Abstract
Background
Malaria remains a burden globally, with the African region accounting for 94% of the overall disease burden and deaths in 2019. It is the major cause of morbidity and mortality among children in Nigeria. Though different environmental factors have been assessed to influence the distribution and transmission of malaria vectors, there is a shortage of information on how they may influence malaria transmission among under-fives in Nigeria.
Methods
This study was based on the secondary data analysis of the Nigeria Malaria Indicator Survey 2021. The study sample comprised 10,645 women (aged 15–49) who delivered a child in the 2 years preceding the survey. The study was restricted to under-fives. Logistic regression was used to identify factors associated with the risk of malaria.
Results
There was a positive association between the risk of malaria and heard/seen malaria messages in the last 6 months (AOR 1.39, 95% CI 1.19–1.62), houses with walls built using rudimentary materials (AOR = 1.38, 95% CI 1.04–1.83), at least 6 children living in the house (AOR 1.22, 95% CI 1.00–1.49), children being 1 or 2 years old was associated with increased odds (AOR 1.89, 95% CI 1.50–2.34 and AOR 1.89, 95% CI 1.52–2.36), children from households with only treated nets (AOR 1.23, 95% CI 1.04–1.46) and those from the North West or South East regions (AOR 1.50, 95% CI 1.10–2.05 and AOR 1.48, 95% CI 1.01–2.16), respectively. All other predictors were not associated with the risk of malaria.
Conclusion
The factors associated with the risk of malaria in this study included sleeping under treated mosquito nets, the age of the children, residing in the northwest and southeast regions, wall construction material, 6 children and above in the household and hearing/seen malaria messages in the last 6 months. Continuous health education and public health interventions, such as the provision of LLITNs, will reduce the risk of malaria and improve the health and well-being of children under 5 years of age.
Similar content being viewed by others
Background
Malaria has been a serious global public health problem for several decades, especially in Africa and other endemic regions [1,2,3]. It is a fatal disease that is preventable and treatable and is transmitted to humans by female Anopheles mosquitoes [4, 5]. Malaria is an infectious disease caused by 5 protozoan species, namely; Plasmodium falciparum, Plasmodium malariae, Plasmodium vivax, Plasmodium ovale, and Plasmodium knowlesi. Among these species, P. falciparum is the most lethal pathogen and is found mostly in sub-Saharan Africa (SSA) [2, 3, 6, 7]. Generally, severe outcomes of malaria in children could result in seizures and coma, anaemia due to repeated infection and low birth weight during pregnancy, increasing the risk of death in the first month of life [8].
Malaria has continued to be the foremost cause of morbidity and mortality in children under 5 years old in sub-Saharan Africa [9, 10]. In 2022, globally, there were 249 million cases of malaria with 75% being children under 5 years of age [8]. Under-five children are more vulnerable to malaria infection than adults due to their lower immunity, thereby making them more susceptible to severe malaria due to repeated malaria infections [7]. A study in Nigeria showed that age, mosquito bed net usage, availability of health infrastructure, source of drinking water, distance to waste disposal points and window protection were significant determinants of malaria infection in children under 5 years of age [7, 11].
In 2020, 95% of all malaria cases and 96% of malaria deaths were reported in the African region with 80% of these deaths reported in children younger than 5 years. 6 sub-Saharan African countries, namely Nigeria (27%), the Democratic Republic of Congo (12%), Uganda (5%), Mozambique (4%), Angola (3.4%), and Burkina Faso (3.4%), bore 55% of the global malaria burden [12].
Nigeria has a high incidence of malaria mortality in children under 5 years, which is largely attributable to a health financing system that ignores uninsured individuals. This results in high out-of-pocket (OOP) medical expenditures that discourage healthcare-seeking behaviour, especially among these individuals [13]. The percentage of out-of-pocket expenditure medical expenditure in Nigeria in 2021 was 76% compared to 66% in 2005 [14]. The rate of care-seeking for suspected cases of malaria in Nigeria is among the lowest globally, as just under 20% of all children under 5 years with fever are taken for clinical consultation and parasitological testing in health facilities [13]. According to the Malaria Indicator Survey (MIS) 2021 in Nigeria, 22% of children tested positive for malaria parasites within 6–59 months according to microscopy results [15].
