Abstract
Background
The COVID-19 pandemic—with its first reported case in Sri Lanka in March 2020—had the potential to impact the risk of re-establishing malaria, a disease which was eliminated from Sri Lanka in 2012. Post-elimination, the country remains highly vulnerable to a return of malaria on account of high vector mosquito densities and the inflow of imported malaria cases.
Methods
Parallels between COVID-19 and malaria after its elimination as health security threats were drawn, and the many ways in which the COVID-19 pandemic impacted the prevention of re-establishment of malaria programmes in the country in 2020 were examined. The implications of this experience for global health security are analysed.
Results
In 2020, imported malaria cases were fewer than in the previous 3 years, due to restrictions on international travel. Yet, a high level of malaria case and entomological surveillance was sustained through surveillance strategies modified to focus on quarantine centers, in response to the pandemic. As a result, more imported malaria cases were detected by active case detection than by passive surveillance. Some of the operational shifts adopted by the Anti Malaria Campaign were moving rapidly into functioning as an intersectoral player by reinforcing its collaborations with the Ministries of Aviation and Defense, switching to the use of online communication systems, and integrating and synergizing its field activities with the COVID-19 control programme.
Conclusions
The experience highlights the need for disease control programmes to be agile, flexible and responsive, and underscores the importance of maintaining even a lean focal programme for diseases such as malaria after they have been eliminated. Sustaining public health leadership and robust technological capacities in communication and data management were paramount in preventing the disruption of the malaria prevention programme during the pandemic and sustaining the malaria-free status of the country.
Similar content being viewed by others
Background
Sri Lanka eliminated malaria, reporting the last case of indigenous malaria in 2012, and received certification by the World Health Organization (WHO) in 2016 [1]. Due to the high prevalence of malaria vectors in the country and a steady inflow of imported malaria cases, the country remains at a very high risk of malaria being re-established [2]. Therefore, a rigorous programme to prevent the re-establishment of malaria is being conducted by the Anti Malaria Campaign (AMC), which is a special programme within the Ministry of Health. Post-elimination, Sri Lanka has remained free of indigenous malaria except for a case of introduced malaria (infection transmitted locally from an imported case) in 2018 [3] and a case of transfusion-induced-malaria in 2021 [4].
In 2020, the COVID-19 pandemic caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and its devastating impact worldwide raised acute awareness of the need for enhanced global health security. Only two decades ago, malaria in Sri Lanka was a major part of the unfinished agenda of infectious disease elimination, but now, after its elimination in 2012, it is a disease at risk of being re-established through importation. Thus, the Prevention of Re-establishment (PoR) of malaria programme is itself reliant on effective health security [5]. It constitutes a parallel example to COVID-19 in the current global discussions on health security [6]. Furthermore, the COVID-19 pandemic also had the potential to impact on the PoR programme for malaria in Sri Lanka in many and diverse ways. Restriction of human movement due to country and area lockdowns and curfews being imposed from time to time; the possibility of having human and financial resources moved away from malaria for COVID-19 control; and the potential of the global pandemic to interfere with procurement of essential commodities were some of the ways in which the malaria PoR programme could have been compromised [7]. However, the COVID-19 pandemic may have also led to a reduction in risk of malaria importation to the country on account of airport closures and restrictions on the arrival of people to the country, which is the principal route of population movement and parasite introduction.
This paper addresses how these complex processes played out, and the resulting impact of the COVID-19 pandemic on the malaria PoR programme in Sri Lanka. It reports on how innovation and adaptation on the part of the AMC and its Regional Malaria Offices (RMOs) kept the country malaria-free amidst the pandemic despite importation of malaria. It also analyses the elements of health security essential to deal with global health threats based on Sri Lanka’s experience with COVID-19 and malaria.
Methods
COVID-19 surveillance data
COVID-19 data were obtained from the Ministry of Health, Sri Lanka. All reported cases in Sri Lanka during the period of the study, March to December 2020, were based on reported COVID-19 cases.
Malaria data
Malaria data from January 2017–December 2020 were sourced from the databases of the AMC, which record confirmed malaria cases and the mode and place of detection. The details of the AMC’s operations, including district level data and the collaborations of the AMC with other sectors and departments within other ministries were captured in the AMC records which are updated every month over time.
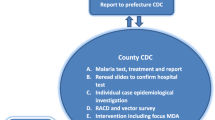
Malaria case surveillance
A cornerstone of the PoR strategy in Sri Lanka is case and entomological surveillance and response. Case surveillance is based on three strategies: passive case detection (PCD), reactive case detection (RACD) and proactive case detection (PACD) [8]. PCD is the detection of cases when patients present on their own accord to the health care system with symptoms suggestive of malaria and are screened for malaria by the attending health worker. RACD is the screening of high-risk individuals and groups prompted by an index case (e.g., those living in the same neighborhood or travel companions of an index case of malaria). PACD is defined as the screening of known high-risk groups, unrelated to an index case of malaria.
