHJF conceived the study, initiated the study design, developed the methodology, and commented on the initial drafts of the manuscript. TdBF initiated the study design, developed the methodology, and commented on the initial drafts of the manuscript. PD commented on the initial drafts of the manuscript. MFCC initiated the study design and developed the methodology. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Research Ethics Committee of the University of São Paulo—Hospital of Clinics of the Ribeirão Preto Medical School (HCFMRP / USP) No. 16379919.5.0000.5440 on July 9, 2019, and registered in the Clinical Trials—NCT 04159467. Written informed consent will be obtained from all participants in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
SPIRIT 2013 Checklist: recommended items to address in a clinical trial protocol and related documents*.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mendes, P.C.S., Fretta, T.B., Camargo, M.F.C. et al. Effect of pelvic floor muscle training on reports of urinary incontinence in obese women undergoing a low-calorie diet before bariatric surgery — protocol of a randomized controlled trial. Trials 24, 376 (2023). https://doi.org/10.1186/s13063-023-07347-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-023-07347-4