In the last two decades, many policies and interventions have been implemented to control malaria at the global and regional levels, which have resulted in a significant reduction in malaria-related morbidity and mortality [2]. The WHO Global Technical Strategy for Malaria 2016–2030 (GTS), the complementing Roll Back Malaria (RBM), and the Action and Investment to Defeat Malaria 2016–2030 (AIM) are notable malaria control initiatives that have been put into place in Nigeria and other malaria-endemic countries [16]. By 2030, they hope to eradicate malaria in 35 countries, decrease malaria mortality and case incidence by 90%, and stop the reintroduction of the disease into previously malaria-free areas [16].
However, despite these remarkable successes, there is still a high disease burden and mortality among children under 5 years of age [17]. This study aimed to identify the factors associated with the risk of malaria and to determine the predictors of malaria among children under 5 years in Nigeria.
Methods
Study setting and design
Nigeria is a country located in the western part of sub-Saharan Africa. The country is composed of 36 geopolitical regions, which include 36 states and one federal capital territory [18]. The country is divided into North Central, Northeast, Northwest, Southeast, South and Southwest regions, each with several states. Nigeria is neighboured by Benin to the west, Chad and Cameroon to the east, Niger to the north and the Gulf of Guinea of the Atlantic Ocean to the south.
The 2021 Nigeria Malaria Survey Indicator (2021NMIS) was constructed by the National Malaria Elimination Programme assisted by the National Bureau of Statistics (NBS) and National Population Commission (NPC) was implemented by the Global Fund to Fight AIDS, TB and Malaria (GFATM) [18]. The data were collected from 13/10/2021 to 4/12/2021.
The Nigeria Malaria Indicator Survey (MIS) data were collected in urban and rural areas from all 36 states, and the Federal Capital Territory (FCT) Nigeria is one of the tropical countries in West Africa and has the highest incidence of malaria in sub-Saharan Africa [18]. This study analysed data from the Nigeria Malaria Indicator Survey (NMIS) 2021, a nationally representative cross-sectional survey.
Sampling and participants
The 2021 NMIS is the third malaria indicator survey conducted in Nigeria, with the first occurring in 2010 and the second occurring in 2015. The 2021 survey is unique in three ways. First, it was conducted in the first year of implementation of the current national malaria strategic plan.
A two-stage sampling strategy was adopted for the 2021 NMIS. In the first stage, 568 enumeration areas (EAs) were selected with a probability proportional to the EA size. The EA size is the number of households residing in the EA. The sample was selected in such a way that the sample was representative of each state. A total of 568 clusters were detected throughout the country, 195 in urban areas and 373 in rural areas. A complete listing of households in these clusters was (Additional file 1) conducted between 26 August and 18 September 2021, with the resulting lists of households serving as the sampling frame for the selection of households in the second stage. GPS dongles (global positioning system devices) were used to capture coordinates during household listing in the 2021 NMIS sample clusters. In the second stage of the selection process, 25 households were selected in each cluster via equal probability systematic sampling [18]. For the 2021 NMIS computer-assisted personal interviewing (CAPI) was used for data collection.
The study included women (15–49) years; each respondent provided informed consent to participate in the survey and understood the liberty of opting out any time she wished [18].
Description of variables
The outcome variable was malaria status in a child, which was generated from the H71 (the respondent was told by the health work that the child had malaria) variable in the Women’s Health Questionnaire. Malaria was coded “has malaria” if the respondent was told that the child had malaria and “no malaria” if the respondent was told that the child had no malaria.