Entomological surveillance for malaria
As an integral component of the PoR strategy, the AMC routinely conducts several entomological surveillance operations as follows: (1) at pre-determined sentinel sites, (2) by way of proactive surveillance operations at selected sites deemed to be at high risk, and (3) reactive surveillance when a case of malaria is detected, in areas surrounding the residence of and places inhabited by the patient [9].
Results
The COVID-19 epidemic in Sri Lanka
The COVID-19 epidemic in Sri Lanka which began in March 2020 was well controlled until end-September of that year. With the exception of three clusters which led to spikes of cases in April, May and July, all of which were effectively controlled, the daily incidence of new cases of COVID-19 was kept well below 100 in the population of 21 million (Fig. 1) [10]. This was achieved through testing, stringent contact tracing and quarantining, implemented through a close collaboration between the Ministries of Health and Defense, combined with the mandatory wearing of face masks, social distancing and strict personal hygiene, which remained enforced throughout 2020 [11]. A countrywide lockdown was imposed on 20th March and lasted until 27th April when it was lifted in some of the COVID-19-free districts, but in others the lockdown continued until 4th May 2020 [11]. The two international airports in the country were closed for incoming flights from 17th March 2020 except for flights bringing Sri Lankan nationals who had been stranded overseas [12]. The airport remained closed for regular international traffic up to about middle of October after which limited travel was permitted for organized tourism—an experiment in which a “bubble” concept was applied to small groups of tourists who were allowed to enter the country for a controlled passage of tours under strict surveillance [13]. Although organized tourism was not a success, the airports were opened for normal traffic in January 2021.
Until September 2020, as much as a third of COVID-19 cases were reported among arrivals to the country from overseas, both foreigners and Sri Lankan repatriates. At the end of September 2020, a large outbreak of COVID-19 among factory workers saw the beginning of a rapid and sustained increase of cases, which was less responsive to the rigorous control measures that were being applied [10]. The COVID-19 epidemic worsened in early October 2020, leading to case numbers doubling every month during the last 3 months of the year and peaking at a daily incidence of over 600 cases per day and remained so up to the end of the study period (Fig. 1). As of 31st December 2020, a total of 42,702 cases of COVID-19 were reported from 1,250,417 real-time PCR tests. During the last 3 months of the year, 95% of reported COVID-19 cases were in resident Sri Lankan nationals, indicating massive community spread [10].
Only thirteen deaths due to COVID-19 were reported up to 14th October 2020. However, since then, in the face of the heightened epidemic, COVID-19 deaths as well as the case fatality rate began to increase. A total of 199 COVID-19 deaths were reported through the end of December 2020.
Malaria during the COVID-19 pandemic in 2020
All malaria cases reported in 2020 were imported, as they were in almost all previous years since malaria was eliminated in 2012. The number of imported malaria cases was lower in 2020 than in previous years, at 30 total cases compared to the 3-year period 2017–2019, when 57, 48 and 53 cases, respectively, were reported (Table 1).
The number of overseas arrivals in the country in 2020 (1.1 million) was reduced to about a fifth of that of the three previous years 2017–2019 (average 5.1 million per year) (Table 1). Of the arrivals in 2020, at least 5790 (0.52%) were known to have arrived from malaria endemic countries, and 95% of those who came from malaria endemic countries were Sri Lankan nationals who returned home due to the COVID-19 pandemic.
Although imported malaria case numbers fluctuated monthly over the past few years (2017–2019) there has been a general trend of higher cases during the first and last few months of the year, corresponding to the peak of travel for holidays and return of Sri Lankans employed overseas (Fig. 2). This trend was not evident in 2020; instead, a spike of cases was seen in June and July, corresponding to the peak in repatriation of Sri Lankans living overseas owing to the COVID-19 pandemic (Fig. 2).
Findings on malaria PoR operations during the COVID-19 epidemic
Malaria case surveillance
From the beginning of the COVID-19 epidemic, working arrangements were made between the AMC and the Ministries of Defence, Airports and Aviation, and Foreign Affairs which coordinated the arrival of passengers, including repatriates, to the country and arranged for quarantine and COVID-19 testing. Screening incoming travelers from malaria endemic countries while they were in quarantine centers was made possible through a well-coordinated arrangement between many sectors: the military operations center, which was in charge of repatriation, informed the AMC of all incoming flights and their passenger lists, where they were coming from and when they were arriving, as well as the location of the centers where incoming passengers were to be quarantined. The AMC then informed the RMOs of the relevant districts to which passengers would be transferred to quarantine centers, providing them with passenger lists well in advance. Thereafter, the RMOs arranged the screening of those passengers arriving from malaria endemic countries whilst in quarantine in their district.