The Independent/predictor variables included socio-demographic characteristics namely house floor material, house wall material, roofing material of the house, mother’s age group, the main source of drinking water, mother’s number of living children, type of mosquito net in the household, sex of child, child age in years, type of place of residence, mother’s education”, combined wealth index.
Results
Characteristics of participants
A total of 10,645 under-five children were included in this analysis (Table 1). The majority were from households with improved sources of drinking water (71.93%), finished roofing (83.17%), finished walls (59.15%) and situated in rural areas (69.98%). More than half of the under-5 children did not have a mosquito net (56.92%) and were from the northern region (66.16%). This study included slightly more boys (51.24%) than girls (48.76%). Most mothers of these children had a maximum of 5 living children (81.32%), were between 25 and 34 years old (51.48%), and did not have access to the Internet the previous month (83.25%). Additionally, more than half of the young children under 5 years old were with mothers who had not received any malaria messages in the last 6 months (56.24%). Yet, most of these children were with mothers who had completed at least primary education (57.54%). The majority of the children under 5 years old were at least 2 years of age (61.33%). In most households, there were at most three under-five children (85.03%) and most of these children belonged to households with a mosquito net (63.57%).
Malaria risk according to sociodemographic factors among children under 5 years of age
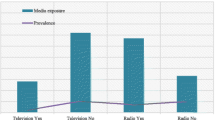
From Table 1, the overall weighted percentage of contracting malaria was 16.57% among children aged 5 years of age. Remarkable differences were observed according to socio-demographic characteristics. The risk of contracting malaria was higher in rural areas (17.71%) than in urban areas (13.66%). This scenario was most risky in “Northwest” (21.57%), “South East” (17.69%), “North East” (16.32%), “North Central” (12.91%), “South-South” (12.53%) and least risky in “South West” (9.05%). The risk of malaria is higher among those whose mothers have no education (18.14%) or have completed only primary education (19.23%), compared to those whose mothers have attained at least secondary education (13.66%). The analysis also reveals the risk of malaria among children aged under five decreases with increase in women’s age group from those aged “15–24” (17.18%), “25–34” (16.89%), to “35–49” (15.33%). Households that reported others (24.84%) and open source (19.4%) as sources of drinking water were significantly associated with high malaria risk among children aged under five compared to those who reported Improved source (15.52%). Children aged 2 years and below are significantly associated with a high risk of malaria (50.85%) compared to those who are at least 3 years of age (32.07%). The study also shows highly significant malaria risk cases among those whose mothers did not use the Internet at all last month (17.06%) compared to those whose mothers reported “less than once a week” (10.96%), “at least once a week” (15.82%) and “almost every day” (13.55%), respectively. Households with at least 6 living children were significantly associated with high malaria risk (20.09%) compared to those that had “1–5” (15.68%) children in number. Additionally, chi-square tests showed that association between malaria risk and covariates heard/seen malaria messages in the last 6 months, mother’s education, main source of drinking water, having mosquito bed net for sleeping in household, floor material, wall material, frequency of using internet last month, number of living children, child age in years, type of mosquito net, region, combined wealth index and type of place of residence was statistically significant.
Factors associated with malaria risk among children under 5 years of age
Results of the bivariate analysis are detailed in Table 2 with factors individually associated with malaria risk highlighted. In the final multiple logistic regression model, the factors found significantly associated with malaria risk were; heard/seen malaria messages in the last 6 months, wall material, number of living children, child age in years, type of mosquito net, and region. Children whose mothers received malaria messages in the last 6 months (AOR 1.39, 95% CI 1.19–1.62) were more likely to face malaria risk compared to those whose mothers did not receive such messages during that time. Those living in homes with rudimentary walls (AOR = 1.38, 95% CI 1.04–1.83) had higher odds of succumbing to malaria risk compared to those in homes with natural walls. Additionally, children of mothers with at least 6 living children (AOR 1.22, 95%CI 1.00–1.49) were more likely to face malaria risk than those with 1–5 living children. Being 1 or 2 years old was associated with increased odds (AOR 1.89, 95% CI 1.50–2.34 and AOR 1.89, 95% CI 1.52–2.36) of malaria risk compared to being newborn (0 years old). Moreover, children from households with only treated nets (AOR 1.23, 95% CI 1.04–1.46) and those from the North West or South East regions (AOR 1.50, 95% CI 1.10–2.05 and AOR 1.48, 95% CI 1.01–2.16) had higher odds of facing malaria risk compared to their counterparts from the North-central region.