From March 2020 onwards, the screening of all persons arriving in the country from malaria endemic countries was performed routinely on day 10 of quarantine, irrespective of their having symptoms or not. The collection of blood samples for malaria microscopy was synchronized with that for COVID-19 testing by working closely with the appropriate unit within the Ministry of Health. If any person developed fever whilst in quarantine (s)he was promptly screened for malaria in co-ordination with the COVID-19 testing programme. After the 14-day quarantine period, when people returned to their residences, they were all screened for malaria at 3, 6 and 12 months after arrival regardless of symptoms, and were advised to report to the nearest hospital (where microscopy facilities were available) if they developed symptoms of malaria.
Eighty percent of those who returned from malaria endemic countries in 2020 (n = 4609) were screened for malaria within a week following their arrival. This included screening of 173 Air Force personnel returning from United Nations Peacekeeping Missions in the Central African Republic and South Sudan. The total number of blood smears screened for malaria by all three case surveillance strategies in 2020 (n = 383,922) was significantly lower than in the previous 3 years (average 691,700) (Table 2).
In 2020, 63% of imported malaria cases were detected by PCD, 33% by PACD and 3.3% of cases by RACD. In previous years, a vast majority of cases were detected by PCD: 98%, 100% and 89% of cases in 2017, 2018 and 2019, respectively. Over the same 3-year period, PACD and RACD contributed very little to the detection of imported malaria cases, with, on average, 1.9% and 2.5% of malaria cases detected by PACD and RACD, respectively [8]. Of the 30 imported malaria cases diagnosed and treated during 2020, a third (n = 10; 33%) were detected through screening of arrivals from malaria endemic countries while they were in quarantine centers by PACD.
The proportions of blood smears collected for screening by the different case detection strategies did not change much in 2020 compared to previous years (Table 2; Fig. 3). Therefore, the yield of positives from PACD was very much higher in 2020 compared to that in previous years.
The ways in which malaria operations and the work of the AMC were modified during the COVID-19 epidemic and adapted to the new conditions and restrictions, and their implications and impact are summarized in Table 3.
Malaria case management
The malaria case management procedures were also adapted to the new conditions imposed by the COVID-19 epidemic. In Sri Lanka, all confirmed malaria cases are routinely managed as in-ward hospital patients [14]. In 2020, malaria patients were admitted and managed in isolated hospital wards until a concomitant COVID-19 infection was excluded in the patient. They were screened daily to monitor the malaria blood infection in response to treatment using EDTA blood samples. Patient management was reviewed online by the AMC with regional (district) teams on the ground.
In 2020, all malaria patients were followed up as routinely done in previous years—i.e., microscopy screening on days 7, 14, 21, 28 and 42 for all species, and additionally once a month for 12 months for Plasmodium vivax and Plasmodium ovale infections [15]. All blood screenings for malaria were conducted strictly in accordance with the guidelines for case management of the AMC [14] and conforming to the safety guidelines for the COVID-19 epidemic [7].
Entomological surveillance
In 2020, entomological surveillance operations were affected by the COVID-19 epidemic owing to restrictions imposed on human movement during area lockdowns and also community resistance to the presence of healthcare workers visiting the area. In total, there were fewer entomological surveillance operations performed in 2020 (n = 1184) compared to the previous year 2019 (n = 2039) (Fig. 4). The relative proportions of the different types of surveillance operations remained the same as the previous year (Fig. 5). One major change in 2020 was, however, that the proactive surveillance operations were rapidly moved to the areas surrounding the quarantine centers which (a) housed passengers arriving from malaria endemic countries, and (b) were located in previously malaria endemic regions of the country. This was based on the assumption that quarantine centers were the most likely places to locate malaria infected persons and that previously malarious areas were most receptive to malaria transmission [16]. In previous years, site selection for proactive entomological surveillance operations was based on geographical areas in which high-risk individuals, such as foreign labourers and other returnees from overseas resided [9].
Training, supervision, advocacy and advisory mechanisms
Every year, the AMC conducts several training programmes for its own technical and field staff and for technical staff of other institutions such as the private health sector and the military. These events were greatly reduced in number owing to the COVID-19 pandemic control guidelines issued by the Ministry of Health. Of 15 microscopy training events for Public Health Laboratory Technicians scheduled in 2020, only six were conducted. Of 10 such programmes scheduled for the private health sector free-of-charge in 2020, only two were conducted. The External Competency Assessments for malaria microscopy conducted within the WHO Southeast Asia Regional Office’s validation programme had to be postponed to 2021. Several of the training programmes conducted in 2020 were carried out as distance-programmes online. Routine supervisory visits by AMC and RMO staff to the various hospitals and field sites throughout 2020 were cancelled owing to travel restrictions.
A new event—a simulation exercise on malaria outbreak response—was carried out for staff in 2020 by the AMC in collaboration with the Disaster Management Unit of the Ministry of Health. The event was held in a venue in a previously malaria endemic district which was not, at the time, affected by COVID-19.
To ensure that malaria is not a forgotten disease, particularly by the medical profession, several advocacy events are conducted every year as part of AMC’s communications programmes. These include visits to Government hospitals in the provinces, making presentations at clinical meetings, and events organized by the Medical Associations. These activities were minimized in 2020. Instead, tele-messaging using Short Message Service through a telecommunications network, was increasingly used as a means of communication with clinicians.
Communication groups were created using internet-based messaging apps, such as WhatsApp, to exchange vital information on most activities in real time among AMC headquarters staff and RMOs, including members of the Technical Support Group (a group of independent experts advising the AMC) [17]. Monthly review meetings of the AMC with all RMOs and meetings of the Case Review Committee (a group of experts that reviews all malaria cases diagnosed by the AMC in the previous month) were conducted without interruption using cloud-based video conferencing systems.
During country- and district-level lockdowns, the AMC had to work with less than the full cadre of staff because travel was restricted. A roster system was introduced for staff, providing transport for them to come to work and to carry out field work. Staff were provided with personal protective equipment as appropriate, and all work was carried out according to the COVID-19 control guidelines provided by the Ministry of Health [18, 19].
AMC developed interim guidelines for surveillance operations in 2020 in accordance with preventive and precautionary measures for COVID-19 and consistent with the country’s COVID-19 control guidelines [16, 20, 21]. When working conditions became very restricted, such as during the months of April and May when the entire country was in lockdown, the AMC prioritized essential work and ensured that commodities—medicines, diagnostics and vector control supplies—were provided to all districts and service delivery points.
Intersectoral co-ordination for malaria surveillance
With the onset of the COVID-19 epidemic in 2020, the malaria PoR programme was conducted with even stronger links to its inter-sectoral collaborators than in previous years [22]. The Sri Lanka Army, Airforce and Navy were in charge of implementing several components of the COVID-19 control programme, from the arrival of travelers into the country and their screening for COVID-19 to quarantining [19, 23]. The AMC rapidly sought synergies with the military’s work and with the Airports and Aviation Services for screening and follow up of people arriving from malaria endemic countries in a seamless manner.
Budgetary implications and procurement of commodities
The approved budget allocations for the AMC Headquarters were not changed during the course of 2020. Utilization of funds was reduced initially, but over the entire year budget utilization increased compared to the previous year. This was due to funds being transferred to regions (districts) to implement activities in the latter part of 2020.
Although the ease and speed of procurement of commodities and supplies was severely affected during the pandemic, the delays did not affect the AMC very much because it had buffer stocks of almost all commodities—antimalarial medicines, rapid diagnostic tests, reagents for microscopy and chemical insecticides—to last through the pandemic. When stocks of the rarely-used second-line medicine (dihydroartemisinin–piperaquine) were running low, the small quantity required was sent by WHO. During the period of the study, and throughout the pandemic, the malaria PoR programme experienced no stockouts.
Discussion
Commonalities between malaria and COVID-19 control programmes
For Sri Lanka, malaria and COVID-19 share some important features: both are febrile diseases with overseas travel as a major risk factor. Whilst the source of malaria in Sri Lanka today is entirely overseas, COVID-19 started out as imported infections before local transmission was established. Yet, importation remained as a very important factor for introducing different, possibly more virulent variants of the virus. Therefore, both malaria and COVID-19 required surveillance of persons arriving from overseas. Thirdly, a key strategy for the control of both diseases was active case surveillance and contact screening. Fourthly, programmes for the control of both diseases were heavily dependent on strong inter-sectoral cooperation and collaboration involving several sectors beyond health. The AMC was quick to identify these common and overlapping areas of intervention and sought synergies with the control of the COVID-19 epidemic in order to effectively deal with malaria PoR amidst the disruptions caused by the former.