Discussion
This study identified factors associated with the risk of malaria among children under 5years of age. Children whose mothers had been exposed to malaria messaging within 6 months before the study showed a heightened risk of contracting malaria compared to those whose mothers hadn’t received such information. This paradox highlights the complex interplay between information dissemination, health literacy, and disease prevention. While access to information is crucial for empowering parents to protect their children from malaria, this study suggests that the timing or content of the message may have unintended consequences.
Additionally, the study revealed a correlation between housing quality and malaria risk among children. Those residing in homes with rudimentary wall materials faced elevated risks compared to those in dwellings with natural materials, emphasizing the critical role of housing standards in disease transmission, particularly for malaria. This finding echoes similar observations from studies conducted in Uganda, emphasizing the broader implications for malaria control strategies [14]. Improving housing conditions not only addresses individual health but also contributes to broader public health objectives by reducing malaria transmission rates within communities.
Furthermore, the study identified an unexpected association between malaria risk and the use of treated mosquito nets. Contrary to expectations based on previous studies demonstrating significant protection conferred by insecticide-treated nets (ITNs), children who exclusively used treated nets showed higher chances of malaria infection [19]. This suggests a potential over-reliance on ITNs as the sole preventive measure, neglecting other malaria prevention strategies. It underscores the importance of comprehensive malaria prevention education, emphasizing the complementary nature of various preventive measures. Targeted efforts to educate the public on adopting multi-pronged approaches to malaria prevention are crucial for maximizing the effectiveness of interventions and reducing the malaria burden in vulnerable populations.
This study further unveils additional factors intertwined with the risk of malaria, providing crucial insights with significant public health implications. Among these factors are the number of living children in a household and the age of the child. Households with 6 or more living children were found to have an increased risk of malaria compared to those with one to 5 children. This finding underscores the intricate relationship between family size, household dynamics, and malaria transmission [20]. Larger families may experience heightened population density and overcrowding, potentially leading to challenges in implementing effective malaria control measures. The strain on basic amenities in such households could contribute to environmental neglect, creating more breeding grounds for mosquitoes and amplifying the risk of malaria transmission. This highlights the importance of tailored interventions addressing the specific needs of larger families, including enhanced access to and compliance with malaria prevention measures. This increased risk associated with larger families aligns with findings from studies examining the impact of urbanization and population density on childhood Plasmodium falciparum parasite prevalence rates in Africa [20]. The correlation between household size and malaria risk underscores the broader implications of socio-demographic factors in shaping malaria transmission dynamics within communities. Addressing these underlying socio-economic determinants is essential for developing holistic malaria control strategies that effectively target vulnerable populations and reduce transmission rates.
In a contrasting observation, children aged 1 and 2 years were found to have an increased risk of malaria compared to those younger than 1 year old. This phenomenon may be attributed to the possession of immunity acquired from mothers during infancy, as well as the increased care and attention typically given to newborns. However, as children grow older, this acquired immunity wanes, leaving them more susceptible to malaria infection. This highlights the importance of age-specific interventions in malaria control efforts, ensuring that preventive measures are tailored to the unique vulnerabilities and immunity profiles of different age groups.