Adaptation and innovation within the PoR programme
The success of the malaria PoR programme rests on rigorous surveillance—both case and entomological surveillance—and rapid response as principal components of the strategy [24]. Due to the COVID-19 pandemic and its consequences, some aspects of the malaria PoR action plans which were being rigorously implemented by the AMC had to be either scaled down, modified or even abandoned (Table 3). The COVID-19 pandemic also led the AMC to introduce and adopt several new and innovative strategies, mechanisms and activities to face the new realities whilst keeping the country free of malaria transmission.
On the one hand, arrivals to the country, which were the only sources of malaria infections to Sri Lanka, were reduced by 78% in 2020 compared to the average over the previous 3 years. Yet, case surveillance was not only maintained but further strengthened compared to previous years. The AMC took advantage of the fact that passenger arrivals through airports were greatly controlled, and that there was a policy of testing for COVID-19 on arrival and mandatory quarantine for 14 days thereafter. These procedures provided the AMC with a ‘captive’ population at risk, which could be more easily screened for malaria through PACD at quarantine centers. In contrast, in previous years, the AMC could proactively screen only a very small proportion of those arriving in the country from malaria endemic parts of the world, mostly military groups returning from UN Peacekeeping Missions.
Apart from these groups, prior to 2020, most arrivals from malaria endemic countries could move freely in the community anywhere in the country until they developed symptoms of malaria and sought healthcare on their own. Therefore, whilst the PCD surveillance strategy detected most (89–100%) imported malaria infections in previous years [8], in 2020, PCD detected only 63% of malaria infections reported. In contrast, the proportion of malaria cases detected by PACD increased significantly, from 0 to 1.9% in previous years to 33% in 2020.
RACD was conducted in relation to every case of malaria detected as in previous years [3, 4]. The total number of blood samples examined for malaria in 2020 was just over half (56%) of the average number screened during the past 3 years. Rather than attributing this reduction to a compromised case surveillance programme, it is postulated that this was because there were fewer people at risk of malaria; fewer arrivals from overseas owing to travel restrictions; and screening being more targeted to capture high-risk groups in quarantine centres which was able to capture the cases before they presented in the community, thus, requiring less screening for malaria in the community.
Overall, the shift in case detection yields from different strategies is a testament to the AMC’s agile and responsive PoR programme, which was quick to change strategy and its modus operandi soon after the COVID-19 epidemic began.
On the other hand, by severely restricting human movement and activity owing to lockdowns and on account of individual safety concerns, the COVID-19 pandemic made several of the routine activities of the PoR programme difficult to perform (Table 3). Some were reduced in frequency, and others were cancelled, but in their place innovative new mechanisms were adopted. The AMC was quick to switch to electronic means of communication amongst its network of staff island-wide. Besides, several new ways of operating—such as depending on online platforms for data sharing and using internet-based communication apps—continued throughout the year and beyond and may have contributed to greater efficiency by reducing travel time of staff. These new and possibly more cost-effective ways of working prompted by the COVID-19 pandemic may have even greater potential in the future with development of adequate technological capacity.
Essential malaria PoR activities were sustained despite the COVID-19 pandemic whilst strictly conforming to the Government’s COVID-19 control measures and guidelines. Even the Mid-Term External Review of the AMC was conducted as scheduled by a group of experts in Sri Lanka led by a foreign expert using online communication methods. What was mostly compromised, particularly during the lockdown periods, were supervisory visits by staff to districts and provinces and in-person training programmes such as those for microscopy. This may have led to deterioration in the quality of services.
Intersectoral collaboration: a critical component of both COVID-19 and malaria PoR
Already well-established intersectoral collaborations of the AMC which functioned well during and after malaria elimination [22] served the programme extremely well during the COVID-19 pandemic. Over the years, the AMC had established strong alliances and worked closely with many sectors beyond health, namely, (1) the Ministry of Defence (Sri Lanka Army, Air Force and Navy) and the Police Department, on account of their members being at high risk of importing malaria on their return from UN Peacekeeping Missions [25,26,27,28]; (2) the Airports and Aviation Ministry, for granting permission for the AMC staff to carry out activities related to malaria surveillance on arriving passengers [29]; and (3) the International Organization for Migration, which repatriates Sri Lankan nationals from India [30]. In 2020, rapid connections were re-established to screen passengers arriving from overseas for malaria at quarantine centers in complete synchrony with the testing programme for COVID-19. This entailed a high degree of coordinated efforts between the AMC, the aforementioned sectors, and Provincial authorities within the Ministry of Health as quarantine centers were located throughout the country [8]. This experience highlights the need for agility and flexibility, and rapidity in the response of health programmes as a key component of health security.
Public health component of the health system
Staff of the malaria PoR programme were not reassigned to control COVID-19 to a significant degree; thus, human resources for malaria were not compromised by the pandemic. The country rapidly deployed cadres of public health personnel to the field, from the Medical Officers of Health to the Public Health Inspectors, and called in the defence forces and the Police Department to implement a stringent COVID-19 control programme. This illustrates yet another important feature for health security, which is to have an adequately staffed public health programme operating at the most peripheral levels of the health system, which can be rapidly deployed in health emergencies without compromising the activities of other specialized programmes.
Several senior public health officials who directed the COVID-19 control programmes when interviewed stated that they had worked in malaria endemic provinces and districts in the 1980s and 1990s and that their prior experience of malaria control served them well in planning and executing the COVID-19 response [30]. When malaria was endemic in the country, the principles used in its control were much the same as those underlying the control of the COVID-19 epidemic: screening high-risk populations, isolating/treating positives, investigating cases to locate the source of transmission, and tracing and screening of contacts. This emphasizes the point that public health cadres proficient in principles and practices of infectious disease control will be an essential component of health security systems that are equipped to respond to future pandemics.
Leadership within the AMC emerged as a critically important factor during 2020, which served as a stress test for an otherwise well run and effective malaria PoR programme. A highly motivated leadership, which inspired dedication and a high work ethic amongst the staff and those in the district malaria offices, was perhaps one of the key factors which led to uninterrupted and successful PoR activities.
Entomological surveillance operations constitute an important component of the PoR programme because the country is highly receptive to malaria due to the high prevalence of vector mosquitoes. This component was placed under stress because it entails extensive fieldwork and is difficult to perform when human movement is highly restricted. Yet, it appears that sufficient entomological surveillance and vector control operations were carried out, albeit more effectively targeted to risk-areas around quarantine centers, to keep the country free of malaria transmission despite many situations which could have led to the resumption of malaria transmission and the re-establishment of the disease.
This raises an important issue, which is often overlooked in health systems that are overly bureaucratic: prioritization of leadership training and development for health professionals. The AMC’s experience in the post-elimination period in Sri Lanka also highlights the importance of maintaining a national malaria programme with dedicated staff and clear mandates, even if it has to operate through a decentralized and integrated health system in the districts. Had there been no equivalent of an AMC in the country, the malaria outcomes during the COVID-19 epidemic might have been quite different, with the general health system under pressure to deviate its resources and attention to COVID-19 control at the peril of other communicable diseases such as malaria. The lesson for malaria endemic countries, many of which are nearing elimination, is the importance of sustaining a lean but dedicated programme for malaria to prevent re-establishment even if implementation of interventions must be integrated within the health system. The risk of fully integrating malaria services into the general health system too early without maintaining dedicated malaria leadership and expertise must be recognized when planning for health security.
Prioritizing current threats vs preserving gains achieved
This collective experience begs the question as to whether Sri Lanka’s malaria PoR programme, which successfully kept the country malaria-free during the COVID-19 pandemic, was justified during an unexpected and serious health crisis. Indeed, many routine health delivery systems, such as those for non-communicable diseases, were seriously disrupted when the country was locked down and human movement was severely restricted. On balance, it appears that the malaria PoR programme was not sustained at the expense of any COVID-19 control interventions; there were adequate public health staff to implement both programmes. The important public health lesson here was the leadership, adaptation, and innovation on the part of the malaria PoR programme in aligning its implementation plans with those of the COVID-19 programme, and taking advantage of the synergies between the two programmes so that both could be successful.
Furthermore, there are many instances of the COVID-19 pandemic negatively affecting malaria control programme in South-East Asia [31]. For example, despite reporting zero indigenous malaria cases since 2017, Timor Leste experienced a localized outbreak of malaria in 2020 due to COVID-19 pandemic disruptions and had to defer planned request of WHO malaria-free certification [31]. Given that Sri Lanka nearly achieved near elimination in 1963 before programme disruptions caused a major resurgence, the public health importance of successfully maintaining PoR while effectively managing the COVID-19 pandemic cannot be overstated.
Conclusion
The COVID-19 pandemic struck an ill-prepared world of public health with alarming suddenness. It demanded rapid responses, swift changes and innovation on a scale that had not been experienced by the current generation of health professionals and planners. Sri Lanka’s AMC innovatively made use of the synergies between COVID-19 and the prevention of re-establishment of malaria, recognizing both as health security threats, and took advantage of strong inter-sectoral collaboration to sustain and even maximize the effectiveness of the malaria PoR programme during the pandemic. The experiences of Sri Lanka’s malaria PoR programme in keeping the country free of malaria during the pandemic highlight several important aspects of health security which are increasingly relevant in a world likely to face similar health challenges in the future.
Availability of data and materials
All data used for analyses are presented in the manuscript.