This study sheds light on a complex of factors influencing malaria risk in children under 5, unveiling both anticipated and surprising associations [14]. While access to information and preventative measures like treated mosquito nets are crucial, their timing, content, and implementation require meticulous approaches to maximize effectiveness. The study underscores the interplay between social, environmental, and demographic factors, emphasizing the need for holistic and multifaceted interventions that address not only individual risk but also underlying socio-economic determinants within communities. Tailored interventions for larger families, age-specific strategies, and comprehensive education fostering multi-pronged approaches are key to reducing the malaria burden and empowering vulnerable populations [19]. This study’s insights, echoing similar observations from broader contexts, pave the way for evolving malaria control strategies that effectively target risk factors and ultimately break the cycle of transmission, safeguarding the health and well-being of children.
Limitations of the study
A two-stage sampling strategy was used during data collection but in our analysis, we didn’t take into consideration the hierarchical levels which could affect the interpretation of our results. The study was purely based on data from children under 5 years hence the findings cannot be used to conclude other groups of children such as children older than 5 years within the Nigerian communities.
Availability of data and materials
The dataset used is openly available upon permission from the MEASURE DHS website. (URL: https://www.dhsprogram.com/data/available-datasets.cfm).
Abbreviations
- GPS:
-
Global positioning system
- COR:
-
Crude odds ratio
- AOR:
-
Adjusted odds ratios
- LLIN:
-
Long-lasting insecticidal nets
- WHO:
-
World Health Organization
- NMIS:
-
Nigeria Malaria Indicator Survey
- CI:
-
Confidence interval
- NMEP:
-
National malaria elimination programme
- DHS:
-
Demographic and Health Survey
- SDSS:
-
Spatial decision support systems
- FMOH:
-
Federal Ministry of Health
- NBS:
-
National Bureau of Statistics
- PMI:
-
Presidential malaria initiative
- GFATM:
-
Global fund to fight AIDS, TB and malaria
- SSA:
-
Sub-Saharan Africa
- FCT:
-
Federal capital territory
- CAPI:
-
Computer-assisted personal interviewing
- NPC:
-
National population commission
- IBR:
-
Institutional Review Board
- USAID:
-
United States agency for international development
- NMSP:
-
National malaria strategic plan
- RBM:
-
Roll back malaria
- RDT:
-
Rapid diagnostic test
- malERA:
-
Malaria eradication research agenda
- AIM:
-
Action and investment to defeat malaria 2016–2030
- ITNs:
-
Insecticide treated nets
References
Ahmed A, Mulatu K, Elfu B. Prevalence of malaria and associated factors among under-5 children in Sherkole refugee camp, Benishangul–Gumuz region Ethiopia. A cross-sectional study. PLoS ONE. 2021;16: e0246895.
Sarfo JO, Amoadu M, Kordorwu PY, Adams AK, Gyan TB, Osman AG, et al. Malaria amongst children under 5 in sub-Saharan Africa: a scoping review of prevalence, risk factors and preventive interventions. Eur J Med Res. 2023;28:80.
Abossie A, Yohanes T, Nedu A, Tafesse W, Damitie M. Prevalence of malaria and associated risk factors among febrile children under 5 years: a cross-sectional study in Arba Minch Zuria district, South Ethiopia. Infect Drug Resist. 2020;13:363–72.
Gaston RT, Ramroop S. Prevalence of and factors associated with malaria in children under 5 years of age in Malawi, using malaria indicator survey data. Heliyon. 2020;6: e03946.
Malaria. Geneva: World Health Organization. 2023. https://www.who.int/news-room/fact-sheets/detail/malaria.
Obasohan PE, Walters SJ, Jacques R, Khatab K. Individual and contextual factors associated with malaria among children 6–59 months in Nigeria: a multilevel mixed-effect logistic model approach. Int J Environ Res Public Health. 2021;18:11234.
Bayode T, Siegmund A. Social determinants of malaria prevalence among children under 5 years: a cross-sectional analysis of Akure, Nigeria. Sci African. 2022;16: e01196.
Roll Back Malaria Partnership. Annual report 2022. Geneva: World health organization; 2023.