Abbreviations
- AMC:
-
Anti Malaria Campaign
- COVID-19:
-
Coronavirus disease 2019
- PACD:
-
Proactive case detection
- PCD:
-
Passive case detection
- PoR:
-
Prevention of reestablishment
- RACD:
-
Reactive case detection
- RMO:
-
Regional Malaria Officer
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- WHO:
-
World Health Organization
References
Senaratne R, Singh PK. Against the odds, Sri Lanka eliminates malaria. Lancet. 2016;388:1038–9.
Dharmawardena P, Premaratne R, Wickremasinghe R, Mendis K, Fernando D. Epidemiological profile of imported malaria cases in the prevention of reestablishment phase in Sri Lanka. Pathog Glob Health. 2022;116:38–46.
Karunasena VM, Marasinghe M, Koo C, Amarasinghe S, Senaratne AS, Hasantha R, et al. The first introduced malaria case reported from Sri Lanka after elimination: implications for preventing the re-introduction of malaria in recently eliminated countries. Malar J. 2019;18:210.
Chulasiri P, Ranaweera P, Sudarshan P, Jayasinghe M, Harishchandra J, Gunasekera K, et al. Transfusion-induced Plasmodium falciparum malaria in a beta thalassaemia patient during the prevention of re-establishment phase in Sri Lanka. Malar J. 2021;20:352.
Perera R, Wickremasinghe R, Newby G, Caldera A, Fernando D, Mendis K. Malaria control, elimination, and prevention as components of health security: a review. Am J Trop Med Hyg. 2022;107:747–53.
Malik SM, Barlow A, Johnson B. Reconceptualising health security in post-COVID-19 world. BMJ Glob Health. 2021;6: e006520.
Ranaweera P, Wickremasinghe R, Mendis K. Preventing the re-establishment of malaria in Sri Lanka amidst the COVID-19 pandemic. Malar J. 2020;19:386.
Gunasekera WMKTDAW, Premaratne R, Fernando D, Munaz M, Piyasena MGY, Perera D, et al. A comparative analysis of the outcome of malaria case surveillance strategies in Sri Lanka in the prevention of re-establishment phase. Malar J. 2021;20:80.
Anti Malaria Campaign. Guidelines for entomological surveillance for malaria in PoR phase-2019. Anti Malaria Campaign, Sri Lanka; 2019. http://amc.health.gov.lk/images/PublicNotice-Repository/Ento_surveillance_guide_2019.pdf.
Epidemiology Unit, Ministry of Health. COVID-19 epidemiology. https://www.epid.gov.lk/storage/post/pdfs/en_6401f018ecba5_esummary-may.pdf.
Wickremasinghe AR, Kumari Ariyasena AD, Munasinghe TU, Perera R. Disability-adjusted life years due to COVID-19 in Sri Lanka: a retrospective cross-sectional study. BMJ Public Health. 2023;1: e000055.
Examplars in global health. How did Sri Lanka respond to the COVID-19 pandemic. https://www.exemplars.health/emerging-topics/ecr/sri-lanka/how-did-sri-lanka-respond#:~:text=34,Lockdowns,essential%20workers%20to%20stay%20home.
Ariyawardana SSN. Post COVID-19 tourism resumes with “Travel Bubble”: a study on the preparation of the hotels and restaurants in Nuwara Eliya, Sri Lanka. J Tour Sports Manag. 2021;4:611–21.
Ministry of Health, Nutrition and Indigenous Medicine. Guidelines of malaria chemotherapy and management of patients with malaria. 2014. http://amc.health.gov.lk/Circulars/Treatment-guidelines_Malaria.pdf.
Anti Malaria Campaign. Scope of work to be performed when a malaria patient is reported. 2016. http://www.malariacampaign.gov.lk/images/Publication%20Repository/SOP/SCOPE_OF_WORK_TO_BE.pdf.
Anti Malaria Campaign. Interim recommendations for malaria entomological surveillance and vector control during COVID-19 pandemic. Sri Lanka; 2020. http://www.malariacampaign.gov.lk/images/PublicNotice-Repository/interim_recommendations_for_malaria_entomological_surveillance_and_vector_control_during.pdf.
Datta R, Mendis K, Wikremasinghe R, Premaratne R, Fernando D, Parry J, et al. Role of a dedicated support group in retaining malaria-free status of Sri Lanka. J Vector Borne Dis. 2019;56:66.
Ministry of Health. Provisional clinical practice guidelines on COVID-19 suspected and confirmed patients. Sri Lanka; 2020. https://shri.lk/wp-content/uploads/2020/10/covid-19_cpg_version_5-1.pdf.
Wickramasinghe D, Fernando VK. Sri Lanka’s fight against COVID-19: a brief overview. In: Pandemic risk, response, and resilience. Amsterdam: Elsevier; 2022. p. 129–42. https://doi.org/10.1016/B978-0-323-99277-0.00031-0.
Anti Malaria Campaign. Interim guidelines on parasitological surveillance for malaria during the COVID-19 pandemic. Anti Malaria Campaign, Sri Lanka; 2020. http://www.malariacampaign.gov.lk/images/PublicNotice-Repository/Interim_Guidelines_on_Parasitological_Surveillance_for_malaria_during_the_COVID-19_Pandemic.pdf.
Anti Malaria Campaign. Interim guidelines for malaria prevention activities in COVID-19 quarantine centres. Sri Lanka; 2020. http://www.malariacampaign.gov.lk/images/PublicNotice-Repository/Interim_guideline_for_Malaria_Prevention_in_COVID_19_Quarantine_Centres_2020.pdf.
Ministry of Health, Nutrition & Indigenous Medicine. Malaria elimination in Sri Lanka national report for WHO certification. Sri Lanka; 2016.
Jayasena H, Chinthaka W. COVID-19 and developing countries: lessons learnt from the Sri Lankan experience. J R Soc Med. 2020;113:464–5. https://doi.org/10.1177/0141076820947367.
Premaratne R, Ortega L, Janakan N, Mendis K. Malaria elimination in Sri Lanka: what it would take to reach the goal. WHO South-East Asia J Public Health. 2014;3:85.
Karunaratna S, Ranaweera D, Vitharana H, Ranaweera P, Mendis K, Fernando D. Thrombocytopenia in malaria: a red-herring for dengue, delaying the diagnosis of imported malaria. J Glob Infect Dis. 2021;13:172.
Fernando SD, Dharmawardana P, Semege S, Epasinghe G, Senanayake N, Rodrigo C, et al. The risk of imported malaria in security forces personnel returning from overseas missions in the context of prevention of re-introduction of malaria to Sri Lanka. Malar J. 2016;15:144.
Fernando SD, Booso R, Dharmawardena P, Harintheran A, Raviraj K, Rodrigo C, et al. The need for preventive and curative services for malaria when the military is deployed in endemic overseas territories: a case study and lessons learned. Milit Med Res. 2017;4:19.
Fernando SD, Ranaweera D, Weerasena MS, Booso R, Wickramasekara T, Madurapperuma CP, et al. Success of malaria chemoprophylaxis for outbound civil and military travellers in prevention of reintroduction of malaria in Sri Lanka. Int Health. 2020;12:332–8.
Fernando D, Thota P, Semege S, Booso R, Bell D, Gunasekera KTDAW, et al. Evaluation of a haemozoin-based rapid diagnostic test for diagnosis of imported malaria during the phase of prevention of reestablishment in Sri Lanka. Malar J. 2022;21:263.
Caldera A, Wickremasinghe R, Newby G, Perera R, Mendis K, Fernando D. Initial response to SARS-CoV-2 (COVID-19) outbreak in Sri Lanka; views of public health specialists through an international health regulations lens. PLoS ONE. 2023;18: e0293521.
Wangmo LD, Freitas Belo OM, Penjor K, Drukpa T, de Fatima Mota MR, Viegas OS, et al. Sustaining progress towards malaria elimination by 2025: lessons from Bhutan & Timor-Leste. Lancet Reg Health West Pac. 2022;22: 100429.
Acknowledgements
The authors wish to acknowledge the Regional Malaria Officers of all the districts for collecting and sharing the data required for this study. The authors also wish to thank Dr. Saveen Semage, Consultant Community Physician, formerly of Directorate of Army Preventive Medicine & Mental Health Services who assisted in obtaining information on quarantine centres.
Funding
We acknowledge the financial assistance provided by the Bill & Melinda Gates Foundation, through a grant to the Malaria Elimination Initiative at the University of California, San Francisco (OPP1160129). The funders had no role in study design, data collection or analysis, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
KM, DK, and RW were involved in the conceptualization and analysis. PR, KG, TF, RP and AC were involved in data curation. Funding was secured by GN and RW. Writing original draft, review and editing were done by KM, DF, RW, PR, KG, TF, GN, RP, and AC.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Review Committee of the Faculty of Medicine, University of Kelaniya, Sri Lanka (Ref. No. P/201/12/2021).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mendis, K., Fernando, D., Ranaweera, P. et al. Preventing the re-establishment of malaria during the COVID-19 pandemic in Sri Lanka: implications for health security. Malar J 23, 254 (2024). https://doi.org/10.1186/s12936-024-05080-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-05080-0