Aychiluhm SB, Gelaye KA, Angaw DA, Dagne GA, Tadesse AW, Abera A, et al. Determinants of malaria among children under 5 years of age in Ethiopia: Bayesian multilevel analysis. BMC Public Health. 2020;20:1468.
Ibadin O, Ofili N, Momodu R, Oaikhena E, Oba I. Some economic and sociocultural factors associated with cerebral malaria among under 5 in Benin City, Nigeria. Niger J Paediatr. 2012;39:168–73.
Tsegaye AT, Ayele A, Birhanu S. Prevalence and associated factors of malaria in children under the age of 5 years in Wogera district, northwest Ethiopia: a cross-sectional study. PLoS ONE. 2021;16: e0257944.
Anjorin S, Okolie E, Yaya S. Malaria profile and socioeconomic predictors among children under 5 years: an analysis of 11 sub-Saharan African countries. Malar J. 2023;22:55.
Dasgupta RR, Mao W, Ogbuoji O. Addressing child health inequity through case management of under 5 malaria in Nigeria: an extended cost-effectiveness analysis. Malar J. 2022;21:81.
EdEdeh HC. Exploring dynamics in catastrophic health care expenditure in Nigeria. Health Econ Rev. 2022;12:22.
NPC-NMCP. Malaria Indicator Survey (MIS) 2021. P:1–137.
Morakinyo OM, Balogun FM, Fagbamigbe AF. Housing type and risk of malaria among under 5 children in Nigeria: evidence from the malaria indicator survey. Malar J. 2018;17:311.
Roberts D, Matthews G. Risk factors for malaria in children under the age of 5 years old in Uganda. Malar J. 2016;15:246.
National Malaria Elimination Programme (NMEP) [Nigeria], National Population Commission (NPC) [Nigeria], and ICF 2022. Nigeria Malaria Indicator Survey final report 2021. Abuja, Nigeria, and Rockville: NMEP, NPC, and ICF.
Killeen GF, Smith TA, Ferguson HM, Mshinda H, Abdulla S, Lengeler C, et al. Preventing childhood malaria in Africa by protecting adults from mosquitoes with insecticide-treated nets. PLoS Med. 2007;4: e229.
Kabaria CW, Gilbert M, Noor AM, Snow RW, Linard C. The impact of urbanization and population density on childhood Plasmodium falciparum parasite prevalence rates in Africa. Malar J. 2017;16:49.
Acknowledgements
The 2021 Nigeria Malaria Indicator Survey (2021 NMIS) was implemented by the National Malaria Elimination Programme (NMEP) of the Federal Ministry of Health, Nigeria, in collaboration with the National Population Commission (NPC). The funding for the 2021 NMIS was provided by the United States Agency for International (USAID) and The Global Fund. ICF provided technical assistance through The DHS Program, a USAID-funded project that provides support and technical assistance in the implementation of population and health surveys in countries worldwide.
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
II conceived the idea and drafted the manuscript, II KT and NS performed the analysis, interpreted the results and drafted the subsequent versions of the manuscript. OLN, ENA, AO and BNG wrote the introduction and discussion. AMJ, DKB and all the other authors reviewed and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We sought permission to use the NMIS datasets from the DHS Program website https://www.dhsprogram.com/data/available-datasets.cfm. The Demographic and Health Survey also anonymized all data before making them accessible to the public. The ICF IRB reviewed and approved the 2021 Nigeria Malaria Indicator Survey. The ORC MACRO, ICF Macro, and ICF IRBs complied with the United States Department of Health and Human Services regulations for the protection of human research subjects (45 CFR 46). All participants provided informed verbal consent to participate in the study and for minors, their parents or guardians consented on their behalf.
Competing interests
All the authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Covariates.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Isiko, I., Nyegenye, S., Bett, D.K. et al. Factors associated with the risk of malaria among children: analysis of 2021 Nigeria Malaria Indicator Survey. Malar J 23, 109 (2024). https://doi.org/10.1186/s12936-024-04939-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-04939-6